Publications in the media
Superficial thrombophlebitis is an inflammatory disease characterized by the development of thrombosis and reactive spasm of the superficial veins, most often of the lower extremities. Often develops as a complication of varicose veins. Iatrogenic thrombophlebitis of the superficial veins sometimes occurs after venipuncture or venosection.
Localization . The great saphenous vein and its tributaries are most often affected in the upper third of the leg, lower and middle thirds of the thigh. Rare forms: thrombophlebitis of the superficial veins of the mammary gland and anterior chest wall (Mondor's disease), as well as thrombophlebitis of the dorsal vein of the penis.
Classification . Acute, subacute, recurrent; migratory thrombophlebitis (repeated thrombosis of various parts of the superficial veins, most often in the lower extremities); ascending and descending.
Etiology . Phlebitis can develop independently and cause venous thrombosis, or the infection quickly joins the primary thrombosis of the superficial veins. In addition, it can be secondary to vasculitis, for example, periarteritis nodosa and thromboangiitis obliterans (Buerger's disease). Migratory thrombophlebitis can be a marker of carcinoma, most often of the tail of the pancreas. Thrombophlebitis of the dorsal penile vein is usually caused by acute or chronic trauma.
Pathogenesis . Thrombophlebitis develops in the presence of the following conditions: slow blood flow, increased blood clotting, damage to the wall or valves of the veins, and infection.
Clinical picture • Acute thrombophlebitis occurs suddenly, accompanied by an increase in body temperature followed by chills. Along the course of the affected vein, a painful dense infiltrate in the form of a cord is palpated. Over the infiltrate, hyperemia of the skin with compaction of the subcutaneous tissue is possible. Regional lymph nodes are enlarged • The subacute form of thrombophlebitis occurs without acute local inflammatory phenomena, with normal or slightly elevated body temperature in the first days. When walking, moderate pain, general malaise • The recurrent form is characterized by the emergence of a new area of damage to the superficial veins or exacerbation of a previously occurring process • With Mondor's disease, thrombophlebitis is usually localized in the upper anterolateral part of the mammary gland, or spreads from the lower part of the gland through the submammary fold towards costal arch and epigastrium.
Laboratory tests • Leukocytosis with a shift of the leukocyte formula to the left and increased ESR • PTI • Duplex ultrasound scanning can confirm the spread of a blood clot to the deep veins of the limb • With migratory thrombophlebitis, a thorough examination of the digestive organs is necessary to exclude a primary oncological disease. In diagnostically unclear cases, it is recommended to determine the content of CEAg in the blood serum.
Differential diagnosis • Erysipelas • Lymphangitis • Cellulitis • Tendonitis • Rupture of the medial head of m. gastrocnemius.
TREATMENT
Conservative treatment • Bed rest, elevated position of the limb • Elastic bandage helps fix the blood clot in the superficial veins • Locally: compress with Vishnevsky ointment, semi-alcohol compress, heat • Physiotherapy: iontophoresis with thrombolytin (trypsin-heparin complex) • Drug treatment •• Anti-inflammatory therapy: acetylsalicylic acid, NSAIDs (reopyrin, phenylbutazone). Anticoagulants are usually not prescribed, except in cases of spread of the process to the deep venous system •• Recurrent superficial thrombophlebitis - antibiotics •• Acetylsalicylic acid as a weak anticoagulant •• Troxerutin 0.3–0.6 g/day for 2–4 weeks.
Surgical treatment . The Troyanov–Trendelenburg operation is performed in the presence of a blood clot at the mouth of the great saphenous vein (the blood clot is removed).
Complications • Hyperpigmentation of the skin over the affected vein. • Organized thrombus fixed inside a varicose vein. • Thrombophlebitis of deep veins. About 12% of patients with thrombophlebitis of the great saphenous vein above the level of the knee have spread of the thrombus to the deep veins of the limb (through perforating veins or saphenofemoral anastomosis). • PE • Suppurative phlebitis may be complicated by metastatic abscesses or septicemia • Streptococcal lymphangitis
The prognosis is favorable with timely and adequate appropriate treatment. The patient should be informed that the illness may last 3–4 weeks or longer. With varicose veins of the superficial veins of the lower limb, the likelihood of relapse is very high. To prevent it, phlebectomy is recommended.
