The article will present the Braunwald classification of unstable angina.
With ischemic heart disease, angina attacks almost always occur. Severe pain develops when the myocardium begins to lack oxygen. When the syndrome develops against the background of physical activity, we are talking about stable angina pectoris, which accompanies increased heart activity. However, the following situations also occur: severe symptoms in the form of painful pressure in the chest, burning and suffocation are in no way related to the activity of the heart muscle. An anginal attack can strike a person suddenly, and it is impossible to predict its occurrence. In this case we are talking about unstable angina. In accordance with the tenth edition of the International Classification of Diseases, pathology refers to diseases of the circulatory system and has its own code 120.0.
Braunwald's classification of unstable angina will be presented below.
Stable and unstable angina
The very name of unstable angina characterizes the complex of symptoms that arise. The condition can manifest itself without reference to physical activity or other provoking factors. This is precisely the main difference between the pathology in question and stable type angina.
Stable angina is characterized by the presence of a certain set of provoking factors:
- Emotional stress.
- Unfavorable weather with snow, rain, cold wind.
- Established boundaries for physical activity (for example, walking at a fast pace for a distance of more than half a kilometer, climbing stairs higher than the first floor).
Stable angina can have one of four functional classes, each of which has certain permissible levels of physical activity and its own degree of severity of clinical symptoms.
An attack of stable angina stops with rest, can last a maximum of 15 minutes, and is effectively stopped by using Nitroglycerin.
With unstable angina, there is a great danger to the patient’s life, since it is impossible to predict its occurrence and clinical picture, there is no way to determine the permissible level of stress for the patient, and it is difficult to identify provocative factors. Any of these attacks occurs suddenly, is unpredictable in its manifestation, threatens the onset of myocardial infarction, and the patient may die from sudden cardiac arrest. In this case, the symptoms are more severe. An attack can last up to half an hour, and Nitroglycerin is not always effective.
Typical signs of Prinzmetal's angina
New York cardiologist M. Prinzmetal described a type of angina pectoris in 1959, which is included in the modern classification of unstable forms of angina pectoris. In pathogenesis, great importance is attached to the increased tone of the vagus nerve.
Features of the clinic:
- occurs more often in young men;
- attacks of pain occur at rest, there are characteristic ECG changes;
- patients do not complain of pain during physical activity and tolerate it well;
- attacks often occur in the morning rather than during the day or at night;
- good effectiveness in treatment with drugs from the group of nitrates and calcium antagonists.
The prognosis of this form is unfavorable due to the high probability of transition to acute myocardial infarction.
Causes of development of unstable angina
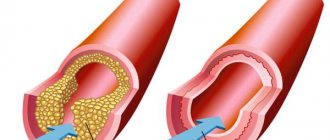
An attack in coronary artery disease occurs when a prerequisite is present - the patient has a violation of the coronary circulation and narrowing of the arteries. Excess cholesterol settles on the vascular walls, atherosclerotic plaques appear, as a result of which the lumen of the artery decreases. Thus, not enough blood flows to the heart. In such conditions, the myocardium begins to work more intensely to replenish the insufficient level of blood supply, but the situation only gets worse. This is due to the fact that the heart, during intense activity, requires an even greater amount of oxygen, which comes exclusively from the blood.
When arterial patency deteriorates by more than 50%, hypoxia increases, which reaches critical limits. Metabolic processes begin to disturb the cells, which is accompanied by pathological changes in intracellular structures. At such moments a person experiences unbearable angina pain. Due to a prolonged attack, tissue necrosis begins and spreads, resulting in myocardial infarction.
IHD and angina pectoris (ICD code 10 I20) develops when the heart has an acute need for large portions of oxygen (stress, physical activity), and damaged coronary vessels are not able to supply the heart muscle with a sufficient volume of blood.
When an atherosclerotic plaque grows to an impressive size, there is a possibility of a violation of its integrity. This happens in cases where there are a lot of fat deposits and not enough collagen, and the vascular wall is inflamed or the blood has increased viscosity. The detached part of the plaque is glued together by platelets, resulting in the formation of a blood clot that can partially or completely block the arterial lumen. This is the main cause of unstable angina. Such blood clots can migrate and penetrate into any part of the coronary vessels.
