Cardiovascular diseases (CVD) are one of the leading causes of mortality in the modern world. In 2021, according to the World Health Organization, 17.9 million people worldwide died from these diseases, accounting for about 30% of all deaths. At the same time, 7.4 million people died from coronary heart disease (CHD) and 6.7 million people died as a result of stroke, one of the causes of which is arterial hypertension (AH).
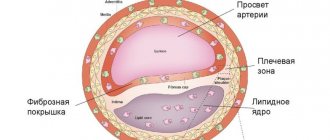
The most dangerous manifestation of IHD is myocardial infarction (necrosis of the heart muscle), which occurs due to blockage of blood vessels supplying the heart by a blood clot. A thrombus forms on the surface of an atherosclerotic plaque, which narrows the lumen of a blood vessel and consists of cholesterol and other compounds of fat, calcium, and connective tissue fibers.
If an atherosclerotic plaque forms in the vessels supplying blood to the brain, there is a risk of thrombosis of the brain vessels and death of part of the brain tissue (ischemic stroke).
What are cardiovascular diseases?
Cardiovascular diseases are a group of diseases of the heart and blood vessels that include:
- coronary heart disease - a disease of the blood vessels that supply blood to the heart muscle;
- cerebrovascular disease - a disease of the blood vessels that supply blood to the brain;
- Peripheral artery disease - disease of the blood vessels that supply blood to the arms and legs;
- rheumatic carditis - damage to the heart muscle and heart valves as a result of a rheumatic attack caused by streptococcal bacteria;
- congenital heart disease – deformations of the structure of the heart existing from birth;
- Deep vein thrombosis and pulmonary embolism - the formation of blood clots in the leg veins that can dislodge and move towards the heart and lungs.
Heart attacks and strokes are usually acute illnesses and occur primarily as a result of blockages in blood vessels that prevent blood from flowing to the heart or brain. The most common cause of this is the formation of fatty deposits on the inner walls of the blood vessels that supply blood to the heart or brain. Bleeding from a blood vessel in the brain or blood clots can also cause a stroke. Myocardial infarction and stroke are usually caused by a combination of risk factors such as tobacco use, unhealthy diet and obesity, physical inactivity and harmful use of alcohol, high blood pressure, diabetes and hyperlipidemia.
Hereditary predisposition
Our body is made up of trillions of cells. Every cell has a nucleus that contains the genetic information that makes you unique. This information is contained in chromosomes. Think of a chromosome as like a ball of wool, and you can stretch it into one long strand called DNA. There are regions of DNA called genes. Each of us has about 20,000 different genes. Since each chromosome has two copies, there are also two copies of each gene (one from each parent).
What is the pattern of inheritance of cardiovascular diseases in families? What is the risk of recurrence of the disease in a family if there is already one patient in it?
Today it is known that hereditary factors are involved in the development of most diseases. From this point of view, diseases of the heart and blood vessels are no exception. Many of them (coronary heart disease, atherosclerosis, hypertension) are multifactorial
.
This means that both environmental factors (for example, ecology) and a person’s lifestyle (for example, the type of diet and amount of physical activity), as well as genetic (hereditary) factors, equally contribute to their formation. However, for children, the most relevant are the so-called monogenic
diseases, for the occurrence of which a mutation (“breakage”) in just one single gene is sufficient. These include, for example, many heart rhythm disorders, such as long QT syndrome (Romano-Ward or Jervell Lange Nielsen syndrome) or short QT syndrome and others. Monogenic heart diseases also include hypertrophic cardiomyopathies.
Gene
(Ancient Greek γένος - genus) is a structural and functional unit of heredity.
A gene is a section of DNA that carries information about the sequence of a specific protein. Genes are located on human chromosomes, each of which is a long DNA molecule. All chromosomes, as well as human genes, are paired: each gene is present in every cell of the body in two copies - one copy on each of the identical (so-called homologous) chromosomes (Fig. 1). Figure 1. DNA, genes and mutations (“breakages”) in genes.
