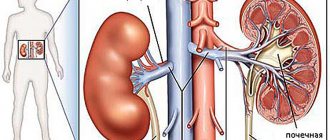
Vasorenal hypertension (also vasorenal arterial hypertension , renovascular hypertension ) is a fairly common syndrome of high blood pressure among all age groups of both sexes, caused in most cases by disturbances of normal blood flow in the renal arteries (renal ischemia).
The processes of arterial stenosis due to atherosclerosis or fibromuscular dysplasia, arteriovenous fistulas, nonspecific aortoarteritis, thromboembolism and other diseases, complicating the normal flow of blood through the renal arteries, prevent the enzyme renin, secreted by the kidneys, from entering the arteries. This enzyme is responsible for regulating blood pressure; a decrease in its amount in the blood leads to hypertension.
Caused by hereditary or acquired arterial diseases, renovascular hypertension is usually very resistant to the effects of drugs and is usually permanent. Based on this collective characteristic, it can be distinguished from other types of arterial hypertension (high blood pressure).
1
Ultrasound in MedicCity
2 Consultation with a phlebologist in MedicCity
3 Vascular surgery in MedicCity
Regular examination by a phlebologist or vascular surgeon will help you avoid serious complications if vascular pathology is detected. Delay in treating vascular diseases is life-threatening! Trust your health to the MedicCity professionals!
Vasorenal hypertension
74% of people do not know their blood pressure and do not know and do not start taking care of their health until they reach a critical point. However, such formidable complications that appear against the background of high blood pressure, such as coronary heart disease and strokes, are superior to the same AIDS or cancer.
Unfortunately, hypertension can appear at any age. The main causes of hypertension are poor diet, lack of exercise, elevated glucose levels and blood fat levels. Added to this are chronic overwork, stress, smoking and other attributes of modern life.
So, for an adult, blood pressure is considered normal no higher than 140/90 mmHg. And in some cases, for example, in the presence of diabetes mellitus, kidney disease, the pressure should be even lower - at the level of 130/80 - 120/70 mmHg, in order to prevent the progression of these diseases and the development of complications. With hypertension, the heart works overload, pumping an additional volume of blood. Over time, this leads to changes in the artery wall. They thicken and harden, lose their elasticity, which can lead to the development of narrowing or pathological expansion, and even rupture of the vessel may occur. If this complication occurs in a vital organ (heart, brain), then it can result in myocardial infarction or cerebral hemorrhage (stroke) . But, despite this danger, the insidiousness of hypertension is that it can be completely asymptomatic for a long time.
Unlike a number of diseases that you can “get over,” hypertension, as a rule, is a chronic, lifelong condition.
If you have been diagnosed with arterial hypertension, you need to find the reasons why your blood pressure may be elevated. Most often, hypertension is primary in nature, i.e. develops for no apparent reason. Less commonly, high blood pressure is secondary and is a sign of diseases of various organs (kidneys, blood vessels, etc.). Each of these diseases requires special treatment. That is why any increase in blood pressure requires consultation with a cardiologist.
Treatment of any increase in blood pressure begins with so-called regimen and dietary measures. Sometimes this gives a positive result and in the future mandatory blood pressure monitoring is required by the patient himself. If this is not enough, then the cardiologist will need to select a medication regimen for you. When prescribing one or more drugs, the doctor takes into account the level of blood pressure, the severity of hypertension, the main risk factors or causes of arterial hypertension, the severity of target organ damage, the presence of concomitant diseases, the interaction of drugs with each other and with other medications taken, and the possibility of developing side effects. Therefore, it is absolutely unacceptable for a patient to change doctor’s prescriptions, drug doses, frequency of administration, or discontinue one or another drug on their own. A lot depends on the patient himself. It is important to combat risk factors - this means quitting smoking, limiting alcohol consumption, regularly taking recommended medications and monitoring their effect on blood pressure by recording measurements in a special diary, reducing excess weight, leading an active lifestyle, limiting alcohol consumption (10 - 20 g for women, 20 - 30 for men in terms of pure ethanol). Reasons that are much more difficult to cope with include obesity, alcohol abuse, the use of certain medications, breathing disorders and stopping during sleep, and kidney disease.
But sometimes it happens that the patient is already taking 3 or more medications, and the pressure has not stabilized at the target level. This form of hypertension is classified as resistant.
What to do?
There is another important cause of resistant arterial hypertension – damage to the renal arteries. The most common cause of narrowing or occlusion (blockage) of the renal artery is the deposition of atherosclerotic plaques on the inner walls of the vessel. Enlarged plaque narrows the artery and slows blood flow, leading to renal ischemia.