Synonym . Thrombophlebitis of superficial veins
ICD-10 • I80 Phlebitis and thrombophlebitis
APPLICATIONS
Thrombosis of the superior sagittal sinus is a blockage of the superior sagittal sinus, the only sinus that carries out venous outflow from the dura mater, with a thrombus. Causes : infection, complication of osteomyelitis, dehydration, trauma, tumors. Clinical picture : fever, headache, lethargy, stretching of the veins of the scalp, convulsions, aphasia, hemiplegia; usually occurs acutely. Treatment depends on the cause: antimicrobials, drainage, surgery. Synonym : thrombosis of the superior longitudinal sinus. ICD-10 . G08 Intracranial and intravertebral phlebitis and thrombophlebitis.
Cavernous sinus thrombosis is a disease characterized by infection of the venous canals that carry out venous drainage from the face and orbit. Causes : direct penetration of infection from the eye socket and face. Risk factors : diabetes and immunodeficiency states. Clinical picture : exophthalmos, swelling of the optic nerve nipple, headache, convulsions, septic fever. The prognosis is unfavorable. Treatment : Hospitalization, intensive care, intravenous fluids and antibiotics. Synonym : cavernous sinus syndrome. ICD-10 . G08 Intracranial and intravertebral phlebitis and thrombophlebitis.
Renal vein thrombosis . Causes : abdominal surgery, chronic heart failure, dehydration, kidney disease, decreased renal blood flow. Clinical picture : lumbar pain, dysuria, enlarged painful kidney. The course can be acute or chronic. Treatment : anticoagulants, glucocorticoids. ICD-10 . N28 . 0 Renal ischemia or infarction.
Thrombophlebitis - symptoms and treatment
Therapeutic and preventive measures for thrombophlebitis are complex and can be conservative and surgical. The main objectives are to maximize the elimination of risk factors, reduce and alleviate local symptoms in acute thrombophlebitis, prevent the spread of thrombophlebitis to the deep vein network and prevent venous thromboembolic complications.
Surgical treatment
Not long ago, the gold standard for the treatment of ascending thrombophlebitis was crossectomy (Troyanov-Trendelenburg operation), but practice results have shown that this method of surgical intervention is the most traumatic and life-threatening for patients.
When the process goes beyond the sapheno-femoral or sapheno-popliteal anastomosis, thrombectomy is performed from the main veins. Surgery can be performed using regional anesthesia or intubation endotracheal anesthesia. The preference for thrombectomy method depends on the level of location of the proximal part of the thrombus.
In case of perforator thrombosis, thrombectomy from the perforator vein is performed. In case of embolic thrombosis of the femoropopliteal segment, ligation of the superficial femoral vein (SFE) is indicated.
In case of embolic-dangerous iliocaval thrombosis, plication of the inferior vena cava is performed.
The figure shows the implantation of a vena cava filter into the inferior vena cava, the indication for which is embolic iliocaval thrombosis.
Laser treatment
According to the latest revised clinical guidelines, endovenous laser coagulation (EVLC) is a low-traumatic and safe technique for ascending thrombophlebitis. This method can be used to operate on any category of patients. As a rule, surgery is performed under local tumescent anesthesia.
Conservative treatment
Today, for existing indications, the most effective method will be anticoagulant therapy. In medical practice, it is customary to distinguish between direct-acting anticoagulants, which help reduce thrombin activity in the blood, and indirect-acting anticoagulants, which prevent the formation of prothrombin in the liver. Low molecular weight heparins belong to the group of direct-acting anticoagulants. These include medications such as Enoxaparin sodium (Anfibra, Clexane, Hemapaxan, Lovenox), Dalteparin (Fragmina) or Tinzaparin, which must be administered subcutaneously 1-2 times during the day. The use of low molecular weight heparins results in maximum effectiveness and minimal side effects. Indirect anticoagulants are Warfarin derivatives, which require special caution and a high degree of laboratory control (INR). Currently, the greatest interest is in drugs that do not require laboratory monitoring of INR and with lower risks of complications, for example, such as Xarelto (Rivaroxaban) or Pradaxa.