Humans have 23 pairs of chromosomes, 22 of which are called autosomes
and are the same in men and women.
And one pair of chromosomes - the sex chromosomes
- differs between the sexes: in men these are XY chromosomes, and in women they are XX.
In human germ cells there is a half set of chromosomes - not 46, but 23, each chromosome and every gene in the germ cell is present in a single copy. Men have 2 types of germ cells: either with the X chromosome or with the Y chromosome. In women, all germ cells, in addition to 22 autosomes, contain the X chromosome.
Genotype
(genotype, from the Greek genos - genus and typos - imprint, form, sample) - a set of genes of an organism.
In contrast, the totality of all external characteristics of an organism (anatomical, functional, etc.) constitutes a phenotype
.
Hereditary pathology of the cardiovascular system can be either isolated or part of complex genetic syndromes.
Genetic syndrome
– this is a combination in a patient of signs of damage to many organs, united by a common genetic cause.
For example, the rare genetic disorder Marfan syndrome is caused by mutations in the fibrillin 1 (FBN1) gene, affecting multiple organ systems. (Marfan syndrome) includes anomalies (structural features) of the skeletal system in the form of an asthenic physique with long “spider” fingers, a funnel-shaped or keeled chest, anomalies (structural features) of the eyes - in the form of dislocation of the lens with loss of visual acuity and cardiovascular system in in the form of prolapse of heart valves, enlargement of the aortic root and pulmonary artery
.
If a child has a hereditary disease in the family, the question arises about the risk of recurrence of the same disease in future children of these parents. In resolving this issue, a geneticist who provides medical and genetic counseling
couples, during which they collect a family pedigree, examine a family member with the disease, examine family members using genetic tests, and determine the risk of birth of a recurrence of the disease in the family, as well as identify possible options that will avoid the increased risk.
An examination of family members may show that in a sick child, a “breakdown” in a gene arose for the first time in this family (de novo). In this case, the risk of recurrence of the disease in future children of this parental couple is minimal. However, there are families in which the disease occurs in several generations. In these families, pathology is transmitted according to certain patterns that determine the risk of having a child with the disease. It is not possible to consider all possible inheritance options within the framework of this brochure, but we will still analyze the most common types of inheritance in cardiology. Autosomal dominant
diseases appear in people even if only one of the two copies of the gene is “broken.”
Autosomal dominant diseases and traits can be traced through many generations of the vertical pedigree (Figure 2). Figure 2. Pedigree with an autosomal dominant type of inheritance: vertical inheritance of the disease, from a parent of any sex to a descendant of any sex.
Circles are female, squares are male. Designations of family members with the disease are shaded. How to determine genetic risk with autosomal dominant inheritance? Since a family member with the disease has two types of germ cells - with a healthy and a “broken” copy of the gene, the risk of transmitting the disease to his child is 50% (Fig. 3).
Figure 3. Inheritance of dominantly inherited heart disease.
Autosomal dominant inheritance is the most common type of transmission of the disease in families for cardiac diseases.
Autosomal recessive
diseases and symptoms only appear if both copies of the gene are “broken.” Family members who have one copy of the gene “broken” and the other copy healthy do not have clinical manifestations of such a disease, but are carriers of it. In a pedigree, the disease can be traced horizontally in one generation through brothers or sisters (Fig. 4).
In autosomal recessive diseases, it is often possible to identify family ties between parents.
How to calculate genetic risk for autosomal recessive inheritance? Possible combinations of germ cells from parents who are carriers of an autosomal recessive disease (25% of healthy offspring with two healthy copies of the gene, 50% of clinically healthy carriers of one “broken” and one healthy copy of the gene, and 25% of offspring with the disease and two “broken” copies of the gene) lead to a 25% chance of having a sick child.