Another reason for the development of coronary artery disease and angina pectoris (ICD code 10 I20) pathology is sudden spasms of the coronary vessels that occur regardless of physical activity. In this case, arteries that are not affected by atherosclerosis can narrow. A similar situation is typical for vasospastic angina (Prinzmetal), which is a rather rare pathology.
Mechanism of pathology
The blood supply to the heart muscle requires a constant supply of sufficient blood through the coronary arteries. The heart's need for oxygen changes depending on the conditions: physical activity, complete immobility, excitement, intoxication of the body due to infectious diseases.
In contrast to the calm state, tachycardia occurs (increased heart rate). It requires more energy, which means oxygen consumption increases, since the heart muscle cells “extract” calories for themselves only in its presence.
If the patency of the coronary arteries is good, blood flows in sufficient quantities to compensate for the necessary costs. What happens if one or all arteries are narrowed? The working heart will experience a state of “hunger”, tissue hypoxia. Clinical symptoms can be called a “cry for help.”
Provoking factors
In addition to the main reasons for the development of unstable angina attacks, experts identify some additional factors that can increase the risk of severe exertional angina. Among them:
- Diseases not related to the heart (diabetes mellitus, pathological changes in the thyroid gland, iron deficiency anemia).
- Pathologies of a cardiac nature (heart defects, hypertrophic cardiomyopathy, condition after a heart attack, chronic myocardial failure).
- The harmful effects of ethyl and tobacco tar.
- Progressive hypertension.
- Strong mental stress, stressful situations, strong emotionality.
- Increased vascular susceptibility to the effects of vasoactive substances, such as serotonin.
- Increased cholesterol levels in the blood.
- Morphan's disease.
- Unfavorable heredity.
- Obesity.
- Insufficient rest, disturbances in night sleep.
- Physical inactivity.
- Excessive physical activity.
What symptoms and signs are used to determine unstable angina?
Unstable angina has several common symptoms with the stable form of this disease. Among them are:
- pain in the chest area, maybe a little to the left, the patient feels as a squeezing, pressing, less often burning pain, which radiates to the left half of the body (arm, bottom of the shoulder blade, jaw);
An attack of angina may occur in the absence of obvious exertion
- the patient is haunted by the fear of death;
- sweating increases;
- dizzy;
- the patient is suffocating, lacking air;
- breathing does not become rapid.
What symptoms distinguish an unstable form of angina from a stable form? In unstable form:
- there are frequent repetitions of painful attacks;
- their duration increases to a quarter of an hour or longer;
- the pain is constantly getting worse;
- pain occurs both at rest and during exercise;
- pain is not always relieved by Nitroglycerin; in some cases, an increased dose of the drug is required.
Symptoms of rest angina
An attack of anginal pain with angina at rest develops with complete physical calm, most often at night or early in the morning. From a sudden attack, the patient is forced to wake up from sudden suffocation or a feeling of tightness in the chest. An attack of angina at rest is accompanied by the following symptoms: a state of increased anxiety, anxiety, fear of death. The pain is intense, localized behind the sternum, has a compressive, pressing nature, spreading to the jaw, left arm, and shoulder blade.
Possible complications
Untreated angina can cause:
- sudden ventricular fibrillation with fatal outcome;
- acute myocardial infarction;
- acute failure of the heart muscle with pulmonary edema;
- thromboembolism of the pulmonary arteries.
Therefore, an increase in attacks and the appearance of unusual symptoms are important reasons for urgent medical attention.
When referred for inpatient treatment, refusal is considered as the patient’s responsibility for his own life.
Braunwald classification of unstable angina
What is this classification? On what principle is it built?
The most widely used classification is the system of Evgeniy Braunwald. In accordance with it, several classes and levels of pathology are distinguished:
- Class “A” has secondary angina pectoris. Symptoms of the pathology in this case develop under the influence of factors of extracoronary origin, which contribute to the worsening of ischemia: strong emotional outbursts, difficult to treat hypertension, hypotension, instability of the heart rate, infectious attack, fever, anemia. How else are heart diseases classified according to Braunwald?
- Class “B” includes primary angina syndromes. They develop against the background of cardiac pathologies and disorders in the coronary circulatory system.
- According to the Braunwald classification of unstable angina, class “C” is a pathology that is diagnosed against the background of a myocardial infarction (during the first two weeks after it).
