- Healthy Heart Library
- Prevention of cardiovascular diseases
Almost all diseases are easier to prevent than to treat later, and cardiovascular pathologies are no exception. In recent years, the frequency of such diseases has been steadily increasing, which is not surprising: most diseases of the heart and blood vessels are rightly considered by doctors to be diseases of civilization. They find nutritious soil in the form of the lifestyle of modern man with his poor nutrition, insufficient physical activity, acute and chronic stress. Therefore, doctors never tire of reminding us of the enormous role of timely prevention of heart disease, especially in patients at risk who are prone to such diseases. Preventive measures help prevent diseases, improve the patient’s quality of life, and prolong it.
Statistics on heart and vascular diseases
In Russia, heart and vascular diseases remain one of the main causes of mortality (up to 47%). However, in recent years there has been a gradual decrease in both the overall incidence of such diseases and mortality from them. Doctors attribute this both to the success of mass medical examinations and the increased effectiveness of modern treatment of heart diseases, and to increased public awareness of the importance of preventing such pathologies.
Preventative measures have been proven to protect against cardiovascular disease more effectively than any other measure. This is proven by research by epidemiologists: for example, a 50% reduction in the incidence of mortality from coronary heart disease is associated precisely with complex and active prevention, and only 40% with the improvement of methods of treating this pathology.
Major heart and vascular diseases
Diseases of the heart and blood vessels constitute a very large group, so the list below represents only the most basic and common pathologies:
- IHD (coronary heart disease), as well as its complications - heart attack, angina pectoris, cardiosclerosis;
- arterial hypertension;
- heart rhythm disturbances;
- congenital and acquired heart defects;
- heart failure;
- infectious and inflammatory pathologies of the heart - endo-, myo-, pericarditis;
- inflammatory vascular pathologies;
- atherosclerosis;
- systemic vascular pathologies;
- bleeding disorders.
Causes of cardiovascular diseases
The main cause of cardiovascular pathology is the lifestyle of a modern person. Insufficient physical activity, poor nutrition with a predominance of animals, “heavy” fats and “fast” carbohydrates, refined and canned foods, and fast food lead to increased blood cholesterol levels and metabolic disorders. The acute and chronic stresses that modern people face also contribute.
In addition, do not forget about bad habits: smoking and drinking alcoholic beverages negatively affect the condition of the walls of blood vessels and blood flow. All this together leads to the formation of certain pathologies: atherosclerosis, ischemic heart disease, hypertension and many others.
Climate change
I would also warn elderly and senile people against traveling to southern countries. The fact is that climate change, as a rule, does not improve health, but it can improve your mood. A new environment, new people, swimming, communication - this is a positive aspect. But, as a rule, climate change has a negative impact on health. And therefore, elderly and senile people, especially the sick, need to rest in a familiar climate zone. If it’s very hot, but there’s no way to go somewhere cooler, where there’s more shade, then at least you need to remember about air conditioning.
I would also caution against excessive use of air conditioning because it can cause rapid cooling. This is especially dangerous for elderly and senile people. And this is fraught with the development of pneumonia. In a significant percentage of cases, pneumonia can result in death.
What we have voiced today is not the speculation of a specific specialist. These are the results of many years of research by cardiologists in many countries - the USA, England, France, Germany, Italy, Japan and so on. These are the countries where, once they understood the situation with cardiovascular pathology, they achieved significant results, prolonging life and significantly reducing strokes and heart attacks.
I think that if you and I seriously think about this problem, we will be able to seriously delay or prevent these two formidable complications of our health. That's what I wish for you.
Primary and secondary prevention of heart and vascular diseases
Rational prevention of cardiac pathology is always comprehensive. It should include rationalization of nutrition, physical activity, stress management, giving up bad habits, and regular medical examinations. All of these measures can be classified as primary prevention measures, which are taken when the risk of heart disease is low. In the presence of pronounced predisposing factors to heart disease, it is necessary to use secondary prevention measures. Among them are weight loss, normalization of cholesterol and blood sugar levels, lowering blood pressure, and normalizing heart rate.
Nutrition to prevent heart disease
In order to ensure effective prevention of cardiovascular diseases, it is necessary to ensure a balanced diet. In this case, the best solution would be split meals in small portions 4-5 times a day; this is much healthier for the heart than two dense meals of large quantities of food. You should have dinner no later than 3 hours before going to bed.
If you are already overweight, you should adhere to a low-calorie diet, but calorie restriction should not be very strict. You can’t go hungry: a sharp restriction of the body’s diet leads to a deficiency of nutrients, including for the heart muscle.