Figure 4. Pedigree for autosomal recessive inheritance: horizontal inheritance of the disease. A related marriage in a pedigree is depicted by a double solid line connecting the symbols representing the spouses. Sick individuals are shaded. The mother and father of sick children are healthy carriers and have one healthy and one mutant copy of the gene. Each parent passed on a mutant copy of the gene to sick children; the probability of such a simultaneous transfer of a “broken” copy of the gene to the child from both parents is 25%.
Diseases linked to chromosome X
and their nature of inheritance is usually considered separately due to the peculiarities of the manifestation of the disease only in individuals of a certain sex; it is also usually divided into the so-called X-linked recessive and X-linked dominant. Here we look at the most common X-linked recessive inheritance.
Since men have only one X chromosome, all X-linked genes are present in only one copy. Those. their cells do not have a second copy of the gene located on the X chromosome. If the breakdown is located in this single copy of the gene, then in men, there is no second copy of the gene on the X chromosome that could compensate for the lack of function of the single “broken” copy. X-linked recessive diseases therefore appear in boys and are transmitted in the pedigree by healthy female carriers. Female carriers have two X chromosomes - one with a “broken” one, the other with a healthy copy of the X-linked gene. This type of transmission in the pedigree is sometimes called “diagonal” (Fig. 5).
Figure 5. Pedigree for X-linked recessive inheritance: diagonal inheritance of the disease. With this type of inheritance, only men are affected (shaded). The symbol “circle with a dot inside” indicates a female carrier of an X-linked gene mutation. All female carriers of the disease are clinically healthy because they have one healthy copy of the X chromosome gene, which compensates for the work of the second - mutant - copy of the gene. All men have the only chromosome X, and if it carries a mutant copy of the gene, then they are definitely sick. Female carriers pass the disease along with a mutant copy of the X chromosome to their sons with a 50% chance; they also have a 50% chance of passing on a healthy X chromosome to their son.
Genetic risk for X-linked recessive inheritance: if a carrier of an X-linked recessive mutation marries a healthy man, then each of their sons will have a 50% risk of getting the disease, and each daughter will have a 50% chance of being a carrier.
What are the risk factors for cardiovascular disease?
The main risk factors for heart disease and stroke are poor diet, physical inactivity, tobacco use and harmful use of alcohol.
The effects of behavioral risk factors on an individual may include increased blood pressure, increased blood glucose, increased blood lipids, and overweight and obesity. These “intermediate risk factors” can be assessed in primary care settings and may indicate an increased risk of myocardial infarction, stroke, heart failure and other complications.
Quitting tobacco use, reducing salt intake, consuming fruits and vegetables, regular physical activity and avoiding harmful use of alcohol have been shown to reduce the risk of developing cardiovascular disease. In addition, drug therapy may be necessary to reduce the risk of CVD and prevent heart attack and stroke in people with diabetes, high blood pressure, and elevated lipid levels. To increase people's motivation to make and maintain healthy behaviors, health policies are needed to create an enabling environment for healthy choices to be made and afforded to them.
In order for people to choose and maintain healthy behaviors, policies are needed to create an environment conducive to healthy choices, their accessibility and affordability.
There are also a number of factors that influence the development of chronic diseases, or underlying causes. They reflect the main driving forces leading to social, economic and cultural changes - globalization, urbanization and population aging. Other determinants of CVD include poverty, stress and genetic factors.
Dyslipidemia
Numerous studies have established that one of the main reasons for the development of vascular atherosclerosis is a violation of fat or lipid metabolism, namely an increase in the level of cholesterol (C) in the blood. In one long-term study that followed its participants for many years in the United States, it was found that people with cholesterol levels from 6.2 to 6.8 mmol/l had a twice the risk of developing coronary artery disease than people with cholesterol levels below 5.2 mmol/l. If the cholesterol level was above 6.8 mmol/l, then the risk increase was 3-fold.
The main lipids found in human plasma are free fatty acids, triacylglycerides, phospholipids and cholesterol. All lipids are found in the blood in protein-bound form in the form of lipoproteins. Chylomicrons are the largest lipoprotein particles. In addition, there are very low density lipoproteins, low density lipoproteins, lipoproteins (a) - a protein complex rich in cholesterol, and high density lipoproteins.