In addition, the patient is prescribed long-term wearing of compression hosiery and auxiliary pharmacotherapy, phlebotonic drugs (Detralex; Venarus; Phlebodia 600), etc. It is also advisable to prescribe non-steroidal anti-inflammatory drugs and local treatment.
Treatment of thrombophlebitis of superficial veins and acute thrombophlebitis
Recently, international consensus has accepted the equality between the terms “acute thrombophlebitis” and “thrombophlebitis of the superficial veins”, which determines the commonality of pathogenetic mechanisms, complications and treatment tactics.
Physiotherapeutic treatment
Intermittent pneumocompression is a physiotherapeutic method of massaging tissue using special multi-chamber cuffs with different operating pressures. This technique has excellent lymphatic drainage properties, helps reduce swelling and can be used for thrombophlebitis of the veins of the lower extremities.
Electromyostimulation using the VENOPLUS device - this patented technique consists in the fact that electromyostimulation leads to muscle contraction and activation of the muscle-venous pump. It can also be used for thrombophlebitis of the veins of the lower extremities.
Gymnastics for thrombophlebitis
This disease poses a threat to life if a blood clot breaks off, so gymnastics is contraindicated.
Leeches for thrombophlebitis
Currently, the first line of therapy is the use of low molecular weight heparins. Hirudotherapy has a much lower effect.
Ointments for thrombophlebitis
The use of ointments is possible in the complex treatment of thrombophlebitis. NSAIDs are used in the form of ointments to relieve pain. Such ointments include Fastum Gel, diclofenac, ortofen and others. It is also possible to use ointments with heparin (Lioton, hepatrombin).
Nutrition for thrombophlebitis
Nutrition does not affect the course of thrombophlebitis. It is worth adjusting the diet only if the disease occurs against the background of obesity.
Can folk remedies help?
Decoctions, tinctures and compresses have no proven effectiveness and therefore cannot be recommended for the treatment of thrombophlebitis. Thrombophlebitis is a disease that can threaten the patient’s life and therefore requires immediate and adequate treatment.
Rehabilitation
Rehabilitation usually takes place at home. Compliance with any special regime is not required. If the patient smokes, he should stop smoking if possible.
Acute ascending thrombophlebitis (AATT) is the most common emergency surgical pathology of the vascular system, for which patients go to clinics and are hospitalized [1-11]. According to some data, AVTF develops during life in 20-40% of the population [12]. In the United States, ABTF is reported in approximately 125,000 people per year [8, 13]. F. Anderson et al. [14] believe that this number is higher and ranges from 56 to 160 people per 100,000 inhabitants per year.
The most common risk factor for the development of thrombophlebitis is varicose veins of the lower extremities, occurring in 68-95% of patients [4, 7, 10, 15-17]. Significant risk factors include prolonged immobilization, trauma, intra- and postoperative period, age over 60 years, obesity, tobacco smoking, history of deep vein thrombosis or VTPS, pregnancy, postpartum period, autoimmune diseases, use of oral contraceptives, hormone replacement therapy , hypercoagulation [16-25], malignant neoplasms (acute thrombophlebitis develops in 13-18% of cancer patients) [26-28], non-tumor systemic diseases (9.5%) or thrombophilia (48%) [29].
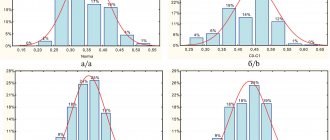
In 60-80% of cases, thrombophlebitis develops in the territory of the great saphenous vein (GSV), in 10-20% of cases - in the territory of the small saphenous vein (SSV). No differences were found in the incidence of lesions in the right or left lower extremity. In 5-10% of cases, bilateral damage to the superficial veins is detected. More often, the thrombotic process affects the tributaries of the GSV or IPV than their trunks [21, 30-34].