Less common are congenital defects in the development of arterial walls (fibromuscular dysplasia), inflammation, or neurofibromatosis. If the development of renovascular hypertension is suspected, the doctor recommends Doppler ultrasound. If this study reveals changes in blood flow in the arteries of the kidneys, then the next stage of the examination to clarify the anatomy of the lesion will offer you modern diagnostics - multislice computed tomography (MSCT) of the renal arteries.
Or angiography of the renal arteries
If you have been diagnosed with damage to the renal arteries, then in the future it will be necessary to decide on angioplasty and stenting of the renal arteries.
Today, all over the world, stenting of the renal arteries is the most advanced and least traumatic method of treating stenoses. The procedure is painless and is performed under local anesthesia through a puncture in the femoral artery. Surgeries allow you to restore the lumen of narrowed arteries using special balloon catheters and stents (endoprostheses). The stent is a cylindrical endoprosthesis, laser cut from a solid metal tube. After angioplasty and stenting, the internal lumen of the artery is restored and thereby the blood supply to the kidney is improved, which leads to improved functioning and normalization of blood pressure numbers. The entire examination and treatment takes only 2-3 days.
However, there are patients who do not have damage to the renal arteries and do not have diseases leading to the development of secondary arterial hypertension. And, despite taking large doses of antihypertensive drugs, blood pressure remains elevated.
The increase in blood pressure is also influenced by renal activation of the sympathetic nervous system, which produces adrenaline and norepinephrine. Excessive increases in blood pressure are a response to physical or emotional stress in people without hypertension and increase the risk of developing high blood pressure later in life by five times.
In this case, there is a non-surgical method for correcting blood pressure through the so-called denervation of the renal arteries. The method involves inserting a catheter through a puncture in the femoral artery. Next, a catheter is inserted into the renal artery and radiofrequency energy is used to create damage to the neural network of the surrounding renal arteries. The procedure takes about 40 minutes, after which the catheter is removed. The duration of the patient's stay in the hospital is 1 day. The result is a decrease in blood pressure that persists over subsequent years without deterioration in kidney function or metabolic disorders. On the contrary, there is an improvement in kidney function and a significant improvement in metabolic parameters such as blood glucose, insulin and insulin resistance index.
Currently, renal denervation is used only in patients with resistant hypertension. This does not mean that medications are no longer needed. Patients will still likely need to take high blood pressure medications, but the number of medications needed to keep blood pressure at target levels will be significantly reduced.
The doctors of our clinic will help you conduct the necessary examination and correctly prescribe medication and, if necessary, perform surgical correction of arterial hypertension - percutaneous balloon angioplasty and stenting of the renal arteries or radiofrequency ablation.
Hypertension. Hypertension
Terminology
The question of how hypertension differs from hypertension is one of the most frequently asked, and it seems advisable to start with terminology.
We say “good tone”, meaning vivacity, energy and readiness for action; otherwise, we rely on “tonic” drinks. The tensor is called the “tensor muscle”, the extensor is the extensor muscle. Stresses in the cross section of a solid body are described by tensor algebra equations. “Tone” translated from Greek means tension (eg, muscle hypertonicity - inability to relax); The Latin “tensio” is translated in almost the same way, but with an even more mechanical connotation: it means compressive, pressure, and tensile stresses. The last two words in this context are key.
Both hypertension and hypertension are pathologically high blood pressure, which gradually stretches and thins the vascular walls. In ICD-10 (International Classification of Diseases), both terms are used as nosological units, and one of them usually follows the other in parentheses, for example: “Hypertensive heart disease (hypertensive heart disease) with a predominant lesion ...”, etc. Perhaps the wording will become clearer in the eleventh edition of the ICD, which is expected to be adopted in 2018.
In the literature one can find different interpretations of the terms “hypertension” and “hypertension”, including the opinion that they are absolutely synonymous. However, any linguist knows that absolute synonyms in languages (especially in such a strict and clear language as medical) practically do not occur, i.e. one or another semantic connotation is always present in synonyms. Therefore, a number of sources give a different interpretation, simple, brief and logically separating the two concepts.
Hypertension is a disease itself, which is characterized (like other diseases) by certain causes and risk factors, patterns of development, typical variants of the clinical picture and outcome. Hypertension is a pathophysiological phenomenon of elevated blood pressure; in addition, it is a set of interrelated symptoms that manifest hypertension.
In short: hypertension is a disease, hypertension is a typical syndrome for it. (In passing, we note that the same syndrome can accompany different diseases, anomalies and conditions).
