1.General information
Arrhythmogenic (causing arrhythmia) dysplasia/cardiomyopathy of the right ventricle (ARVD, ACM RV) - such a cumbersome name means a dangerous cardiac disease, known since the 18th century, but still insufficiently studied in a number of aspects.
The famous anatomist and materialist thinker of his time, the author of a number of outstanding works on malaria, plague of farm animals, syphilis, and the structure of the brain, the Italian Giovanni Maria Lancisi (1654-1720) was engaged in research, including the cardiovascular system. However, one of his main works, “De Motu Cordis et Aneurysmatibus”, which gave the first clinical description of arrhythmogenic pancreatic dysplasia, was published only posthumously, in 1728. Lancisi described a family disease that appeared in four generations and resulted unexpectedly and fatally (two and a half centuries later, this outcome would be called sudden cardiac death).
Modern nosological definitions of “arrhythmogenic dysplasia”, “arrhythmogenic right ventricular cardiomyopathy” appeared relatively recently, in the late 1970s - early 80s, and in ICD-10 they were classified under the heading “Other heart diseases / Cardiomyopathies”). The essence of this pathology repeats the patterns of many fibrosis, but also has pronounced distinctive features: the parenchymal muscle tissue of the heart, consisting of functional cardiomyocyte cells, degenerates and is replaced partly by fatty, partly by connective (scar) tissue, which inevitably affects the functioning of the myocardium as a whole, – causing, in particular, characteristic irregularities in heart rhythm, which gave the disease its name. The specificity is that the fibrosing process and fatty degeneration are almost always localized in the so-called. “dysplastic triangle” of the right ventricle of the heart muscle, i.e. in the area limited by the apex of the heart, the inlet and outlet tracts of the ventricle.
ACMP of the pancreas is considered a rare disease, but it has been established that it is the second most common cause of sudden cardiac death in young people. This is especially true for athletes, among whom such an outcome often becomes the first, only and last manifestation of the disease. In general, the proportion of ACMP of the pancreas as a cause of sudden cardiac death is, according to various estimates, from 20% to 25%, and in age samples under 20 years old this figure reaches 26%. About 80% of cases of arrhythmogenic right ventricular cardiomyopathy are diagnosed in people under the age of 40 years.
The incidence of ACMP of the pancreas in terms of the general population is estimated differently; Usually data is given at the level of 0.05% -0.5%. In the countries of the Mediterranean basin, the disease is registered much more often: up to 0.8% of the general population. The majority of patients are male.
However, all these data require careful verification and clarification in large samples, which is complicated by the complexity of diagnosis (in many cases, arrhythmogenic pancreatic dysplasia is not recognized and not registered as such) and the relative rarity of the disease.
A must read! Help with treatment and hospitalization!
What happens in the organ with Fontan's disease
Structural abnormalities in this disease occur as a result of lipid impregnation and proliferation of connective tissue in the muscle of the right ventricle. This leads to its progressive expansion and decreased contractility. The left ventricle is affected much less frequently; the interventricular septum is practically not involved. Involvement of the left ventricle in the process is associated with a poor prognosis of the disease.
Mechanisms of destruction of myocardial cells:
- apoptosis (programmed cell death);
- inflammation, increasing fibrosis and loss of contractility;
- fatty replacement of heart cells.
Arrhythmogenic right ventricular dysplasia, autopsy of the heart of a young man who died suddenly while playing basketball.
As a result, the electrical stability of the myocardium is disrupted, and foci of pathological excitation appear in it. They become a source of ventricular arrhythmias.
Ventricular tachycardia that occurs suddenly can cause cardiac death in a young and apparently healthy person.
With further replacement of the myocardium with fatty and connective tissue, the function of the right ventricle suffers and its failure develops. At the final stages of the disease, there is already insufficiency of both ventricles, and the disease takes on the features of another cardiomyopathy - dilated.
2. Reasons
The genetic, hereditary nature of the disease applies to only 30-50% of cases, and the genes responsible for its development have already been identified. In the regional variant of ACMP of the pancreas, known as Naxos Island disease (Greece), fibrofatty degeneration and progressive heart failure are accompanied by congenital abnormalities of the skin and hair (keratoderma, “woolly hair”).
The etiopathogenesis of all other, non-hereditary cases remains essentially unknown. Hypotheses are considered and discussed according to which the degenerative process in the right ventricle of the myocardium is triggered as a result of bacterial or viral infectious inflammation; idiopathic (purely individual) features of intrauterine development; abnormally accelerated apoptosis (premature death of cardiomyocytes after a significantly lower number of cell divisions than normal); spontaneous degeneration of cardiomyocytes into cells of other types (transdifferentiation). However, even if any of these assumptions are confirmed statistically, it will be of little value without understanding the internal reasons: why arrhythmogenic dysplasia starts and develops in some people, while others do not.