For a long time, AVTF was considered as a disease with a benign course and rarely leading to complications, and the main task was seen in the relief of symptoms that develop with this complication and significantly worsen the patient’s well-being and his quality of life [35-37]. In reality, this is not the case, since a serious threat to the life and health of patients is not thrombophlebitis itself, but the associated spread of thrombosis from the saphenous to the deep veins. Most often (from 1 to 44% of cases) a thrombus from the GSV spreads to the common femoral vein through the saphenofemoral anastomosis, less often (from 0.2 to 1% of cases) - from the SSV it spreads to the popliteal vein through the saphenofemoral anastomosis. The rarest route for thrombosis to spread to deep veins is through incompetent perforating veins [10, 38, 39].
The frequency of detection of deep vein thrombosis in ARVT, according to various sources, ranges from 6.8 to 40% [40-43]. Typically, deep vein thrombosis occurs in the same lower extremity as the DVT [44–46], but in some cases (up to 2%) deep vein involvement occurs in the contralateral limb [41].
The greatest danger is posed by the so-called ascending forms of AVTF (40-60% of cases); it is with them that the threat of deep vein thrombosis and pulmonary embolism (PE) is associated, and justifiably. Due to the difference in the diameters of the GSV and the common femoral vein, the apex of the thrombus in saphenofemoral thrombosis in most cases has a non-occlusive, floating nature, which is a prerequisite for the occurrence of pulmonary embolism [6, 8, 31, 32, 38, 47, 48].
In real clinical practice, the situation is further aggravated by the fact that the spread of the thrombotic process from the distal parts of the limb in the proximal direction is often asymptomatic, and often the first sign of the transition of thrombosis to the deep venous system is the manifestation of pulmonary embolism [1, 4, 8, 49]. Symptoms of pulmonary embolism can be detected in 5.6-28% of patients with AVTP [10, 34, 39, 50]. Some researchers [45, 48, 51] claim that the incidence of pulmonary embolism in patients with VTTF is higher and reaches 33.3%. Moreover, using lung perfusion scintigraphy, disturbances in pulmonary blood flow are detected in 50% of cases of OVTP, i.e. a significant proportion of cases of pulmonary embolism are subclinical in nature and are not diagnosed when patients visit doctors [52-54]. In particular, F. Verlato et al. [48] when examining 21 patients with ascending thrombophlebitis without damage to the deep veins, they found PE in 7 patients, although clinical symptoms indicating this complication were present in only 1 patient [48]. Mortality from pulmonary embolism, the source of which was varicothrombophlebitis, according to M.F. Muravyov [50], reaches 10%. R. Zollinger et al. [55] reported a 1.5% incidence of fatal pulmonary embolism in patients with superficial thrombophlebitis.
It is not so rare that the thrombotic process in the saphenous veins is recurrent in nature, which leads to long-term, and sometimes permanent, disability [17, 56, 57]. The average recurrence rate of AVTF is 18% over 15 months of follow-up. Reflux from the deep venous system increases the risk of relapse to 33%, a permanent state of hypercoagulability - to 42% [58].
Thus, the doctor who solves the problem of adequate management of a patient with AVTF faces not only, and even not so much, the task of eliminating inflammatory-thrombotic changes in the saphenous veins and the associated clinical symptoms. The task of preventing the transition of thrombosis to the deep venous system should be considered more important. There are two fundamentally different approaches to solving this problem: conservative and surgical. The first involves the use of anti-inflammatory and phlebotropic drugs to relieve phlebitis, as well as anticoagulants to suppress thrombus formation. The second approach, surgical, aims to eliminate the danger of thrombosis transferring to the deep venous system by eliminating the very possibility of such a transfer, i.e. by eliminating the anastomosis of the superficial and deep veins.
Despite the fact that the problem of ARVT has attracted the attention of surgeons for more than 100 years, to date there has been no consensus on the choice of tactics to prevent deep vein thrombosis and PE in patients with ARVT [46, 59, 60]. A number of authors believe that such patients should be managed conservatively. They allow the possibility of surgery only if there is a threat of thrombosis spreading directly to the saphenofemoral anastomosis [14, 21, 31, 35, 38, 47, 50, 56, 61-66, 92, 144]. Others choose active tactics for the treatment of varicothrombophlebitis and give preference to surgical treatment in the scope of the Troyanov-Trendelenburg operation (crossectomy). A third treatment option, radical phlebectomy, is also being discussed [39, 57, 67, 68]. It is surgical intervention for decades, and still, by most surgeons that is perceived as synonymous with the effective treatment of AVTF. But is the faith of surgeons in the possibilities of surgery for acute thrombophlebitis justified?