Classes of unstable angina, in accordance with this classification, reflect the circumstances of the development of ischemic symptoms, characterized by an unstable manifestation.
The Braunwald classification table for unstable angina is presented in the article.
Causes
Unstable angina has the same causes as all manifestations of myocardial ischemia:
- Damage to the coronary vessels by the atherosclerotic process when the diameter is narrowed by ½. Risk factors should be taken into account here (age after 45 years, predominantly male gender, presence of hypertension, diabetes mellitus, cigarette smoking, alcohol dependence).
- Thrombosis of cardiac vessels with increased blood clotting, decreased blood flow speed (heart failure), thromboembolism from various sources.
According to cardiologists, it is the addition of thrombosis that plays a major role in the instability of vasoconstriction. This possibility increases in patients with thyrotoxicosis and anemia.
Morning jogging can cause pain
Classification depending on the severity of the attack
The pathology is also classified into groups that characterize the severity of the resulting anginal attack:
- The first group includes angina pectoris, which was recorded for the first time within a month before the day the patient consulted a doctor. Such angina pectoris manifests itself stably in conditions of physical activity.
- The second group includes subacute syndromes. The attacks that occur have a more severe course and can manifest themselves at rest. Occurs within a month before contacting a specialist, with the exception of the last two days.
- Angina pectoris of the third group is characterized by acute manifestation of symptoms. Angina pain occurs without reference to physical activity during the last two days.
Many people are interested in what it is - angina pectoris. Its symptoms are very unpleasant. A sudden attack of acute pain in the chest in most cases is a sign of chronic angina pectoris (other names are angina pectoris, acute coronary insufficiency, angina pectoris).
It is the paroxysmal nature of the painful sensations that makes it possible to accurately diagnose the disease. Angina pectoris is considered a form of cardiac ischemia. The most serious complication of the disease is myocardial infarction.
Case from practice
A 56-year-old man came to the emergency department with complaints of burning pain behind the sternum and palpitations.
During the interview, it turned out that he had been experiencing chest discomfort for 2 days when lifting weights (the patient attributed the symptom to heartburn) and walking at an accelerated pace. There were no attacks of tachycardia before. On the electrocardiogram: atrial fibrillation with a contraction frequency of about 130 beats per minute, oblique depression of the ST segment up to 2 mm in leads II, III, aVF. The patient was hospitalized in the intensive care unit with a diagnosis of acute coronary syndrome without ST segment elevation. The staff took tests and started drug treatment. After the administration of Nitroglycerin, the pain decreased. According to the GRACE scale, the score was 150 points. Coronary angiography was performed, which revealed a stenosis of the right coronary artery of up to 90%, and therefore a stent was implanted in the patient. After the procedure, sinus rhythm spontaneously returned. Markers of myocardial necrosis were not elevated, which made it possible to exclude a heart attack. Formulation of the final diagnosis: IHD. Unstable angina IIIB according to Braunwald. Stenosis of the right coronary artery up to 90%.
Surgery: RCA balloon angioplasty with stent installation. Complication of the underlying disease: AHF 0. New atrial fibrillation, spontaneous restoration of sinus rhythm.
Symptoms of unstable angina
There is no difference between the symptoms of different types of angina. For any type of pathology, the patient indicates the manifestation of the following symptoms:
- Sharp jumps in blood pressure.
- Nausea.
- Weakness.
- Dizziness.
- The appearance of anxious thoughts.
- Increased heart rate.
- Increased sweating.
- Feeling of suffocation.
- Pain in the chest, heart, having a compressive nature.
- Pain in the lower back, shoulder blades, teeth, stomach, arms.
These are the symptoms of angina pectoris. What it is is now clear.
The main forms of unstable angina pectoris
Unstable angina is a variant of the development of coronary heart disease, which in practice manifests itself as intense, pressing pain in the pericardial region, which can independently regress or transform into more complex forms of coronary artery disease - myocardial infarction, sudden death of coronary origin.
According to the modern classification, it is customary to distinguish the following types of unstable angina:
- First appeared
This form of the disease is characterized by the duration of the onset of the first cardialgic manifestation, which is no more than one to two months. The disease is often complicated by such an acute form of coronary artery disease as myocardial infarction. In a number of clinical cases, unstable angina, which occurs for the first time, can transform into a stable form of the disease.