One way or another, the problem of chronically high pressure in the blood vessels remains so acute around the world that its non-medical synonyms most often become darkly poetic images like “the silent killer”, “silent killer”, “disease of the century”, “curse of civilization” and etc. These definitions cannot be called groundless: hypertension has a tendency towards a long latent or asymptomatic course, and the very first clinical manifestation - if it is a hypertensive crisis, myocardial infarction, acute cerebrovascular accident - can be fatal.
As with other “diseases of the century,” epidemiological estimates of hypertension vary widely depending on region, the dominant diagnostic approach, the composition of the samples studied, and many other factors. In all likelihood, clinically significant hypertension affects between 20 and 50 percent of the world's adult population. About half of them don't know about it. Of the remaining, informed half, a significant portion of patients, for various reasons, do not take any therapeutic or preventive measures.
At the same time, in regularly published statistical data on the causes of non-violent mortality, cardiovascular diseases consistently occupy the first position, and the largest contribution to “cardiovascular” mortality belongs to arterial hypertension (at least in Russia this is the case).
Medicine does not stand still; Thanks to the intensive development of theory and methodology, technology, and pharmacology, the mortality rate from arterial hypertension has been significantly reduced in the last 30-40 years. And yet the situation remains, to put it mildly, unsatisfactory.
City Hospital reports!
All organs and tissues of the body are penetrated by small arterial vessels - arterioles. Sometimes, for a number of reasons, these vessels begin to narrow. In this case, the heart, in order to push the same amount of blood from the arteries into the veins, needs to apply more force, creating more pressure in the arteries. It is this increase in pressure in the arteries that is called arterial hypertension (simply hypertension or hypertension).
Hypertension occurs in 10-20% of people aged 25-45 years and in 30-40% over 45 years of age.
There are many causes of hypertension; chronic stress, poor nutrition, smoking, age and hereditary factors have been proven to influence the development of this disease. But these are only factors predisposing to the development of the disease. In most cases, the exact cause cannot be determined and a systematic increase in blood pressure is called primary hypertension or essential hypertension. Treatment in this case is aimed at eliminating these negative factors and prescribing medications to lower blood pressure.
However, in some cases, hypertension occurs due to impaired blood supply to the kidneys - a cause that can be radically eliminated. The cause in such situations is most often a narrowing of the renal artery by an atherosclerotic plaque, or due to a congenital defect in the development of the artery walls (fibromuscular dysplasia). This disease is called renovascular (renovascular) hypertension or renal hypertension.
Vasorenal hypertension (hypertension) and its causes
If the kidney, due to narrowing of the artery, does not receive enough blood, it begins to release substances into the blood that contribute to the occurrence of arterial spasm and increased blood pressure. Thus, the kidney provides itself with greater blood flow through the narrowed artery. In other words, renovascular hypertension is a protective reaction of the kidney to decreased blood supply. In this case, drug-induced reduction of blood pressure can lead to disruption of the blood supply to the kidney and a deterioration in its function, up to and including renal failure.
The most common cause of renovascular hypertension is narrowing of the renal artery by atherosclerotic plaque. In addition, there are cases of congenital disorders of the development of the wall of the renal arteries - fibromuscular dysplasia, which also significantly narrow the vascular lumen. Impaired blood supply to the kidney, leading to vasorenal hypertension, can also be caused by kidney prolapse, aortoarteritis, aneurysm of the aorta and renal artery, or external compression, but these cases are quite rare.
Difference between renovascular hypertension and hypertension
The assumption of a renovascular cause of hypertension should arise in cases of unresponsiveness or poor responsiveness to therapy, especially if hypertension was previously well responsive to drug correction; with the sudden development of severe hypertension in patients with initially normal blood pressure. You should also be wary of hypertension at a young age, especially in young women, the presence of concomitant kidney diseases, and changes in the retina.
If a vasorenal cause of hypertension is suspected, it is necessary to perform a duplex scan (Doppler ultrasound) of the renal arteries, which can reveal clinically significant (more than 50%) narrowing of the renal artery. Similar results are obtained using angiographic examination (angiography) of the renal vessels. In doubtful cases, laboratory determination of the level of specific hormones is performed.
Treatment of renovascular hypertension
Treatment of renovascular hypertension is aimed at eliminating the narrowing of the renal arteries. Drug antihypertensive therapy, in the case of narrowing of the renal arteries, as a rule, does not bring sufficient effect; moreover, it can contribute to the development of renal failure.
1. Surgical treatment: removal of an atherosclerotic plaque, damaged area of a vessel, or application of a bypass shunt. This is a rather complex and traumatic surgical procedure. Currently, due to the rapid development of endovascular surgery, it is used much less frequently, mainly in cases where endovascular treatment is impossible.