Visit our Cardiology page
Diagnosis of arrhythmogenic right ventricular dysplasia
The diagnosis is made when certain criteria are met. To detect them, the following studies are necessary:
- EchoCG;
- MRI of the heart;
- endocardial and myocardial biopsy;
- radioisotope angiography;
- ECG;
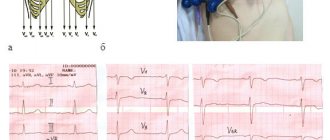
On the ECG of a patient with ARVD: negative T waves in leads V1–V5, arrows indicate epsilon waves.
- daily ECG monitoring;
- electrophysiological study of the heart;
- three-dimensional ECG mapping;
- molecular genetic testing.
Echocardiography for arrhythmogenic dysplasia of the right ventricle, see this video:
The “gold standard” for diagnosis is X-ray contrast ventriculography. During this test, a substance that is impenetrable to X-rays is injected into the heart cavity through a vein. Characteristic signs of the disease are:
- expansion (dilatation) of the right ventricle;
- impaired contractility of individual areas of the myocardium;
- protrusion in the area of affected cardiomyocytes;
- increased trabecularity - an increase in the number of muscle fibers in the cavity near the walls of the ventricle.
Many of these research methods are carried out only in specialized cardiology centers. Therefore, it is important to suspect the disease in time based on clinical data, and if unexplained dizziness, fainting, or palpitations occur, consult a doctor.
CRITERIA FOR DIAGNOSIS OF ARVD
3. Symptoms and diagnosis
The clinical picture of ACMP of the pancreas requires differentiation from many other diseases and conditions in which gradually progressive heart failure is combined with episodes of arrhythmia. As a rule, patients begin to pay attention to increased heartbeat, interruptions in heart rhythm, shortness of breath, then pain in the heart, dizziness, sudden syncope with loss of consciousness (an unfavorable prognostic sign, which is considered one of the possible harbingers of sudden cardiac death). Fatigue increases, the patient tolerates physical activity less and less well.
However, in many cases, the progression of fibrofatty degeneration over a long period of time is not accompanied by any significant subjective sensations or clinical symptoms.
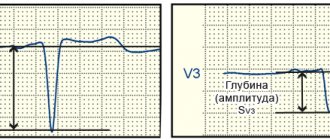
Considering the diagnostic complexity of ACMP of the pancreas, international cardiological associations have made attempts not only to unify terminology, but also to develop reliable recognition and differential diagnostic protocols. Thus, the presence of at least 3% connective tissue and at least 40% adipose tissue in the histological structure of the right ventricle is considered necessary to establish a diagnosis; Electrocardiographic, auscultatory and other diagnostic criteria are also used. For obvious reasons, a family history is required.
As necessary, EEG, echocardiography, stress tests, Holter monitoring, radiography, MRI are prescribed, and if all these methods do not allow an unambiguous diagnosis, it is necessary to resort to invasive endomyocardial biopsy, taking tissue samples for histological analysis.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms of the appearance of arrhythmogenic dysplasia of the right ventricle
Sometimes the disease is asymptomatic for a long time, and its first manifestation may be sudden death.
In other cases, the patient is bothered by episodes of rapid heartbeat and fainting caused by paroxysmal ventricular tachycardia. With a less dangerous ventricular extrasystole, sometimes there is a feeling of interruptions in the heart.
Children and adolescents may complain of dizziness, unexpected attacks of palpitations or severe weakness, and fatigue.
As right ventricular failure progresses, swelling in the legs, heaviness in the right hypochondrium, abdominal enlargement, and weakness appear. If the function of the left ventricle is impaired, shortness of breath during physical exertion, attacks of suffocation in a lying position, and cough occur.
4.Treatment
Etiopathogenetic therapy does not currently exist, and it will not appear until all issues related to the causes and pathogenesis of arrhythmogenic right ventricular dysplasia are finally clarified. The risk of sudden fibrillation and cardiac arrest is reduced by beta-blockers and other antiarrhythmic drugs; Cardiac glycosides, diuretics, ATP inhibitors, etc. are prescribed symptomatically. The effectiveness of such tactical schemes requires additional research. Lifestyle adjustments must be made, and any risk factors and provoking factors are strictly excluded. Some cardiac centers practice radiofrequency catheter ablation as a treatment, but this experience has not yet been studied enough.
There are opinions that the method of choice should be a radical intervention - a heart transplant or, at least, implantation of a cardioverter-defibrillator - however, to other specialists, the risk of possible complications during trans- or implantation seems justified only in cases where the process progresses quickly and manifests itself with obviously threatening symptoms.
Prognosis for the disease
Arrhythmogenic cardiomyopathy is constantly progressing and all types of treatment, except heart transplantation, can only improve the quality of life and reduce the risk of SCD, which is quite high. After diagnosis, about 4-19% of patients die within 5 years. With a successful heart transplant, the prognosis is relatively favorable.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Nekrasa
Graduated from Rostov State Medical University with a degree in General Medicine.