Most cases of angina are associated with a sharp increase in the level of physical or psycho-emotional stress. However, there are exceptions to this rule. Thus, Prinzmetal's angina, also called variant, vasospastic or spontaneous, usually develops in a patient who is at rest. The typical time for symptoms to occur is between midnight and the wee hours of the morning. The pain syndrome is intense, spreading to the head or arms, reminiscent of signs of seizures. It is more often observed in smokers, patients with high cholesterol or blood pressure, but can also occur in healthy people. Thanks to modern diagnostic methods and a thoughtful course of treatment while eliminating bad habits or factors, it is possible to significantly reduce the frequency of attacks and make them less painful.
Causes of Prinzmetal's angina
Coronary artery spasm can occur in the following cases:
- hypothermia of the body;
- smoking;
- symptoms of arterial hypertension;
- stress;
- increased cholesterol levels;
- taking medications that slow blood flow;
- consumption of alcohol and drugs.
The disease is more common in patients aged 50 to 60 years. 5 times more common in men than in women. Smoking and alcohol consumption are recognized as the main risk factors. Less commonly, the pathology develops against the background of vasomotor vascular disorders.
Prinzmetal's angina (AP), also called vasospastic or variant [1], is characterized by the occurrence of anginal pain of typical localization at rest, but not during physical activity, during which discomfort in the chest is absent or even disappears. The development of attacks of vasospastic angina is associated primarily with episodes of local spasm of the coronary arteries (CA) in the absence of hemodynamically significant atherosclerotic lesions. At the same time, it is possible that spasm may predominate, which can lead to the development of acute coronary syndrome and acute myocardial infarction in patients with coronary artery atherosclerosis.
According to the recommendations of the Expert Committee of the All-Russian Scientific Society of Cardiology [1], vasospastic angina is diagnosed based on the identification of the following criteria:
- the occurrence of anginal attacks at rest with a transient increase (but not decrease) in the ST segment;
- good tolerance to physical activity, which nevertheless sometimes provokes an attack of angina (the so-called variable threshold for the occurrence of angina), usually in the morning, but not in the afternoon or evening;
- the effectiveness of calcium antagonists and nitrates in preventing angina attacks; β-blockers, on the contrary, are ineffective and can provoke anginal pain.
SP was first described in 1959 by American cardiologist Miron Prinzmetal M. et al. [2]. M. Prinzmetal was born in Buffalo (New York, USA) on February 8, 1908 and was the second child in the family (his older brother later became a famous lawyer). M. Prinzmetal received his doctorate in medicine in 1933 from the University of San Francisco (California). While still a student, he took part in scientific research and became one of the co-authors of a scientific publication that discussed the effect of drugs that induce bronchospasm on intrapleural pressure.
During his residency, Prinzmetal became a National Research Council Fellow at Harvard. By that time, he had already published more than 20 printed works on the problems of pulmonology (including pulmonary emphysema), ventricular tachycardia - he was one of the active enthusiasts of the active introduction of the electrocardiography method into routine clinical practice.
Since 1935, M. Prinzmetal worked at the famous Mount Sinai Hospital (New York), where he carried out a series of scientific studies. Among them are work devoted to the role of peripheral vasospasm in the formation of arterial hypertension (AH) [3], a description of pheochromocytoma with confirmed hyperproduction of adrenaline at the time of hypertensive crisis [4], studies on the role of renin in the formation of urine [5] and the pathogenesis of hypertension in total ischemia kidneys [6]: using an original experimental model, he confirmed the fundamental results previously obtained by H. Goldblatt (1934), which made it possible to significantly approach the understanding of the mechanisms of development of hypertension in stenotic lesions of the renal arteries. Prinzmetal studied the role of renin in the development of hypertension in collaboration with GW Pickering. Having received the title of honorary member of the American College of Physicians, M. Prinzmetal worked for a year at University College London and later returned to the USA.
During World War II, M. Prinzmetal partially reoriented the direction of his scientific work in accordance with wartime demands, studying the pathogenesis, clinical picture and outcomes of emergency conditions, including shock, occurring in persons with severe muscle trauma and burns. In the field of cardiology, Prinzmetal began to develop various aspects of the regulation of coronary blood flow, in particular during its partial occlusion and the formation of collaterals. In addition, Prinzmetal actively studied the mechanisms of heart rhythm disturbances emanating from the left atrial appendage. He improved the electrocardiographic method and characterized the mechanisms underlying changes in the R wave and ST segment in acute myocardial infarction. During the same period, M. Prinzmetal became one of the pioneers of the clinical use of radioactive iodine for the treatment of diffuse toxic goiter (Graves' disease).