Basic principles of nutrition for the prevention of heart disease:
- limiting “fast” carbohydrates - sugar, baked goods, sweets; preference should be given to dried fruits, honey, whole grain bread;
- The consumption of animal fats is limited; it is better to give preference to olive and flaxseed oil. It is better to exclude palm and coconut oil;
- limit the consumption of caffeinated drinks;
- salt consumption is limited, it is better to exclude sausages and smoked meats, pickles;
- It is better to completely eliminate the consumption of alcoholic beverages;
- from meat it is better to choose lean veal, chicken, rabbit, turkey;
- nuts, flax seeds, sesame are useful;
- It is recommended to consume large amounts of fiber in the form of vegetables, fruits, and herbs;
- healthy sea fish and seafood, fish oil in the form of supplements;
- It is recommended to consume fermented milk products daily, which stimulate digestion and saturate the body with calcium.
- Fast food, semi-finished products, products with an abundance of flavor enhancers and preservatives should be completely abandoned.
Dishes should be boiled, baked, steamed. It is recommended to completely exclude fried foods. It is necessary to drink a sufficient amount of liquid - up to one and a half to two liters per day. At the same time, strong tea or coffee should be avoided, preferring still mineral water, herbal tea, compote, fruit juice.
Physical activity to prevent heart disease
Modern man is becoming less and less mobile: work, thanks to the automation of processes, requires less and less effort, transportation takes him to his place of work, even laundry, washing dishes, turning on the TV no longer require real physical activity. Sedentary weekdays flow into similar weekends spent watching TV. This lifestyle contributes to excess weight gain and poor blood circulation in the tissues. In order to avoid developing heart disease, you need to increase physical activity. The best solution would be reasonable exercise in the fresh air - walking, Nordic walking, skiing, cycling. Cardio exercises in the gym (exercise bike, treadmill) are also useful. Swimming and gymnastics have proven themselves well.
An important condition for such physical activity: it should not be excessive and should not provoke overwork.
At the same time, it is important that the loads be regular: it is much better to walk 2-3 km every day, that is, half an hour, than to arrange a grueling two-hour session in the gym.
Preventative therapy and support for body health
Anyone can prevent the development of vascular and heart diseases. Comprehensive programs that include diets, exercise, timely treatment of infectious pathologies and protection from emotional overload will be of great benefit. Exercise and diet will not save you from poisoning with toxic substances or genetic predisposition. However, they will help stop the filling of the blood with cholesterol and prevent the growth of plaques on the walls of blood vessels.
First of all, you should optimize your diet. Classic diets are quite suitable for fighting diseases. Spicy, salty, smoked, fatty, floury, and fast carbohydrates should be excluded from the menu. You will need to reduce the consumption of strong tea and coffee, and store-bought condiments (ketchup, mayonnaise) and sauces should be abandoned altogether.
For the prevention of diseases, fresh vegetables, seafood, fruits, hard cheeses, and dairy products are recommended. Wheat and oatmeal porridge, cabbage, bananas, and nuts will saturate the body with essential microelements.
Proper physical activity is an indispensable condition for disease prevention. No need to start with cross-country running and marathon running. To maintain health and improve immunity, visiting the gym, swimming pool and walking at the same pace in the fresh air is enough. Such activities should be enjoyable and become a pleasant habit. At the initial stages, sports activities are best done under the supervision of a trainer.
It will be useful to protect the nervous system from the effects of emotional stress. The rhythm of modern life is such that it is impossible to completely eliminate stressful situations. However, it is possible to mitigate the harm from their effects. To do this, you should get enough sleep, have a good rest, and be in nature more often.
A prerequisite for the normal functioning of blood vessels and the heart is the timely disposal of foci of infectious diseases. Inadequate or delayed treatment of influenza and sore throat can cause abnormalities in the functioning of the body.
Prevention of cardiovascular diseases in children
It is better to protect the health of the heart and blood vessels from the first days of a child’s life. This means that from the first months of life it is important to accustom your baby to gymnastics - naturally, appropriate for his age, and proper nutrition. By the way, eating habits established in childhood are sometimes very difficult to change, and a child accustomed to an abundance of baked goods and sweets will most likely suffer greatly in adulthood due to the need to follow a diet.
Key points for the prevention of heart and vascular diseases in children:
- rational nutrition and maintaining normal body weight;
- sufficient physical activity, sports;
- prevention of bad habits;
- regular medical examinations.
The example of parents plays a huge role: if they eat right, lead a healthy and active lifestyle, the baby will have the right example before his eyes, which he will unconsciously adhere to.
The first signs of illness
Chest pain and discomfort behind the sternum are not the only sign of vascular and heart diseases. You can notice deviations in the functioning of the heart and blood vessels using other signs if you carefully monitor the condition of the body.
The main manifestations of the disease also include:
- arrhythmia that appears in the absence of negative external factors;
- shortness of breath that occurs with obesity, physical activity of an untrained body, excessive overload, the development of vascular and heart diseases;
- swelling, in which there is an accumulation of fluid (usually in the lower extremities towards the end of the day);
- regular headaches, accompanied by increased blood pressure and increased heart rate;
- pathological changes in skin color - pallor in the area of the nasolabial triangle, cyanosis, and also against the background of swelling of the legs.
