Diagnosis of IHD
Late diagnosis of coronary heart disease is one of the common causes that claim the lives of 700 thousand Russians every year. Only a correct diagnosis, observation by a qualified cardiologist, and regular examinations guarantee that your heart will not let you down. With IHD, mortality (especially in men 55-65 years old) is 70%. And the main reasons are delayed access to a doctor, inappropriate treatment. Don’t risk your life - undergo professional and objective diagnostics at the CBCP Center for Circulatory Pathology!
Coronary heart disease (CHD)
Stroke
Diabetes
5073 08 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Coronary heart disease (CHD): causes, symptoms, diagnosis and treatment methods.
Definition _
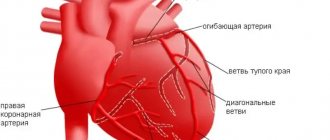
Coronary heart disease (CHD) is an acute (transient) or chronic (stable) damage to the heart muscle (myocardium) caused by a decrease or cessation of blood flow through the coronary arteries.
Causes of coronary heart disease
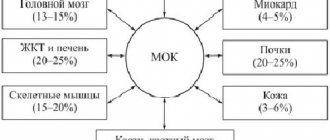
Myocardial ischemia occurs when the myocardial demand for oxygen exceeds the ability to deliver it through the bloodstream through the coronary arteries. Normally, the coronary arteries have a reserve for expansion, providing a fivefold increase in coronary blood flow, and, as a result, oxygen delivery to the heart muscle. A discrepancy between oxygen delivery and muscle demand can occur under the influence of various factors.
In 95% of cases, the cause of coronary heart disease is a decrease in its blood supply (insufficient oxygen supply) through the coronary arteries due to atherosclerotic narrowing of the lumen of the vessel.
The course of the disease is determined by the presence and further growth of an atherosclerotic plaque, which can block the vessel completely or partially. When blood pressure increases, the sclerotic endothelium of the vessel is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
A significant role in the development of IHD is played by disturbances in the movement of blood through the vessels and changes in the rheological properties of blood (the ability of blood to flow).
The formation of a blood clot, especially against the background of vessel spasm, can lead to complete or partial blockage.
In 5% of cases, the cause of IHD is congenital anomalies of the origin of the coronary arteries, Marfan and Ehlers-Danlos syndromes with aortic root dissection, coronary vasculitis in systemic connective tissue diseases, Kawasaki disease and Hurler syndrome, infective endocarditis, overdose of vasoconstrictor drugs and certain narcotic drugs, syphilitic mesaortitis and other conditions.
There are factors that provoke the development of coronary heart disease that can be influenced: dyslipoproteinemia (violation of the normal ratio of blood lipids); arterial hypertension; diabetes; smoking; low physical activity; obesity; stress. And also those risk factors for the development of coronary artery disease that cannot be changed: male gender, age, family history of cardiovascular diseases (myocardial infarction or ischemic stroke in close relatives: in women - up to 65 years, in men - up to 55 years).
Classification of IHD
I. Acute myocardial infarction (MI).
- According to the stage of the disease:
- developing – from 0 to 6 hours;
- acute – from 6 hours to 7 days;
- healing (scarring) – from 7 to 28 days;
- healed - starting from the 29th day.
- According to the depth of the lesion:
- transmural MI (necrosis of the entire thickness of the heart muscle);
- Q-wave (Q wave appears on the ECG);
- not Q-generating.
- By localization:
- front;
- lower;
- myocardial infarction of other specified locations;
- myocardial infarction of unspecified localization.
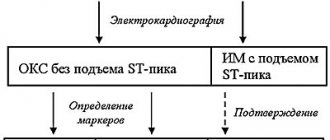
- Based on the presence or absence of persistent ST segment elevation on the ECG:
- myocardial infarction with ST segment elevation on ECG;
- myocardial infarction without ST segment elevation on ECG.
II. Unstable angina (a period of ischemic heart disease that threatens the development of myocardial infarction).
- New-onset angina.