While developing experimental methods for characterizing blood flow in the coronary artery, Prinzmetal et al. was one of the first to document spasm of large coronary arteries [7]. His description of the vasospastic form of angina, later named after him, became the basis for identifying a special clinical form of coronary heart disease that is still recognized today. M. Prinzmetal’s great contribution to the study of the problem of acute myocardial infarction and cardiac arrhythmias; in particular, he took part in studying the antiarrhythmic effects of quinidine and propranolol.
M. Prinzmetal has published more than 160 scientific articles. He served on the editorial boards of the American Heart Journal and the American Journal of Cardiology, and was at the forefront of the creation of one of the most influential public professional organizations for cardiologists today, the American College of Cardiology. M. Prinzmetal is deservedly considered as one of the main organizers of cardiological services in the western United States.
Having devoted himself entirely to medicine, Prinzmetal nevertheless collected a unique collection of rare books, which included ancient editions of Shakespeare’s works, as well as the famous work of W. Harvey “Anatomical study of the movement of the heart and blood in animals” (“Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus”) is the only copy that was in private possession. He donated the only known portrait of W. Harvey to the Royal College of Physicians of London. The ideal for M. Prinzmetal was always the famous Anglo-American therapist W. Osler, whose name and works he tirelessly popularized. In addition, M. Prinzmetal was a connoisseur of classical music. M. Prinzmetal died in 1987.
To diagnose SP, the use of provocative tests is recommended, however, traditionally used cold and hyperventilation tests are characterized by extremely low sensitivity and specificity. Tests with acetylcholine and ergonovine are more informative, but before performing them it is advisable to perform coronary angiography in order to demonstrate the absence of stenotic lesions of the coronary arteries. In addition, at the time of an attack of chest pain, it is advisable to perform an ECG, and in an outpatient setting, Holter ECG monitoring [1].
SP remains a largely mysterious disease today. On the one hand, its development is associated with excessive activation of the sympathetic nervous system - in patients suffering from it, the so-called. coronary (type A) personality type and increased anxiety [8]; they are characterized by depression and panic attacks [9]. Nevertheless, it is obvious that in the development of vasospastic angina, dysfunction of the endothelial cells of the coronary arteries, possibly local, is no less important - in some patients, spasm of the same section of the coronary bed recurs [10]. The role of certain genetic determinants is discussed, in particular the polymorphism of the gene encoding endothelial NO synthase, which causes a decrease in its activity and, accordingly, a decrease in the formation of NO - the main agent that prevents spasm and causes dilatation of the coronary artery. It has been demonstrated that SP is associated with carriage of the Glu298Asp variant in exon 7 [11] and the T-786 C variant in exon 5 [12] of the endothelial NO synthase gene. It has been demonstrated [13] that in carriers of the T-786 C variant of the NO synthase gene, the frequency and severity of vasospastic angina attacks can be significantly reduced by oral administration of L-arginine, a complete precursor of nitric oxide.
Other mechanisms that determine the tendency to develop attacks of SP include an increase in the activity of phospholipase C with a subsequent increase in phosphorylation of myosin light chains, leading to excessive contractility of vascular smooth muscle cells [14]. Along with this, the hypersensitivity of vascular smooth muscle cells to calcium ions and the accumulation of this ion in their cytoplasm are called as a circumstance predisposing to the development of SP [8].
Typical SP, unlike other clinical variants of angina, often does not have a clear association with most traditional cardiovascular risk factors, including hypertension, diabetes mellitus and a decrease in serum concentrations of high-density lipoproteins. These risk factors are less common in vasospastic angina than in typical exertional angina. In addition, the age of patients with variant angina is often significantly younger than the age of patients suffering from stable angina [10]. At the same time, SP develops significantly more often in smokers [15]: it is well known that smoking contributes to a significant increase in endothelial dysfunction and the formation of a tendency to vasospasm.