If such signs appear, you must immediately contact a medical facility for help. You can refute or confirm your fears after an appointment with a specialized physician. For diagnosis, examination, listening to the heart, taking an anamnesis, taking EC and measuring blood pressure is usually sufficient.
Preventing heart disease in older people
Natural age-related changes in the body inevitably affect the cardiovascular system. The walls of blood vessels lose their elasticity, atherosclerotic plaques appear on them, blood pressure rises, and blood flow decreases. The risk of thrombosis of peripheral vessels increases, including coronary (myocardial infarction), brain (ischemic stroke), retina (blindness), etc. Therefore, in old age, it is especially important to regularly visit a cardiologist - at least once every six months starting from 40-50 years.
In addition to examining a doctor, it is recommended to:
- ECG, including with stress (for men);
- blood test for lipids;
- coagulograms.
In addition, you need to regularly monitor your blood pressure using a household tonometer.
Diagnostics
The diagnosis of pathology of the heart or blood vessels is established based on the results of a clinical examination, a patient interview, and a number of instrumental and laboratory tests. The main instrumental methods used in the diagnosis of CVD:
- Electrocardiography (ECG) is an electrophysiological method used in the diagnosis of arrhythmias and myocardial infarction. A variation is Holter monitoring, which allows you to take readings throughout the day using a portable device.
- Echocardiography (EchoCG) is an ultrasound method of examining the heart that reveals both functional disorders and structural disorders (tumors, vegetations, defects, inflammation). It is also prescribed for suspected pulmonary embolism.
- MRI, CT (magnetic resonance, computed tomography) of the brain - used in the diagnosis of strokes.
- Ultrasound scanning and dopplerography of blood vessels - used in the diagnosis of chronic cerebrovascular accidents and peripheral vascular diseases.
Laboratory tests include:
- In the diagnosis of inflammatory heart diseases - biochemical study of the protein spectrum, general blood test, bacterial blood culture.
- In the diagnosis of atherosclerosis - a biochemical test for the level of cholesterol, LDL, triglycerides.
- If any CVD is suspected, a coagulogram is performed.
Modern equipment allows diagnosis without invasive procedures.
Drugs for the prevention of cardiovascular diseases
Secondary prevention of cardiovascular diseases with the help of pharmaceuticals is extremely important, especially for people prone to such pathologies. For preventive purposes, complexes of vitamins and minerals, drugs with antithrombotic effects, and drugs that lower blood cholesterol levels can be taken. These drugs are usually sold without a prescription, but it is recommended that you consult a doctor before taking them.
Riboxin for the prevention of heart pathologies
Riboxin stimulates the supply of tissues, including the heart muscle, with oxygen, stimulates blood circulation, and normalizes heart rhythm. Taking the drug as a course course, treatment is prescribed by a doctor. There are contraindications, including gout and kidney failure.
Acetylsalicylic acid for the prevention of heart disease
Taking acetylsalicylic acid helps improve blood flow and has an antithrombotic effect. As a rule, for the prevention of heart disease, acetylsalicylic acid is produced in a special cardio dosage. To achieve the effect, long-term or continuous use is required. There are contraindications for use, including gastritis, gastric and duodenal ulcers.
Magnesium for the prevention of heart disease
Magnesium is a mineral that plays an important role in the health of the cardiovascular system, it helps stabilize the heart rhythm and lower blood pressure. Magnesium is included in many drugs for the prevention and treatment of cardiac diseases; your doctor will help you choose the optimal drug.
Fasostabil for the prevention of heart disease
Fasostabil is a complex drug in which the main active ingredient, acetylsalicylic acid, is supplemented with magnesium hydroxide. Thanks to this, the irritating effect of acetylsalicylic acid on the walls of the stomach is significantly reduced, in addition, magnesium has a mild hypotensive and stabilizing effect. The use of Fazostabil is preferable to taking regular acetylsalicylic acid; the drug is well tolerated.
Herbal medicine for the prevention of heart disease
Herbal medicines and various traditional medicines are available to everyone. It is important to remember that herbal remedies are only good as part of comprehensive prevention - they cannot replace a balanced diet or quitting smoking. In addition, individual intolerance or contraindications may also occur to herbal remedies. Among the “folk” remedies for the heart are:
- garlic - it should be consumed raw with food, as well as in the form of tincture, garlic oil;
- chokeberry, ground with honey;
- a mixture of persimmon and turnip juices with honey;
- a mixture of radish, carrot, beet juices with honey;
- a mixture of carrot juice with vegetable oil;
- a mixture of honey and royal jelly;
- hawthorn in the form of tea, tincture.
Nutrition
Nutrition should not have large restrictions in terms of product composition. The only thing that needs to be limited is easily digestible carbohydrates - sweets, flour products, cereals. And you need to limit animal fat. Limit, but under no circumstances stop using it. With all due respect to diets, drug interventions are still necessary, correction of blood clotting with cardiac aspirin, correction of lipid metabolism with statins and the use of other drugs, but as prescribed by a doctor. I specifically make this disclaimer. It does more good than harm.