2. Endovascular treatment: balloon dilatation (angioplasty) or stenting of the renal artery.
Procedure for endovascular restoration of the renal artery lumen
The endovascular surgeon performs a puncture of the femoral artery. In some cases, access through the arteries of the arm is possible. A catheter is passed through the puncture hole into the aorta, and an angiographic study is performed to clarify the location of the renal arteries and the degree of their narrowing. The catheter is brought to the renal artery, through which a balloon is installed at the site of narrowing. The balloon is then inflated at the site of the narrowing, which causes the narrowed section of the artery to smooth out. After the balloon is deflated, a control angiogram is performed, which shows changes in the lumen of the artery. In fibromuscular dysplasia, such intervention usually completely eliminates the narrowing. If the narrowing of the artery lumen is caused by an atherosclerotic plaque, a control angiogram often shows residual stenosis of the renal artery. This is caused by the fact that during dilatation the plaque is not physically removed, but is evenly distributed along the artery wall, “smoothed out.” Therefore, in many cases, to completely eliminate the narrowing, a stent is installed in the renal artery - a special device that allows you to support the artery wall from the inside, “reinforce” the narrowing site. Stenting allows you to completely restore the patency of the renal artery without damaging the surrounding tissue. After the intervention is completed, the catheter is removed from the artery, a pressure bandage is applied to the puncture site, and in the case of femoral access, the patient is prescribed bed rest until the next morning.
The intervention is practically painless, is performed under local anesthesia, and the stay in the clinic can last 2-3 days. After the intervention, drugs that reduce thrombus formation are prescribed for several months to prevent thrombosis of the dilated artery.
results
After the narrowing of the renal artery is eliminated, blood pressure begins to decrease. The prospects for its stabilization depend on the duration of the stenosis. If the narrowing exists for a long time (for years), eliminating it may not completely normalize the pressure, but a positive effect is achieved in most cases.
In the first 1-2 days after endovascular intervention, blood pressure may be unstable and may fluctuate. This occurs as a result of changes in blood supply conditions; the kidney “adapts” to the redistribution of blood flow.
Side effects, complications, relapses
The most common complication of any endovascular intervention is puncture site hematoma. This complication does not require additional hospitalization; in the vast majority of cases it is treated conservatively. Complications at the dilation/stenting site are extremely rare. These include renal artery thrombosis, its rupture with a balloon or stent, and stent dislocation. As a rule, such complications may be associated with insufficient experience of the doctor or imperfect instruments. If the operating specialist has many years of experience and high-quality instruments, the risk of such complications can be less than 0.5-1%, in addition, they can be eliminated by endovascular methods, without open surgery.
Is it possible for the renal artery to narrow again? In the case of fibromuscular dysplasia, relapse is unlikely, but in atherosclerosis, repeated narrowing of the artery over time is possible and may be associated with the development of a new plaque or growth of the intima (inner lining of the artery) at the site of the stent. If such a relapse occurs, repeated dilatation is often sufficient to eliminate it (re-stenting is rarely required). In aortoarteritis, repeated narrowing of the renal artery is associated with an inflammatory process in the aorta. A solution to this situation can be the use of stents covered with a thin plastic sheath (grafts). Without eliminating inflammation, this design prevents the pathological process from moving to the mouth of the renal artery and narrowing it again.
And finally...
The currently accumulated experience in the use of endovascular reconstruction of the renal arteries allows us to recommend the method to everyone who faces the problem of treating this disease.
So, angioplasty and stenting of hemodynamically significantly narrowed renal arteries help combat renovascular hypertension. But the technique also has other positive aspects. It is important to note that timely detection and correction of stenotic lesions of the renal arteries significantly increases the effectiveness of treatment and avoids complications of hypertension. In addition, the natural course of stenotic lesions of the renal arteries (especially with critical degrees of narrowing) in the absence of radical treatment over time can lead to complete closure (occlusion) of the renal artery and loss (shrinkage) of the kidney. Such a kidney ceases to perform its function, which in the long term brings the patient closer to the possible occurrence of renal failure. Thus, this intervention also performs an organ-preserving function.
For timely detection of this disease, all patients with suspected vasorenal hypertension must undergo a duplex scan (Doppler ultrasound) of the renal arteries, based on the results of which further treatment tactics are determined.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC:
Tel., email mail
Ivanov Andrey Gennadievich (head of the department of x-ray surgical methods of diagnosis and treatment, doctor of the highest category in the specialty “endovascular diagnostics and treatment”)