Factors that provoke an attack of SP include:
- peace;
- psycho-emotional stress;
- smoking;
- hyperventilation;
- smoking;
- cooling;
- catecholamines (adrenaline, norepinephrine);
- β-adrenergic agonists (dobutamine);
- anticholinesterase agents (physostigmine, neostigmine);
- ergot alkaloids (ergonovine, ergotamine);
- serotonin;
- prostaglandin;
- cocaine;
- histamine;
- calcium chloride
The prognosis for SP is quite serious: these patients often develop acute coronary syndrome/acute myocardial infarction, as well as ventricular arrhythmias, and sudden death is possible [16, 17]. Beta-blockers are ineffective for vasospastic angina; mainly antianginal drugs with a direct coronary effect (nitrates, calcium antagonists) are used for its treatment [1]. However, in more than 2/3 of patients with SP, chest pain recurs [18, 19]. With the development of severe ventricular cardiac arrhythmias, these patients undergo implantation of a cardioverter-defibrillator [8]. Experience with the use of other drugs, including those that selectively eliminate endothelium-dependent mechanisms of vasodilation, for example endothelin-1 antagonists, is so far limited to the description of individual clinical observations [20]. Studying the significance of genetic determinants and features of the pathogenesis of SP will not only improve the management tactics of these patients, but will also bring us even closer to understanding the mechanisms of development of coronary spasm and associated life-threatening complications.
Symptoms of Prinzmetal's angina
The list of characteristic symptoms of vasomotor angina includes:
- pain in the chest at rest, which can be of a different nature - from some discomfort to severe pain radiating to the head or arm;
- feeling of pressure and tightness in the chest;
- attack of nausea;
- sweating;
- dizziness, clouding of consciousness;
- tachycardia, etc.
The duration of the attack ranges from 2 to 20 minutes, and the characteristics of individual episodes are usually similar to each other. Cases of relapse with frequent attacks may be followed by a state of calm for several weeks or months.
Are you experiencing symptoms of Prinzmetal's angina?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Where can I get diagnosed and treated?
Rest assured that your heart is not in danger! If the first symptoms and signs of angina appear, consult a qualified healthcare provider. Cardiologists at the CBCP Center for Circulatory Pathology are ready to help you. The clinic will offer professional consultation and modern types of diagnostics, through which the doctor will receive objective, detailed and accurate information about the disease.
If you discover serious violations, do not despair! The level of medicine at CBCP makes it possible to effectively treat complex cardiovascular diseases using medicinal and non-surgical methods.
Methods for diagnosing the disease
Suspicion of Prinzmetal's angina arises in any case if the patient complains of sharp chest pain at rest or at night. The diagnosis implies that the duration of attacks can range from 30 seconds to 5 minutes, and their number varies up to several dozen within half an hour. In addition, an indirect sign is the subsidence of pain when taking sublingual drugs with a nitrate chemical composition.
The initial assumptions can be confirmed by:
- electrocardiogram in the format of a one-time study or daily monitoring;
- provocative pharmacological tests.
What can the disease be confused with?
As for diseases not related to the cardiovascular system, based on the symptoms and signs, angina pectoris can be mistaken for:
- osteochondrosis of the cervical or thoracic spine;
- vegetative-vascular dystonia;
- gastrointestinal diseases (diaphragmatic hiatal hernia);
- pleurisy, pulmonary embolism;
- pinched nerves.
Usually this disease is confused with the onset of myocardial infarction. The signs are really very similar. The main difference is that an attack of angina is relieved by taking nitroglycerin. In case of a heart attack, the medicine does not work or relieves pain only slightly and temporarily.
Treatment of Prinzmetal's angina
A course of medication that affects both the symptoms of the disease and its causes can help cope with attacks and reduce their regularity. Clinical recommendations for Prinzmetal angina include:
- taking drugs from the category of calcium antagonists in combination with long-term nitrates;
- anti-alpha adrenergic drugs that prevent coronary artery spasm;
- a course of antioxidant vitamins C and E;
- other medications that promote the natural elasticity of blood vessels and maintain their conductive capacity.
If a conservative course turns out to be ineffective, doctors resort to surgical intervention. More often this is coronary angioplasty with stenting, less often cardiac denervation with plexectomy simultaneously with coronary bypass surgery. A decision may be made to implant an automatic defibrillator or pacemaker.
Risk factors for developing angina
The following factors lead to narrowing of the coronary vessels and insufficient blood supply to the myocardium:
- atherosclerosis - deposition of cholesterol plaques in the walls of blood vessels;
- hypotension ー low blood pressure;
- coronary artery thrombosis;
- age-related changes in blood vessels.
In the vast majority of cases, angina is caused by atherosclerotic lesions of the coronary arteries. It develops due to disturbances in the metabolism of cholesterol and other lipids: excess animal fats in the diet, lack of plant foods. Therefore, proper nutrition is the basis for successful prevention of angina pectoris.