Ten steps to a healthy heart!
Ten preventive measures that are simple and accessible to absolutely everyone: save this list and let your heart be healthy!
- Step 1 - rational nutrition. In your daily diet, it is recommended to minimize the consumption of fatty foods, fried foods, and reduce the consumption of salt, sugar, and caffeine. It is recommended to give preference to sea fish, lean poultry, whole grain bread, and consume a sufficient amount of fiber-rich vegetables and fruits.
- Step 2 - normalization of body weight. Excess weight automatically becomes a burden for the heart and blood vessels, in addition, it reflects an unfavorable balance of cholesterol in the body. It is known that excess body weight also contributes to increased blood pressure. If you have extra pounds, you need to reconsider your diet and increase physical activity. By the way, not only body weight as such plays a role, which should be normal (Quetelet body mass index is not higher than 28.0), but also waist circumference - no more than 88 cm in women and no more than 102 cm in men.
- Step 3 - increase physical activity. Physical inactivity is the enemy of the heart and blood vessels, and for the sake of their health, it is necessary to maintain a sufficient level of activity whenever possible. The choice of physical exercise depends on taste and capabilities; it could be swimming, gym classes, walking, not using a car or elevator, or gymnastics. What is important is not the specific type of activity, but the fact that the body will be sufficiently active at the same time.
- Step 4 - giving up bad habits. Smoking, alcohol, drugs, excessive coffee consumption and even energy drinks with excessive caffeine content gradually lead to diseases of the cardiovascular system, so you should get rid of such habits. If independent cessation is impossible due to an established addiction, it is worth resorting to special treatment.
- Step 5 - overcoming stress. Acute and chronic stress is an integral part of the life of a modern person and it is impossible to completely eliminate it. But a big role is played by a person’s personal perception of stressful situations, a reasonable and adequate reaction to them. Positive communication with pleasant people, relaxing hobbies, sports and walks, a rational daily routine in which there is time for rest, travel, and natural sedatives help to distract yourself. As with physical activity, the choice of methods to deal with stress remains up to the individual and depends on his preferences.
- Step 6 - control blood pressure. With blood pressure 140/90 mmHg. and below, control measurements should be carried out 1-3 times a year, at 140-180/90-105 mmHg. - twice a month, with blood pressure above 180/105 - daily. For persistent blood pressure levels above 140/90, antihypertensive therapy should be administered.
- Step 7 - systematic examinations with a cardiologist for those who are at risk for cardiovascular diseases and with a general practitioner for everyone else. Using modern equipment, a doctor can detect a disease even when it does not cause discomfort for the patient. And the earlier it is started, the more effective treatment is!
- Step 8 - control blood cholesterol levels. It should be done every year for all people over 30 years of age. The norm for a healthy person is 5 mmol/l, for a patient with diabetes mellitus - 4-4.5 mmol/l.
- Step 9 - Control your blood sugar levels. Also held annually starting at age 40. The norm is 3.3-5.5 mmol/l.
- Step 10 - taking blood thinning medications, for example, Fasostabil. The antiplatelet effect of acetyl salicylic acid is the most important factor in the prevention of coronary artery disease and its complications - myocardial infarction and ischemic stroke. Before starting to take the drug, you should consult your doctor.
Prevention of heart and vascular diseases in general is not difficult for the patient. Take care of yourself, be attentive to your health and your heart will thank you!
Risk factors for circulatory system diseases and their prevention
Risk factors for circulatory system diseases and their prevention
1. Biological (non-modifiable) factors:
- elderly age,
- male gender,
- genetic factors contributing to the occurrence
- - dyslipidemia,
- - hypertension,
- - glucose tolerance,
- - diabetes mellitus
- - obesity
2. Anatomical, physiological and metabolic features:
- arterial hypertension,
- dyslipidemia,
- obesity and the pattern of fat distribution in the body,
- diabetes
3. Behavioral factors:
- eating habits,
- smoking,
- physical activity,
- alcohol consumption,
- exposure to stress.
The presence of even one of the risk factors increases the mortality rate of men aged 50-69 years by 3.5 times, and the combined effect of several factors - by 5-7 times.
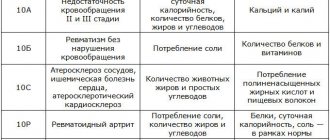
Currently, a distinction is made between primary, secondary and tertiary prevention of diseases of the circulatory system (hereinafter referred to as CVD). The first two types of prevention are consistent with previously put forward provisions, namely: primary prevention of coronary heart disease (hereinafter referred to as IHD) is the prevention of the development of the disease in healthy individuals and persons burdened with various risk factors, and secondary prevention is the prevention of the progression of the disease and the development of complications of the course of CHD. in people who already have this disease.