- Progressive angina.
- Variant angina (Prinzmetal's angina).
III. Chronic ischemic heart disease.
- Angina pectoris I-IV FC (functional class).
- Previous myocardial infarction.
Symptoms of coronary heart disease
Coronary heart disease can have a relatively benign course over many years. The progression of atherosclerosis of the coronary vessels leads to the development of the disease.
The most common form of coronary artery disease is angina pectoris, in which the most common complaint of patients is squeezing or pressing pain in the chest. The pain can radiate to the left arm, back or neck, lower jaw, less often to the area under the xiphoid process, and last from 2 to 5 or even 20 minutes. It occurs during physical exertion or severe psycho-emotional stress. After stopping physical activity or 1-3 minutes after taking nitroglycerin, the pain quickly disappears.
As the disease progresses, there comes a time when even minimal exertion is enough for an angina attack, and finally, attacks begin to occur at rest. Some patients may experience pain while lying down due to increased blood flow to the heart.
It is necessary to take into account that pain that occurs with other diseases (neuralgia, gastralgia, cholecystitis, etc.) can provoke and intensify existing angina.
When the blood circulation of the heart muscle is disrupted with the development of a focus of necrosis (tissue death), myocardial infarction occurs. A heart attack (from the Latin infarcire - to stuff, stuff) is the necrosis of organ tissue due to an acute lack of blood supply.
The pain of myocardial infarction is significantly greater in intensity and duration than a normal angina attack.
The pain is not relieved by nitroglycerin and its duration can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by weakness, dizziness, headache, vomiting, fainting, and loss of consciousness. The patient looks pale, his lips are blue, and he is sweating.
Diagnosis of coronary heart disease
The diagnosis of “coronary heart disease” is established by a combination of complaints, information about the course of the disease, data from laboratory and instrumental examination methods.
For all patients with suspected ischemic heart disease, the following questions are asked:
- current or past smoking;
- the presence of cardiovascular diseases and/or deaths from cardiovascular diseases in the patient’s immediate relatives (father, mother, siblings);
- previous cases of seeking medical help and the presence of previously registered electrocardiograms, studies and conclusions;
- comorbidities to assess additional risks;
- medications taken.
The following studies are recommended for all patients with coronary artery disease or suspected coronary artery disease at initial consultation:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);
What does the primary diagnosis consist of?
At your first meeting with you, the CBCP cardiologist will:
- will listen to your complaints;
- will ask what medications you are taking;
- will study data from previous studies (if available);
- will conduct an examination to identify cyanosis or swelling;
- listen to noises.
For the most accurate diagnosis of coronary heart disease, your detailed and comprehensive answers are very important, so it is worth preparing for this meeting. Remember the unpleasant sensations in the left side of the chest, their changes over time. Indicate whether you have increased heart rate, irregular heartbeat, shortness of breath, nausea, excessive sweating, dizziness, or loss of consciousness.
Laboratory diagnostic tests
Coronary heart disease is characterized by many symptoms. Patients feel many of them quite subjectively. Therefore, instrumental and laboratory examinations are important to make an objective diagnosis.
- The CBCP laboratory will determine the level of sugar, cholesterol in the blood, specific enzymes characteristic of IHD (troponins, myoglobin, etc.)
- Among instrumental studies, various types of electrocardiography, as well as ultrasound studies (echocardiography, stress echocardiography), have the greatest accuracy.
Risk factors for the development of myocardial ischemia
Factors predisposing to this disease are conventionally divided into two groups – modifiable and non-modifiable.
By eliminating or correcting the former, the risk of coronary heart disease is significantly reduced. This group includes situations in which the myocardium needs more oxygen than usual (or oxygen delivery is reduced without increasing its consumption):
- sedentary lifestyle;
- excess weight;
- unhealthy diet – a large amount of fatty and high-calorie foods in the diet;
- psycho-emotional stress;
- bad habits, especially smoking;
- high levels of “bad” cholesterol and triglycerides in the blood;
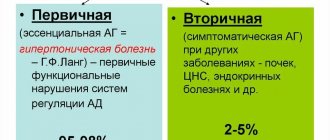
- high blood pressure – arterial hypertension;
- diabetes;
- endocarditis and heart defects;
- decrease in the concentration of high-density lipoproteins in the blood.