Surgical interventions.
The most famous and common operation is estial ligation of the GSV with all its tributaries (crossectomy, or Troyanov-Trendelenburg operation), the purpose of which is to prevent the spread of thrombosis into the deep venous system with the subsequent development of pulmonary embolism.
Although this intervention may well claim to be the “gold standard”, even its indications are controversial. Some authors believe that it is necessary when clinical manifestations reach the level of the knee joint [69]. A number of experts suggest performing a crossectomy when the level of thrombophlebitis extends to the upper third of the thigh [41, 50, 70-74]. Other indications for emergency ligation of the GSV are considered to be signs of a thrombotic process in the area of the inguinal fold [8, 57, 75]. E.L. Margalis et al. [76], when determining the indications for surgery, did not take into account the level of thrombophlebitis at all - in fact, the reason for intervention was the very fact of the development of this complication. This position can be supported, in particular, by reports of cases of pulmonary embolism, when the clinically detectable level of thrombophlebitis did not reach the upper third of the thigh [32, 70].
Despite the fact that crossectomy is aimed at preventing deep vein thrombosis and pulmonary embolism in patients with ARVT, this operation is often accompanied by the development of these very complications. Thus, according to H. Kock et al. [57], who examined 44 patients who underwent proximal ligation of the GSV, 2 of them developed thrombosis of the stump of this vessel, which led to PE in 1 patient, and thrombosis of the femoral vein occurred in 1 patient. F. Lozano et al. [77] in a group of 30 patients who underwent crossectomy, recorded 1 (3.3%) relapse of acute thrombophlebitis and 2 (6.7%) - submassive pulmonary embolism. A number of authors [20, 33, 40, 41, 55, 56, 71, 75, 78-86] report that pulmonary embolism after ostial ligation of the GSV occurs with a frequency of up to 8%, and relapse of varicothrombophlebitis develops in 2-4.3% cases. The incidence of PE in real practice is probably higher than reported, since most studies report only clinically manifested PE [87]. As for the frequency of recurrence of thrombophlebitis, in the literature [2, 4, 17, 34, 88] one can find indications of significantly higher figures - 50-75.4%.
In patients who have undergone crossectomy, common postoperative complications are also recorded - wound suppuration (12.8-16.5%), seromas, hematomas [31, 57, 74, 77, 88-90]. Although there are no reports in the available literature of cases of transection or injury of the femoral vein, clinical experience suggests that such intraoperative complications do occur, although they are not the subject of widespread discussion.
Along with palliative surgery aimed at preventing the transition of the thrombotic process through the saphenofemoral anastomosis and preventing pulmonary embolism, stem and even radical phlebectomy for varicothrombophlebitis are currently performed. The latter involves the removal of all varicose veins (thrombosed and non-thrombosed), as well as dissection (ligation, coagulation) of insufficient perforators [3, 10]. Some surgeons [4, 6, 17, 34] recommend two-stage surgical treatment. First, estial ligation of the GSV is performed, then, after the inflammatory process subsides, radical phlebectomy is performed.
Radical intervention is performed when the disease lasts no more than 14 days. First, if necessary, the embolic thrombus is removed from the femoroiliac segment or perforating vein. Then crossectomy and all other stages of the intervention are performed [3].
According to D. Son [91], in patients who underwent radical phlebectomy, recurrence of thrombophlebitis on the operated lower limb occurred in 9.8% of cases 3-12 months after surgery. In the immediate postoperative period, 2.3% of patients developed deep vein thrombosis of the leg, 1.2% had necrosis of the skin edges of the wound on the leg, and 0.6% had lymphorrhea from a postoperative wound in the groin area. In the long-term postoperative period, PE was diagnosed in 0.6% of cases.