Tertiary prevention refers to the implementation of actions aimed at delaying the progression of heart failure (hereinafter referred to as HF). In heart failure, the relationship between traditional risk factors and disease outcome breaks down. The functional state of the left ventricle plays a decisive role. The onset of left ventricular remodeling is the starting point for tertiary prevention.
The main components of primary prevention are population strategy and individual prevention (high-risk strategy).
The population strategy, or mass prevention strategy, is to create a healthy lifestyle, which primarily involves reducing tobacco smoking, establishing a balanced diet, increasing physical activity for the entire population and improving the environment. These are, as a rule, government events that involve the involvement of not only and not so much the Ministry of Health, but other ministries and departments (Ministry of Sports and Tourism, Ministry of Agriculture, Ministry of Information, etc.).
Individual prevention (High-risk strategy) is the identification of individuals with high levels of risk factors (smoking, arterial hypertension, hypercholesterolemia, excess weight, low physical activity, etc.) and their correction.
The current recommendations “Prevention of Coronary Heart Disease in Clinical Practice”, developed by the working group of the European Society of Cardiology, the European Atherosclerotic Society and the European Society of Hypertension, emphasize the importance of assessing overall cardiovascular risk.
The priority for primary prevention, according to European guidelines, is healthy individuals who are at high risk of developing coronary artery disease or other atherosclerotic diseases due to a combination of risk factors, including smoking, high blood pressure and lipid levels (increased total cholesterol and low-lying lipoproteins). density (LDL), low high-density lipoprotein and high triglycerides, elevated blood glucose, family history of premature coronary disease or high hypercholesterolemia and other forms of dyslipidemia, hypertension or diabetes.
Secondary prevention should also include lifestyle changes (stop smoking, avoid second-hand smoke, eat rationally to lose weight, reduce blood pressure and cholesterol levels, control blood glucose, increase physical activity). If active lifestyle changes fail to achieve target levels of risk factors, drug therapy should be added. Patients with angina pectoris and those who have had a myocardial infarction should give preference to beta-blockers, and if they are not tolerated, long-acting calcium channel blockers.
ACE inhibitors should be prescribed to patients with significant left ventricular systolic dysfunction. Almost all patients are prescribed antiplatelet drugs such as aspirin 75 mg per day, etc. Simultaneous administration of aspirin and ACE inhibitors is undesirable.
If, with lifestyle changes, target cholesterol and LDL cholesterol levels are not achieved, lipid-normalizing drugs, primarily statins, must be prescribed. It is also necessary to correct high blood pressure and glucose levels.
The most unfavorable combination of risk factors is the so-called metabolic syndrome (MS), which is a complex of interrelated disorders of carbohydrate and fat metabolism, as well as the mechanisms of regulation of blood pressure and endothelial function. The basis of these disorders is a decrease in tissue sensitivity to insulin - insulin resistance. The main components of MS are abdominal-visceral obesity, hypertriglyceridemia, hyperinsulinemia and arterial hypertension. When these factors are combined, atherosclerosis develops at an accelerated rate.
Due to the particular aggressiveness of MS, it is called “deadly quartet”, “deadly sextet”, “syndrome X”, “insulin resistance syndrome”.
To diagnose MS, they most often resort to measuring waist circumference, determining the level of triglycerides in the blood serum and fasting insulin, and monitoring blood pressure.
When MS is detected, preventive and therapeutic measures should be aimed at the entire set of risk factors and include weight loss, adequate control of glycemia and dyslipidemia, and normalization of blood pressure. The management tactics for patients with hypertension and MS have a number of features:
- immediate initiation of treatment with antihypertensive drugs in combination with non-pharmacological measures (diet, physical activity);
- focus on achieving optimal or normal blood pressure (below 130/85 mm Hg), since it has been proven that stabilizing blood pressure at this level and below gives a real organoprotective effect;
- more frequent use of combinations of antihypertensive drugs, which is due to greater resistance to reducing high blood pressure in such patients.
If general measures fail to normalize carbohydrate metabolism, it is necessary to resort to medication to increase tissue sensitivity to insulin by using biguanides (metformin), β-glycosidase inhibitors (acarbose, miglitol), thiazolindiones (cyclitazone, engystol, pioglitazone, troglitazone). Sensitivity can also be increased by increasing tissue blood flow with the help of ACE inhibitors, β-blockers (doxazosin) and other drugs. The same should be done for hypertriglyceridemia: prescribe fibrates, nicotinic acid preparations, etc.
Tertiary prevention should be targeted specifically from the onset of left ventricular remodeling. This is the most important part of all preventive measures for CSD, since almost half of the hospitalizations of patients with cardiovascular pathology are for heart failure. The rate of re-hospitalization among patients with CHF within 3 months after discharge reaches 47%, within 6 months - 54%. The costs of treating patients with CHF exceed the costs of treating patients with the most common forms of cancer and myocardial infarction. Left ventricular function in such patients has a primary influence on the outcome of the disease. Low or normal blood pressure, elevated cholesterol and brain natriuretic peptide levels increase the risk of heart failure and are associated with increased mortality.