- Progressive view
This type of disease is characterized by a particular intensity of pain, an increase in the frequency of attacks and their duration, as well as the appearance of characteristic changes in the electrocardiogram that have not previously been recorded.
- Early post-infarction angina pain
It is characterized by the appearance of pain symptoms from 1 to 28 days after myocardial infarction.
- Prinzmetal's angina
This type of disease is known as vasospastic. The pathology is extremely rare and is manifested by the development of angina attacks in a state of absolute rest (usually during sleep) without any contributing factors. It is believed that the cause of this condition is an unexpected spasm (narrowing) of the coronary vessels, the etiology of which scientists have not yet been able to fully investigate.
Differences in unstable angina
Unstable angina can be distinguished by the following signs:
- Symptoms progress during an attack, the attack is more difficult to bear, pain affects adjacent areas (jaw, back, neck, left arm).
- An anginal attack has acute manifestations (feeling of heaviness in the chest, heat, squeezing) and, along with suffocation, occurs more and more often.
- For an attack to occur, less and less load is required each time; angina pectoris can occur even at rest.
- Signs of acute ischemic disorders were detected after coronary artery bypass surgery, no later than 90 days before contacting a specialist.
- The pain is poorly relieved by the use of Nitroglycerin.
- The paroxysm lasts more than a quarter of an hour.
- Prinzmetal's angina occurs, as a rule, in males, and it develops regardless of their physical activity. Between attacks, the patient is able to withstand severe muscle tension without consequences. More often, heart pain appears in the morning. They are provoked by spasms in the coronary arteries, in which atherosclerotic changes are not always observed. The pathological condition is characterized by rapid progression and carries a high risk of myocardial infarction.
How to get rid of heart pain due to angina pectoris?
Prognosis: is there a chance of recovery?
The answer to this question sounds disappointing: absolute recovery will not be achieved. But don't rush to panic. In the 21st century, almost all diseases have a chronic course: hypertension, diabetes, obstructive pulmonary disease, and so on. The causes of these pathologies are not bacteria, which doctors have successfully learned to fight, but lifestyle and environmental conditions.
The basis of coronary heart disease is atherosclerosis, which begins to develop with the birth of a person. Unstable angina is an acute manifestation of this process. By removing the symptoms by stenting, we do not destroy the root cause. To prevent new exacerbations, constant use of medications is necessary to prevent pathologies from progressing.
All patients want to minimize the use of pharmaceutical drugs, and some of them stop treatment after relief occurs. In their understanding, discharge from the hospital means freedom from medications, because there is no more pain. Unfortunately, such a decision often turns against them with serious consequences - a hospital bed and life-threatening complications.
In conclusion, I would like to add that cardiovascular diseases cannot always be defeated, but it is quite possible to prevent them. Weight control, smoking cessation, regular physical activity, normal cholesterol and glucose levels will help you in the fight for your health.
An important part of my work is preventive education of patients. Everyone does their own thing, and mine is to help people get rid of heart problems. Since this can only be done in the early stages of development of the pathology or at the stage of formation of a predisposition to it, I pay a lot of attention to issues of nutrition, lifestyle and screening. Only in this way - together - can we significantly improve the health of the nation.
Diagnostics
The diagnosis is established based on the patient’s complaints about the progression of angina attacks, medical history, and the results of various laboratory and instrumental studies:
- Analyzes of samples of biological fluids.
- Coronary angiography.
- Echocardiography.
- Centigraphy.
- Daily monitoring using the Holter method.
Due to the fact that the symptoms may be atypical, differential diagnosis should be carried out and myocarditis, mitral valve disease, pneumonia, esophagitis, pleurisy, osteochondrosis, pancreatitis, and gastrointestinal disorders should be excluded.
How is diagnosis done?
To diagnose the disease, the patient is initially interviewed and all existing complaints about his health condition are clarified. Establish the relationship between attacks and the presence of other symptoms and causes.
Daily ECG monitoring allows you to register episodes of transient ischemia, both associated with pain and painless, and determine their number
Next, an electrocardiogram is prescribed, which is supplemented with daily ECG monitoring. Laboratory tests are also used for diagnosis - a general blood test, which shows the number of leukocytes.
Ultrasound examination determines where the areas with reduced myocardial contractility and cardiac output indicators are located.