After radical phlebectomy, in 4-50% of cases, damage to the cutaneous nerves occurs, manifested by hyposthesia, hypersthesia, and parasthesia in the area of the lower third of the leg along the medial surface [92-96].
Despite the fact that radical phlebectomy eliminates the very cause of varicothrombophlebitis - varicose veins, it also has a sufficient number of contraindications and does not exclude the occurrence of postoperative complications, which is why the possibilities of performing this operation are limited. Emergency surgery results in a 3-fold increase in costs and is associated with a higher likelihood of pulmonary embolism [60].
Thus, an objective analysis of literature data allows us to speak about an insufficiently substantiated attitude towards surgical prevention of deep vein thrombosis and pulmonary embolism in VTHF as a reliable and safe approach to the management of these patients. The incidence of pulmonary embolism after crossectomy is quite comparable to the incidence of this complication in non-operated patients with AVTP, and radical phlebectomy cannot be considered the means of choice in all cases, since intervention on thrombosed veins is traumatic and requires general or regional anesthesia.
Could a more restrained, conservative approach be an alternative to traditional surgical tactics?
Conservative treatment.
Its goals are to stop the process of thrombus formation and the spread of thrombosis, as well as to relieve inflammatory changes in the venous wall and surrounding tissues, which eliminates pain [6, 25, 41, 48, 59, 65, 66, 82, 84, 97, 98]. The regimen for patients with AVTF should be active; it is considered a serious mistake to prescribe bed rest [99], which is the main risk factor for the development of deep vein thrombosis. During bed rest, the activity of the muscular-venous pump of the lower leg, which provides intense blood flow in the deep veins, is limited. It is not surprising that in the study by S. Hill et al. [99], who used bed rest and immobilization of the affected limb in patients with AVTF, found such a large number of cases of increasing levels of GSV thrombophlebitis (56.6%) and the transition of the thrombotic process to the common femoral vein (26.6%). Activation of patients with AVTF helps to improve the fibrinolytic activity of the blood, which contributes to thrombus reduction [3, 20, 68, 100-102].
Elastic compression of the lower extremities is one of the most important components of the treatment of acute thrombophlebitis. As a rule, elastic bandaging is initially used. For these purposes, medium-stretch bandages are used [3, 6, 101]. As the thrombotic and inflammatory processes subside, after about 7-10 days, medical knitwear [3, 65, 66] of 2nd compression class becomes the best alternative to bandaging. The use of elastic compression even after recovery helps patients avoid relapse of the disease [3, 25, 34, 48, 102].
One of the central places in the complex treatment of acute thrombophlebitis is occupied by systemic pharmacotherapy. According to a number of experts [3, 51, 65, 66, 82, 84, 85, 103-105], patients with acute thrombophlebitis need to be prescribed non-steroidal anti-inflammatory drugs. They quickly stop inflammation, provide the necessary pain relief, and indirectly affect hemostasis, having a disaggregant effect. They are prescribed on average 2-3 times a day and are usually used for no more than 7-10 days.
According to a number of researchers [3, 7, 17, 39, 50, 106], hydroxyethylrutosides (venoruton, troxerutin, troxevasin) are effective treatments for AVTF. The dose of the drug should be at least 1200 mg/day, and the average duration of treatment should be 2-3 weeks [3]. A good effect is achieved by micronized purified flavonoid fraction (detralex) at a dosage of 3000 mg per day for 4 days, then 2000 mg per day for the next 3 days [3]. Multienzyme preparations (wobenzym, phlogenzyme) are used. At the same time, taking a large number of tablets at a strictly defined time and the high cost of these drugs limit their widespread use [3, 6, 65, 66, 82, 103-105, 107].
Until now, in the literature [99] one can find indications for the prescription of antibacterial therapy for the treatment of acute thrombophlebitis. At the same time, bacteriological examination of blood clots removed from the affected veins during surgery showed a low level of contamination. In the vast majority of cases, thrombophlebitis is aseptic in nature (with the exception of rare cases of septic course) and does not require antibiotic therapy, in addition, many antibiotics cause hypercoagulation and thus can lead to the progression of thrombus formation [3, 4, 34, 65, 71, 108, 109 ].