Factors that cannot be changed:
- male gender;
- age over 65 years;
- IHD, especially myocardial infarction in the past in close relatives of the patient;
- the onset of menopause.
The likelihood of coronary heart disease in women increases significantly with the onset of menopause.
Electrocardiography (ECG) at CBCP
Chronic coronary heart disease is traditionally diagnosed using an ECG . Almost every person undergoes this simple and painless procedure several times during their life. You will sit on a comfortable couch, the doctor will attach electrodes to your body and within 10-15 minutes the electrocardiograph will read the performance of the heart muscle. In our clinic you will undergo an ECG using a General Electric MAC 800 electrocardiograph (USA), which determines hidden changes in myocardial metabolism. The transcript is issued immediately.
An expanded option for diagnosing coronary heart disease is Holter ECG monitoring. It is the same ECG, but carried out over 24, 48 or 72 hours. A portable heart rate monitor (fits comfortably under your shoulder or on your belt) with secure electrodes attached to your body, continuously reads and records your readings. The method identifies irregular heart rhythm disturbances, examines the functioning of the heart muscle during sleep, during emotional and physical stress. The procedure allows the doctor to understand the causes of ischemic heart disease.
Echocardiography (ultrasound of the heart)
Echo-CG, also called cardiac ultrasound, can significantly clarify the diagnosis. Coronary heart disease is accompanied by changes in its size, condition of valves, cavities, pericardium, and large vessels. In addition to visualizing cardiac structures, this safe ultrasound procedure evaluates myocardial contractility and the presence of acoustic noise.
At the CBCP clinic you will undergo a cardiac ultrasound using a modern expert-class ultrasound system MyLab 50 (Italy). You will need to undress to the waist and lie on your left side. The doctor will lubricate the chest with a special gel and will move an ultrasonic sensor over the skin, which will read the information. You receive a conclusion 10 minutes after the end of the procedure.
Stress echocardiography
Stress echocardiography is another ultrasound method that allows you to effectively diagnose the disease. In this case, coronary heart disease is studied under physical or medicinal stress. Disturbances in heart contractions and blood flow are detected that are not noticeable at rest, which is why IHD is asymptomatic.
Under the supervision of a diagnostician who has undergone special training in stress echocardiography, you will perform exercises on an exercise bike. If exercise is contraindicated, you will be given a safe stimulant drug. At this time, the equipment records various indicators. The doctor will decipher it within 15 minutes and give you a conclusion.
Treatment of coronary artery disease
Treatment for coronary heart disease includes lifestyle changes, medications and, in some cases, surgery.
All patients are advised to give up bad habits, spend more time in the fresh air, and reduce excess body weight. In your diet, you must avoid foods high in fat, very salty and sweet foods. Smoking and unauthorized discontinuation of prescribed medications are strictly prohibited. All this can lead to a sharp deterioration in the patient's condition. To stop an attack of angina, you need to immediately stop physical activity, provide access to fresh air and take nitroglycerin under the tongue or use nitrate in the form of a spray.
Basic drug therapy includes the following drugs:
- antiplatelet agents – drugs that thin the blood;
- beta blockers;
- ACE inhibitors or sartans;
- statins.
Long-acting nitrates can be used to prevent attacks.
In the presence of concomitant diseases, especially diabetes mellitus and hypertension, their treatment and achievement of target blood pressure and glucose levels are required.
To restore cardiac blood flow, surgical intervention is necessary in some cases:
- Coronary artery bypass surgery is the creation of a bypass for blood at the site of narrowing of the coronary arteries using vascular prostheses.
- Coronary angioplasty and stenting - restoration of the diameter of the vessel, and, accordingly, the blood flow in it, by installing a special dilator.