It has been proven that the main drugs that protect the myocardium are ACE inhibitors and beta blockers. It has now been practically established that aspirin has an adverse effect in the treatment of patients with CHF. Nothing is known yet about the safety and effectiveness of statins in patients with HF.
Currently, a multidisciplinary approach to the treatment of heart failure is generally accepted, the essence of which is to unite doctors and representatives of other specialties to comprehensively address the many medical, psycho-social, behavioral and financial problems faced by patients with heart failure and the doctors treating them.
One of the organized forms for the practical application of a multidisciplinary approach to the treatment of CHF is the heart failure clinic. It can be presented both as an inpatient unit and as a day hospital at an outpatient clinic facility, which has at its disposal the means for diagnosis, monitoring and the ability to provide adequate treatment.
The team that will be involved in the treatment of patients with CHF in heart failure clinics, according to LR Erhardt, should include a cardiologist or heart failure specialist, a specially trained nurse, a gerontologist, a social worker, a physiotherapist, a general practitioner, a psychologist, a nutritionist and clinical pharmacologist.
What goals need to be achieved in the fight against risk factors?
According to WHO, three main risk factors make the greatest contribution to the risk of sudden death: hypertension, hypercholesterolemia (dyslipidemia) and smoking.
Arterial hypertension (HTN) is often called the “mysterious and silent killer.” Mysterious - because in most cases the causes of the disease remain unknown, silent - because in many patients the disease is asymptomatic and they do not know about the presence of high blood pressure (BP) until any complication develops. In order to correctly determine the risk of developing arterial hypertension and, as a result, coronary artery disease, you need to know and control your blood pressure level, and, if necessary, undergo an examination that will help clarify disorders of carbohydrate and fat metabolism and the degree of damage to target organs (vessels, heart, kidneys) , brain).
Analysis of the study results showed that to diagnose target organ damage in our country, examination methods such as ultrasound of the brachiocephalic arteries (in 9% of patients, versus 24.1% in other countries), determination of microalbuminuria (in 0.7% of patients versus 10% in other countries), and 24-hour blood pressure monitoring is performed less frequently (in 8.9% of patients, versus 24.5% in European countries).
An analysis of prescribed antihypertensive therapy showed that treatment of patients with hypertension in the Republic of Belarus is carried out with modern drugs, in 80.4% combination therapy is prescribed, which is comparable to the results of treatment in other European countries. In our country, as well as in comparison countries, there is a low effectiveness of treatment of patients with hypertension with concomitant diabetes mellitus (the target level is achieved in only 10% of patients).
Dyslipidemia is an imbalance in the content of “bad” and “good” fat fractions in the blood towards an increase in “bad” and/or a decrease in “good” fats. “Bad” fats, an increased amount of which greatly increases the risk of developing atherosclerosis and coronary artery disease, include cholesterol, low- and very low-density lipids, and triglycerides. To the “good” fats, i.e. Preventing the development of CVD include high-density lipids. With the exception of a small number of people with hereditary hypercholesterolemia, cholesterol levels are generally associated with poor diet. A balanced diet requires eating plenty of fruits and vegetables, healthy breads, lean meats, fish and legumes, along with low- or no-fat foods.
Soft margarine, sunflower, corn, rapeseed or olive oil should be used. The total fat content should not exceed 30% of the total energy composition, and the saturated fat content should not exceed 1/3 of all fat consumed. Many years of clinical experience indicate the unique properties of omega-3 polyunsaturated fatty acids, which help reduce the risk of CVD and its complications. More than 30 years ago, a group of Danish researchers suggested that the low incidence of cardiovascular pathology among the Greenland Eskimos was associated with their high consumption of deep-sea fish and seafood.
In epidemiological comparative, prospective and clinical studies, it has been shown that the intake of omega-3 polyunsaturated fatty acids at a dose of 2-4 g per day, both with increased amounts of fish consumed and in the form of encapsulated fish oil, leads to the correction of dyslipidemia and reduces the risk of death in patients who have had myocardial infarction. The presence of dyslipidemia is determined by a doctor based on the results of a biochemical analysis of venous blood. If dyslipidemia is present, its correction begins with diet. If, with the help of diet and balanced nutrition, it is not possible to reduce the lipid spectrum within 3 months, and a person simultaneously has other risk factors, drug therapy is prescribed.
A balanced diet is a balanced, regular (at least 4 times a day) diet with limited salt intake. Research by scientists has shown that if you limit your salt intake, the risk of myocardial infarction and other heart events can be reduced by 25%. It is very useful to increase the consumption of foods containing potassium and magnesium (seaweed, raisins, beets, apricots, zucchini, pumpkin, buckwheat).
Healthy food choices
All individuals should receive professional advice on food choices and follow a diet that is associated with minimal risk of developing CVD.