In the first 2-3 days of the disease, it is recommended to use local hypothermia. It provides a good analgesic effect, since cooling the tissues inhibits the processes of inflammation in them [3, 49, 50, 110]. For local treatment, various gels are used, most often containing only heparin. The combination of heparin-containing and non-steroidal anti-inflammatory local agents can achieve a good anti-inflammatory effect [3, 85].
All of the listed methods and means of treatment are certainly effective, but they make it possible to achieve a greater degree of relief of inflammatory phenomena in thrombosed saphenous veins. One can hardly count on the fact that local agents, phleboprotectors, and anti-inflammatory drugs can have any significant effect on the coagulation potential of the blood and prevent the process of increasing thrombosis. Anticoagulant therapy can be considered the only effective means for this. The feasibility of using anticoagulants in the treatment of patients with ARTF is the subject of active debate.
According to many authors [8, 38, 59, 60, 84, 82, 101, 106, 111-114], it is impossible to prevent the spread of the thrombotic process in acute thrombophlebitis without their use. D. Chengelis et al. [122] in patients with thrombophlebitis of the GSV of the thigh who did not receive anticoagulant therapy, deep vein thrombosis was found in 24% of cases as a result of the process passing through the saphenofemoral anastomosis. In another study [51], in the first 2 weeks of treatment in patients receiving placebo, the incidence of deep vein thrombosis was 30.6%.
The recently completed international multicenter trial CALISTO [124] demonstrated that anticoagulant therapy in patients with varicothrombophlebitis is effective and prevents the spread of thrombosis and the development of pulmonary embolism. The factor Xa inhibitor fondaparinux was used as an anticoagulant and compared with placebo. The incidence of clinically significant PE was 0.2% compared with 1.3% in patients not receiving anticoagulants.
There is no single point of view on which drugs to use and in what dosage. In a study of the effectiveness of low molecular weight heparin (enoxaparin) in prophylactic (40 mg once daily) and therapeutic (1.5 mg/kg once daily) dosages, the incidence of thrombosis in the superficial and deep venous system of the lower extremities in the first 2 weeks of treatment was 8.3% in group 1 and 6.9% in group 2 [51].
On the other hand, A. Marchiori et al. [82] in 20% of cases, when using unfractionated heparin in a prophylactic dosage (5000 units subcutaneously 2 times a day) for 4 weeks, progression of acute thrombophlebitis or deep vein thrombosis was observed, while such complications developed only in 3.3% of patients who received unfractionated heparin in a therapeutic dosage 2 times a day for 2 weeks. The authors believe that the use of therapeutic doses of low molecular weight heparins will also provide good results.
In a study by G. Belcaro et al. [41] after 6 months of follow-up, the incidence of deep vein thrombosis was 7.7% in the control group (use of compression stockings only), while in the other three groups (knitwear and prophylactic doses of low molecular weight heparins; stockings and prophylactic doses of unfractionated heparin; stockings and vitamin K antagonists) there was no thrombosis.
E. Kalodiki et al. [72] also advocate the use of low molecular weight heparins in the treatment of AVTF, explaining that the incidence of disease relapse and its complications is lower in patients treated with anticoagulants than in patients treated without their use.
J. Titon et al. [84] believe that there is no difference in effectiveness between a fixed dose of low molecular weight heparins and a weight-based dose.
Treatment of AVTF with low molecular weight heparins in a prophylactic dose should last, according to H. Bűller et al. [59] and M. Di Nisio et al. [111] at least 4 weeks. A similar point of view is shared by S. Kearon et al. [60], who prescribe prophylactic or intermediate doses of anticoagulants for 4 weeks.
As an alternative, they also offer the possibility of prescribing vitamin K antagonists from the 5th day of treatment with unfractionated or low molecular weight heparins. The duration of taking indirect anticoagulants should, in their opinion, be 4 weeks. In the literature [66, 116], one can find proposals to continue therapy with indirect anticoagulants for 3 months after a short initial course of low molecular weight heparins.