Strong evidence of the connection between the state of blood lipids and atherosclerosis came from the results of international studies, which established that the degree of development of fatty streaks and plaques in the coronary arteries of the heart was associated with the level of total cholesterol and very low-density lipoproteins.
A high level of cholesterol in the blood can be a manifestation of a hereditary disease - familial hypercholesterolemia. The frequency of this disease in the heterozygous form is high and amounts to 1 case per 500 people in the population (with a cholesterol level of 7.5 -12.5 mmol/l). And the frequency of familial hypercholesterolemia in the homozygous form is much less common and amounts to 1 case per 1,000,000 people in the population (with a cholesterol level of 15 - 30 mmol/l). The homozygous, most severe form of this disease is characterized by the development of severe atherosclerotic vascular damage and its complications already in childhood, namely in the first decade of life. Cholesterol is deposited not only in the blood vessels, but also under the skin, on the tendons, and the cornea of the eye.
In general, lipid metabolism is a complex process that plays a leading role both in maintaining the vital functions of the body and in the development of a number of pathological conditions, one of which is atherosclerosis. If your family members under the age of 45 have already suffered myocardial infarctions, you should determine the blood cholesterol levels not only in yourself, but also in your children. Normally, the cholesterol level of a healthy person should not exceed 5.2 mmol/l.
Methods for correcting blood lipid disorders include: a low-fat diet, normalizing body weight, increasing physical activity, and, if necessary, taking special medications.
What are the common symptoms of cardiovascular disease?
Symptoms of heart attack and stroke
Often the underlying blood vessel disease is asymptomatic. A heart attack or stroke may be the first warning sign of the disease. Symptoms of a heart attack include:
- pain or discomfort in the middle of the chest;
- pain or discomfort in the arms, left shoulder, elbows, jaw or back.
In addition, the person may experience difficulty breathing or shortness of breath; nausea or vomiting; feel dizzy or faint; break out in a cold sweat and become pale. Women are more likely to experience shortness of breath, nausea, vomiting, and back and jaw pain.
The most common symptom of a stroke is sudden weakness in the face, most often on one side, arm or leg. Other symptoms include sudden numbness of the face, especially on one side, arms or legs; confusion; difficulty speaking or difficulty understanding speech; difficulty seeing in one or both eyes; difficulty walking, dizziness, loss of balance or coordination; severe headache for no specific reason, as well as loss of consciousness or unconsciousness.
People experiencing these symptoms should seek medical help immediately.
What is rheumatic carditis?
Rheumatic heart disease is damage to the heart valves and heart muscle due to inflammation and scarring caused by rheumatic fever. Rheumatic fever is caused by an abnormal response of the body to a streptococcal infection. The disease usually first manifests itself as a sore throat or tonsillitis in children.
Rheumatic fever primarily affects children in developing countries, especially in settings where poverty is widespread. Worldwide, rheumatic carditis is associated with almost 2% of all deaths from cardiovascular diseases.
Symptoms of rheumatic carditis
- Symptoms of rheumatic heart disease include: shortness of breath, fatigue, irregular heartbeats, chest pain and loss of consciousness.
- Symptoms of rheumatic fever include: fever, joint pain and swelling, nausea, stomach cramps and vomiting.
How can the burden of cardiovascular disease be reduced?
For the prevention and control of cardiovascular disease, WHO has identified a number of “best buys,” or highly cost-effective interventions that are feasible even in low-resource settings. They include 2 types of interventions—population-based and individual-level interventions—that can be used in combination to reduce the high burden of cardiovascular disease.
Examples of interventions that can be implemented to reduce CVD at a national level include the following:
- comprehensive tobacco control policies;
- taxation to reduce consumption of foods high in fat, sugar and salt;
- building walking and cycling paths to increase physical activity levels;
- strategies to reduce the harmful use of alcohol;
- ensuring proper nutrition for children in schools.