To determine the level of narrowing of the heart arteries, an angiogram is used when a contrast agent is injected into the vessels.
Treatment
Treatment of unstable angina should be carried out exclusively in a hospital setting. When an attack occurs, the patient should call emergency assistance, while waiting for it to take Nitroglycerin and Aspirin. After admission to the hospital, the patient is provided with assistance according to the following algorithm:
- Elimination of pain syndrome.
- Removing obstacles to normal blood circulation.
- Providing measures to prevent sudden cardiac arrest and the onset of the acute phase of myocardium.
- Rehabilitation therapy to stabilize the condition.
Diagnostic detection methods
The presented data convinces of the need for a detailed interview with the patient, clarifying the connection between a painful attack and other symptoms, time frames, and causes.
The main diagnostic method - ECG studies - is available in clinics and ambulances. Typical diagnostic manifestations are familiar to doctors of all specialties. It is necessary to take into account the course of the disease, symptoms and the possibility of delayed ECG manifestations or even their absence.
Holter monitoring during the day is especially indicated in stationary conditions.
ECG can be taken even at home
Laboratory methods reveal:
- leukocytosis in a general blood test;
- high levels of low-density lipoproteins, enzymes AST (aspartic aminotransferase) and LDH (lactate dehydrogenase), CPK (creatine phosphokinase) in biochemical analysis.
An ultrasound can show areas of decreased myocardial contractility and establish a decrease in cardiac output.
To check the patency of the coronary vessels, an angiogram is performed with the introduction of a contrast agent.
Medicines
After stopping the attack, the patient is prescribed a special diet, bed rest, complete emotional rest, and taking special medications, including:
- Nitrates (“Isosorbide dinitrate”, “Nitroglycerin”). Able to dilate coronary arteries and reduce myocardial oxygen demand.
- Antiplatelet agents, anticoagulants (“Fraxiparin”, “Aspirin”). To prevent the formation of blood clots and increase blood flow.
- Metabolic drugs.
- Calcium channel inhibitors (Verapamil, Cinnarizine), which improve patency in the coronary arteries.
- Painkillers (narcotic origin, antipsychotics), for example, Fentanyl, Droperidol. Indicated for the relief of acute pain.
- Statins (Lovastatin, Rosuvastatin), which help lower cholesterol levels and prevent the formation and hardening of cholesterol plaques.
- Beta blockers (“Proprnalol”, “Carvedilol”), which reduce the heart rate and improve blood flow.
Causes of angina
With few exceptions, the disease develops as a result of atherosclerosis of the heart vessels. Cholesterol, accumulating in the wall of blood vessels and forming an atherosclerotic plaque, narrows their lumen, causing local disruption of myocardial blood flow. When the load on the heart muscle increases during physical or emotional stress, the relationship between the delivery of oxygen to the heart and its need occurs. Under conditions of oxygen starvation, metabolic acidosis develops in the working tissue and irritation of myocardial pain receptors. Subjectively, these changes are expressed by pain in the heart area.
But this doesn't always happen. In 1957, during a dynamic ECG study of a group of patients, short-term episodes of myocardial ischemia without subjective manifestations were first identified. Instrumentally detected signs of disturbances in the metabolism of the heart muscle, its contractility, and electrical activity did not entail the development of angina attacks. This form of ischemia was called painless. It is prognostically unfavorable in terms of a high risk of sudden death or myocardial infarction without a history of previous pain. The mechanism of development of silent ischemia is not fully understood. Based on a number of studies, as an option, it was suggested that for the development of pain, the ischemic factor must be of a certain strength and duration of exposure, exceeding a certain threshold value. It has been instrumentally confirmed that ischemia for less than three minutes does not cause pain. On the ECG, silent ischemia is manifested by a less profound and prolonged displacement of the ST segment.
Diagnosis of angina pectoris
- Characteristic pain syndrome;
- Transient depression of the ST segment > 1 mm, including in combination with changes in the T wave, at rest or during exercise, positive stress tests. Changes in the ECG are detected during a standard ECG at the time of an attack, or during daily Holter ECG monitoring. An attack of variant angina is characterized by ST segment elevation.
- Coronary angiography reveals areas of stenosis (narrowing) in the vessels of the heart affected by atherosclerosis, which makes it possible to clarify the diagnosis.
- Laboratory indicators are uninformative.