The recurrence rate of AVTF after treatment with anticoagulants ranges from 7.5 to 15-20% [36, 40, 74, 81].
Despite the ambiguity of opinions about which anticoagulants and in what dosages should be used for the treatment of acute thrombophlebitis, the use of anticoagulant therapy to prevent deep vein thrombosis and pulmonary embolism seems pathogenetically justified and justified. The data available in the world literature allow us to speak of at least equal effectiveness of the conservative and surgical approaches to the management of patients with ARTF. Moreover, if in publications devoted to surgical prevention of deep vein thrombosis using crossectomy, the development of pulmonary embolism is regularly reported as a complication of the operation, and not as a result of AVTF, then in works on anticoagulant therapy, cases of pulmonary embolism are practically not mentioned. At the same time, it is impossible to talk about proven advantages of this or that approach today. A search in the MEDLINE, EMBASE, Cochrane databases for literature data on treatment tactics for patients with ascending thrombophlebitis led us to an amazing conclusion: despite a nominally significant number of works devoted to this problem, the number of high-quality comparative studies that meet the requirements of evidence-based medicine is extremely small [41, 77, 82, 84, 102]. Despite the rapid development of the evidence base for the treatment of chronic venous diseases, such pathology as CVVT has found itself on the sidelines of scientific interest of the world phlebological and surgical community. In fact, the approach to the management of these patients to this day is empirical in nature and largely depends on individual preferences or the attitudes of surgical schools, which, of course, cannot contribute to finding the right solution to the problem. In our opinion, there is a need for an in-depth study of the issues raised in this literature review.
Conflict of interest
absent.
Deep vein thrombosis
For the development of the disease, a combination of several factors is necessary:
- damage to the internal lining of the venous wall as a result of exposure to a mechanical, chemical, allergic or infectious agent;
- violation of the blood coagulation system;
- slowing down blood flow.
Under certain circumstances, blood viscosity increases. If there are obstacles to the normal flow of blood on the walls of the vein, the risk of blood clots increases. A small blood clot that forms on the venous wall causes inflammation and further damage to the vein wall, which causes the formation of other blood clots.
The occurrence of deep vein thrombosis is facilitated by congestion in the veins of the lower extremities. The cause of stagnation is immobility or inactivity of a person for a long time. Triggering factors for deep vein thrombosis:
- injury, surgery, excessive physical stress;
- infection;
- prolonged immobility in conditions after surgery, neurological and therapeutic diseases;
- period after childbirth;
- taking oral hormonal contraceptives;
- malignant tumors (especially cancer of the stomach, lungs and pancreas);
- DIC syndrome.
The risk of developing the disease increases with prolonged immobile position with legs down. Thus, in the West there are the terms “economy class syndrome” and “television thrombophlebitis”. In the first case, we are talking about people who developed deep vein thrombosis after a long flight. The second is about elderly patients who developed the disease after sitting in front of the TV for a long time. In both cases, the trigger factor was a long stay in a sitting position with bent legs, which creates obstacles to normal venous outflow.
The return of blood through the veins is largely ensured by muscle contraction. After operations and with some chronic diseases, the patient remains practically motionless for a long time. As a result, congestion develops in the lower extremities, leading to deep vein thrombosis.
When taking oral contraceptives, blood diseases, and malignant tumors, thrombosis is largely due to hypercoagulation (increased blood clotting). In some cases, impaired blood flow in the deep veins may indicate Buerger's disease (thromboangiitis obliterans of allergic origin).
As a rule, deep vein thrombosis develops in the lower extremities. However, deep vein thrombosis in the arm area is sometimes observed, which occurs when exposed to the following triggering factors:
- catheterization of veins of the upper extremities. A catheter located in a vein for a long time causes irritation of the venous wall and leads to the formation of a blood clot;
- implanted cardiac fibrillator or pacemaker;
- malignant neoplasm in the vein area;
- excessive load on the upper limbs in athletes (baseball players, swimmers, weightlifters). The disease develops due to compression of the deep veins of the upper extremities by trained muscles of the shoulder girdle.