To prevent first myocardial infarctions and strokes, individual health interventions should target individuals with moderate or high overall cardiovascular risk or those with individual risk factors such as diabetes, hypertension and hypercholesterolemia above recommended levels. carrying out treatment.
The former (an integrated approach that takes into account all risk factors) is more cost-effective than the latter and can significantly reduce the incidence of cardiovascular events. This approach is feasible in low-resource settings, including the use of non-physician medical personnel.
For secondary prevention of CVD in people with pre-existing disease, including diabetes, treatment with the following medications is necessary:
- aspirin;
- beta blockers;
- angiotensin-converting enzyme inhibitors;
- statins.
The positive results obtained are largely unrelated, but when used in combination with smoking cessation, almost 75% of recurrent vascular events can be prevented. There are currently significant gaps in the implementation of these measures, especially at the primary health care level.
In addition, treatment of CVD sometimes requires expensive surgery. These include:
- coronary artery bypass grafting;
- balloon angioplasty (in which a small balloon catheter is inserted through an artery to restore lumen to a blocked vessel);
- plastic and valve replacement;
- heart transplant;
- operations using an artificial heart.
Some CVDs require medical devices to treat. These devices include pacemakers, artificial valves, and patches to close holes in the heart.
WHO activities
Under WHO's leadership, in 2013, all Member States (194 countries) agreed on global frameworks to reduce the burden of preventable NCDs, including the Global Action Plan for the Prevention and Control of NCDs 2013–2020. The plan aims to reduce premature deaths from NCDs by 25% by 2025 through 9 voluntary global targets. 2 of these global goals directly address the prevention and control of CVDs.
Goal six of the Global NCD Action Plan aims to reduce the global prevalence of high blood pressure by 25%. High blood pressure is one of the main risk factors for cardiovascular disease. The global prevalence of high blood pressure (defined as systolic and/or diastolic pressure ≥140/90 mmHg) among people aged 18 years and over in 2014 was about 22%.
To achieve this goal, it is necessary to reduce the incidence of hypertension through national policies that address behavioral risk factors, including harmful use of alcohol, physical inactivity, overweight, obesity and high salt intake. Early detection and cost-effective management of hypertension to prevent myocardial infarction, stroke, and other complications requires a risk-based approach.
Goal eight of the Global NCD Action Plan aims to ensure that at least 50% of eligible people receive drug therapy and counseling (including glycemic control) to prevent myocardial infarction and stroke. Preventing heart attack and stroke using a comprehensive approach that takes into account overall cardiovascular risk is more cost-effective than treating based solely on individual risk factor thresholds and should be part of the core package of services to achieve universal health coverage. sanitary assistance. Achieving this goal will require strengthening key components of the health system, including financing health care services to ensure access to essential health technologies and essential medicines for NCDs.
In 2015, countries will begin setting national targets and measuring progress against the 2010 baselines set out in the Global Noncommunicable Disease Status Report 2014. The UN General Assembly will hold its third high-level meeting on NCDs in 2021 to review countries' progress towards achieving the voluntary global targets by 2025.
Proper nutrition and lifestyle
Trans fats are fats containing trans isomers of unsaturated fatty acids. They are naturally present in small quantities in the meat and milk of ruminants. They are produced from vegetable oils using a special treatment method - hydrogenation: hydrogen is passed through liquid vegetable oil heated to high temperatures. The result is a solid fat mass that is resistant to oxidation. It is used to make margarines, confectionery and cooking fats, which are used to improve the taste and extend the shelf life of food products. Because these fats are cheap and easy to use, they are found in almost all industrially produced foods. Trans fats can also be formed during deep frying. Hydrogenated vegetable fats have recently been frequently introduced into many food products and are completely unjustifiably advertised as dietary fats. These fats behave in the human body like real fats of animal origin - they increase cholesterol levels and accelerate the aging process of the arteries. This type of fat is used to prepare products such as corn flakes, potato chips, and they are used in semi-finished products - pizzas, battered products, muffins, cookies, and candies.