General recommendations (determined according to cultural traditions):
- food should be varied, energy consumption should be optimal to maintain ideal weight;
- Consumption of the following foods should be encouraged: fruits and vegetables, whole grains and breads, low-fat dairy products, lean meats, fish;
- consume products containing fish oil and w-omega, which have special protective properties;
- the total fat content should not exceed 30% of the total energy composition, and the saturated fat content should not exceed a third of all consumed fats; the amount of cholesterol consumed should be less than 300 mg/day;
- with a low-calorie diet, saturated fats should be replaced partly with carbohydrates, partly with monounsaturated and polyunsaturated fats from vegetables and marine animals.
In the diet, it is recommended to limit the consumption of animal products rich in cholesterol and saturated fats: fatty meats, lard, butter, sour cream, egg yolk, fatty cheese, sausage, sausages, all offal, fish caviar, shrimp, squid. It is recommended to replace animal fat with vegetable fat, since the latter is rich in anti-atherogenic unsaturated fats. Polyunsaturated fats (PUFs) are found in the form of omega-6 linoleic acid in vegetable oil (sunflower, corn, cottonseed) and in the form of omega-3 alpha-linolenic acid in flaxseed and soybean oils. The minimum daily human need for essential linoleic acid is 2-6 g, which is equivalent to 10-15 g of sunflower oil (2-3 teaspoons).
Fish oil is rich in polyunsaturated omega-3 fatty acids (omega-3 PUFAs) - eicosapentaenoic acid and docosahexaenoic acid. Preference should be given to fish from the northern seas that contain a lot of omega-3 PUFAs (mackerel, sardines, tuna, salmon, mackerel, herring, halibut, etc.). It has been established that polyunsaturated fatty acids significantly reduce the level of TG and, to a lesser extent, total cholesterol. Other effects of omega-3 PUFA include its effect on blood pressure levels, suppression of thrombus formation and improvement of endothelial function. It has been established that the likelihood of developing coronary heart disease is reduced by at least 25-30% when eating fish 2-4 times a week.
Over the past decade, hydrogenated vegetable oils have been widely used in the diet. The level of trans isomers (harmful substances) in hard margarines can reach up to 60%. Trans isomers of unsaturated fatty acids are similar to saturated fatty acids in lipid metabolism. It has been proven that their consumption (more than 1%) increases the risk of development and progression of coronary heart disease due to a significant increase in the levels of total cholesterol and LDL cholesterol and a decrease in the concentration of HDL cholesterol. To prevent atherosclerosis, it is recommended to use only soft margarine, produced in tubes (margarine spread) and plastic boxes, with a low content of saturated fat and trans-isomers of fatty acids (FA) (less than 1%). Replacing butter with “soft” margarine reduces the risk of IHD by 10%. However, the amount of soft margarine consumed should be limited, spreading no more than 5 g on bread.
Typically, by limiting dietary cholesterol intake to 300 mg per day over time, it is possible to reduce its blood level by 10-15%, and by reducing total fat intake from 40 to 30% of the total caloric intake - by another 15-20%.
Another important principle of anti-atherogenic nutrition is increasing the consumption of plant-based foods that can bind and remove cholesterol from the body. In this regard, it is recommended to use:
— dietary fiber (at least 30 g per day); they are found in large quantities in fruits (pears, apples, oranges, peaches), berries (raspberries, strawberries, blueberries), vegetables (cauliflower, broccoli, green beans) and legumes (peas, lentils, beans);
- pectins (at least 15 g per day), which are found in fresh fruits (apples, plums, apricots, peaches), berries (black currants) and vegetables (carrots, beets);
— plant stanols (at least 3 g per day); they are contained in soybean and rapeseed oils, pine oil extracts; Recently, sterols/stanols, being plant lipids, have been shown to reduce LDL cholesterol levels in the blood by competitively inhibiting the absorption of cholesterol in the small intestine.
It has been proven that their regular use is accompanied by a decrease in the concentration of LDL cholesterol by 10-15%; Margarines and fermented milk products fortified with sterols/stanols are now available and may be a useful addition to a lipid-lowering (HL) diet or drug treatment for DLP.
To prevent atherosclerosis, it is recommended to eat more fruit - at least 400 g or 5 servings per day: 1 serving = 1 apple / 1 banana / 1 orange / 1 pear / 2 kiwi / 2 plums / 1 tablespoon of dried fruit / 1 large slice of melon or pineapple / 1 glass of juice. The amount of boiled or fresh vegetables in the diet should be at least 400 g (2 cups).
Basic principles of the diet recommended for the prevention of atherosclerosis and DLP:
1. regular consumption of a variety of vegetables and fruits (fresh vegetables for dessert);
2. the ratio between saturated, mono- and polyunsaturated fats should be 1:1:1;
3. moderate consumption of dairy products (skim milk, low-fat cheese and low-fat yogurt);
4. give preference to fish and poultry (without skin) over meat products;
5. from meat products, choose lean meat, without layers of fat;
6. consume no more than 2-3 eggs per week (the consumption of yolks is limited, but not the white, which can be unlimited).