When reducing the fat content in food, it is important not to exclude from the diet “heart-healthy” fats (mono- and polyunsaturated fats), mainly found in vegetable fats and seafood (fish oil).
How to change the ratio of fats in your diet:
- Use butter and spreads (butter substitutes) sparingly
- Choose lean meat
- Use grilling, steaming or baking meats. Avoid frying.
- Replace saturated fats such as butter with unsaturated oils such as sunflower, canola or olive oil
- Limit consumption of trans fats (such as margarine) for cooking
- Eat fatty fish (eg sardines, mackerel, fresh tuna, salmon)
Essential fatty acids (Omega-3, Omega-6). Previously known as vitamin F. Vitamin F is important for the cardiovascular system: it prevents the development of atherosclerosis, improves blood circulation, and has cardioprotective and antiarrhythmic effects. Polyunsaturated fatty acids reduce inflammatory processes in the body and improve tissue nutrition. Essential fatty acids are found in fatty fish. For heart health, you need to eat two servings of fish per week, one of which should be fatty.
Stanols and sterols
Plant sterols and stanols are the so-called phytoesterols - insignificant in content, but very important elements of the cell wall of plants. They are found in small amounts in some vegetable oils, nuts, grains, beans, fruits and vegetables. Plant sterols and stanols help lower blood cholesterol levels. Phytoesterols are added to foods - margarines, mayonnaise, yoghurts, orange juice, breakfast cereals, and much more. These fortified foods may be beneficial for people with high blood cholesterol. Clinical trials have shown that with regular use, they can reduce high blood cholesterol levels.
Fruits and vegetables
Fruits and vegetables are rich in many important nutrients, including vitamins C, E, and carotenoids (antioxidants). They may help protect the heart by limiting the harmful effects of cholesterol on body tissue. This confirms the need for daily inclusion of vegetables and fruits in the diet.
Whole grains and fiber
Research has shown that diets rich in whole grains can reduce the risk of heart disease by 30 percent. It is important to include whole grains at every meal, choosing wholemeal bread and using appropriate types of pasta and rice. Soluble dietary fiber found in oats and legumes can help lower LDL (low-density lipoprotein) cholesterol levels. These foods should be included as part of an overall healthy, balanced diet at least two to three times a week. Soy protein. Recommending a diet that includes at least 25 grams of soy per day has been associated with a reduction in cholesterol and cardiovascular disease. Soy isoflavones, in particular, reduce the risk of cardiovascular disease because they inhibit the growth of cells that form when arteries become clogged with atherosclerosis. Soy protein is also an excellent meat substitute and is available in a convenient and tasty form in many ready-made meals. Another good source of protein is soy milk and yogurt.
Rest and relaxation
While exercise can help lower blood pressure and strengthen the heart, rest and relaxation can reduce anxiety and improve your stress response. We all have to deal with situations such as divorce, bereavement, job loss or financial problems from time to time. There are also everyday events (traffic on the way to work, an argument with your partner, or a disagreement with someone at work) that can lead to stress—these everyday annoyances have an even greater impact because they are constant. Ways to cope with stress - Keep a journal - take note of stressful situations and how you responded to them. This will help you change how you react to stress in the future - Stay positive: Be in control of your feelings. Listen to your emotions. Replacing negative thoughts with positive ones will help you cope with stressful situations more calmly. — Learn to relax, pay attention to your posture, master yoga techniques, massage, meditation, etc. — Restore and regulate your sleep. Each person requires a different number of hours of sleep to feel rested. Try to get enough sleep every night.
Smoking
One of the most important steps you can take to reduce your risk of heart disease is to quit smoking. Smokers under 50 are five times more likely than non-smokers to die from coronary heart disease. Quitting smoking will reduce the risk of not only cardiovascular disease, but also lung diseases such as cancer and chronic obstructive pulmonary disease (COPD). Your doctor may prescribe nicotine replacement therapy or, for example, acupuncture to help you.