Excess body weight increases the risk of developing coronary artery disease and other diseases associated with atherosclerosis. To estimate your weight, use a simple formula for determining your body mass index (weight (kg) / height (m2) = body mass index). If the body mass index is less than 25, this is the desired body weight; if more than 28 in women and 30 in men, we can talk about obesity. Moreover, the so-called central obesity (male type), when fat is deposited on the abdomen, is more dangerous. The presence of central obesity can be judged by waist circumference and the ratio of waist circumference to hip circumference. The risk of CVD increases in men with a waist circumference greater than 94 cm and, especially, with a circumference greater than 102 cm; in women, greater than 80 cm and 88 cm, respectively. The ratio of waist circumference to hip circumference in men is greater than 1.0 and in women greater than 0. 85 is a more accurate indicator of the central type of obesity. The most common causes of excess weight are family factors (some of which may be genetic, but more often reflect general eating habits), overeating, a diet high in fat and carbohydrates, and lack of physical activity. Overweight is most common among sections of society with lower cultural and educational levels, especially among women due to lack of a balanced diet.
Smoking is one of the main risk factors. Why is smoking dangerous? Because even one cigarette increases blood pressure for 15 minutes, and with constant smoking, vascular tone increases and the effectiveness of medications decreases. If a person smokes 5 cigarettes a day, this increases the risk of death by 40%, if one pack a day - by 400%, that is, the chances of dying are 10 times greater!
According to WHO, 23% of deaths from coronary heart disease are caused by smoking, reducing the life expectancy of smokers aged 35-69 years by an average of 20 years. Sudden death among people who smoke a pack of cigarettes or more per day is 5 times more common than among non-smokers. Smokers not only put their lives at risk, but also the lives of others (passive smoking increases the risk of coronary artery disease by 25-30%). After just 6 weeks of following a healthy lifestyle, dramatic changes in health occur, and among those who quit smoking, the risk of coronary heart disease is significantly reduced and after 5 years it becomes the same as for those who have never smoked.
Low physical activity contributes to the development of CVD 1.5-2 times more often than in people leading a physically active lifestyle. Walking at a brisk pace for half an hour a day can reduce the risk of heart disease by approximately 18% and stroke by 11%. For the prevention of CVD and health promotion, the most suitable physical exercises are those that involve regular rhythmic contractions of large muscle groups: fast walking, jogging, cycling, swimming, skiing, etc. The frequency of physical exercise should be at least 4-5 times a day. week, duration of classes is 30-40 minutes, including a warm-up and cool-down period. When determining the intensity of physical exercise acceptable for a particular patient, they proceed from the maximum heart rate (HR) after physical activity - it should be equal to the difference between the number 220 and the patient’s age in years. For people with a sedentary lifestyle without symptoms of coronary artery disease, it is recommended to choose an intensity of exercise at which the heart rate is 60-75% of the maximum. Recommendations for individuals with CAD should be based on clinical examination and exercise test results.
The Committee of the European Society of Cardiology has developed the main tasks for the prevention of CVD in a healthy person:
- systolic blood pressure below 140 mm Hg;
- no tobacco use;
— total cholesterol level below 5 mmol/l;
— low-density lipoprotein cholesterol below 3 mmol/l;
- walking 3 km a day or 30 minutes of any other moderate physical activity;
- daily use of at least 5 pieces of fruits and vegetables;
- Avoid obesity and diabetes.
The experience of multifactorial prevention of coronary artery disease carried out by the Republican Scientific and Practical Center "Cardiology" since 2000 at the population level in Minsk has shown that a decrease in the levels of risk factors in combination with active measures for secondary prevention is accompanied by a decrease in the incidence of myocardial infarction by 21%, cerebral stroke by 21%. 24%. At the same time, the practical implementation of preventive programs, which involves a set of measures to increase the population’s literacy in matters of a healthy lifestyle and resolve a number of social issues relating to a balanced diet, the organization of physical culture and health activities for the population, etc., requires the widespread involvement of republican and local government bodies.
Thus, to effectively prevent most cardiovascular diseases and their complications, you need to follow only 7 rules:
1. Monitor your blood pressure.
2. Control your cholesterol levels.
3. Eat right.
4. Exercise: A little is better than nothing.
5. Don’t start smoking, and if you smoke, try to quit, no matter how difficult it may seem.
6. Do not abuse alcoholic beverages.
7. Try to avoid prolonged stress.
In conclusion, even small lifestyle changes can slow down the aging of the heart. It's never too late to start living a healthy lifestyle. After a person develops signs of coronary artery disease, risk factors continue to act, contributing to the progression of the disease and worsening the prognosis, so their correction should be an integral part of treatment tactics.