Nicotine also constricts blood vessels, so smokers develop angina more often.
The risk group for the development of angina pectoris includes:
- people over 55 years of age;
- men;
- smokers;
- people who abuse alcohol and drugs;
- people with pathologies of the cardiovascular system (heart defects, heart failure);
- with pathologies of the respiratory system (bronchial asthma, chronic obstructive diseases);
- overweight.
All these factors increase the risk of developing atherosclerosis, cardiac ischemia and angina. Most of them can be eliminated through lifestyle changes.
FAQ
What does Prinzmetal's angina mean?
This is the name of a separate type of angina, the main symptom of which is severe pain during the patient’s rest or night sleep. The main reason is a short-term spasm of the coronary artery, as a result of which the blood flow sharply slows down. But the heart muscle, maintaining the same rhythm of work, is forced to contract even more intensely, which gives a characteristic pain syndrome.
How does Prinzmetal's angina manifest?
It is not easy to miss an attack of the disease: it makes itself felt by a sharp pain in the heart area, which radiates to the head, shoulder or arm. You feel nausea, difficulty breathing due to a feeling of pressure in the chest, dizziness, and a sharp increase in heart rate. Sometimes patients complain of nausea and sweating.
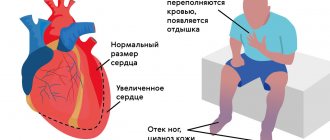
How does the disease develop?
It is at such moments that common signs of angina pectoris appear in women and men: you feel a lack of air, arrhythmia. At this time, chemical changes occur in the myocardium associated with metabolic disorders, a decrease in the synthesis of substances, and the accumulation of acids. The functions of the myocardium are gradually disrupted, and its metabolism changes.
What causes this disease? There are certain factors:
- high cholesterol levels;
- obesity when consuming excessive amounts of fats and carbohydrates;
- physical inactivity disrupts lipid volume;
- smoking causes oxygen starvation of cells and arterial spasm;
- arterial hypertension causes myocardial tension;
- anemia, intoxication contribute to oxygen starvation;
- diabetes mellitus increases the risk of ischemia;
- increased blood viscosity is a direct risk of blood clots;
- psycho-emotional stress (especially in women) worsens myocardial nutrition.
Description
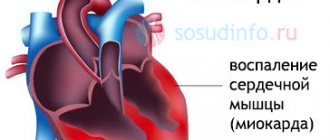
Prinzmetal's angina is a disease characterized by cyclical attacks of chest pain resulting from spasm of the arteries supplying blood to the heart muscle.
In medical practice, you can find other names, such as variant, spontaneous, vasospastic angina. It was first described by the American cardiologist M. Prinzmetal in 1959. In total, about 3% of patients with coronary heart disease suffer from the pathology. According to my personal observations, the disease is more often found in heavy smokers who have diseases such as:
- arterial hypertension;
- peptic ulcer;
- chronic hepatitis of viral and toxic etiology.
So what should we do?
Once Prinzmetal's angina has been diagnosed, treatment becomes challenging. Medication measures show the greatest effectiveness. In this case, they resort to several groups of drugs.
First of all, the patient should have short-acting, quick-acting medications on hand. As a rule, this is a nitroglycerin spray or tablets. It is necessary to take the medication as soon as the attack begins so that the symptoms subside. As a preventive measure, it is permissible to use drugs based on nitroglycerin, but acting for a long period of time. These include:
- "Kardiket";
- "Nitrosorbide".
Characteristics
Prinzmetal's angina is clearly visible on the ECG. This study shows characteristic changes. They usually appear during an attack, and when it ends, the indicators gradually return to normal. From the diagram you can see that during an attack the RS-T segment rises above the isoelectric line. The T turns into a tall prong. These are key features that help distinguish variant angina from other subtypes of angina.
Changes in QRS are diagnosed: Q becomes a pathological wave, R becomes larger than normal, QRS widens.
Failures in the functioning of the ventricle lead to disturbances in the rhythm of the heartbeat. In particularly difficult cases, ventricular fibrillation is diagnosed. In addition, atrioventricular conduction is affected. When the pain syndrome passes, Prinzmetal's angina is characterized by a fairly rapid restoration of all indicators to standard values.
To diagnose the disease, it is customary to resort to a bicycle ergometer test and coronary angiography.
Clinical case
In 2021, a 42-year-old man came to me with complaints of recurring attacks of anginal pain, mainly at 4:00 - 5:00 in the morning and much less often during the daytime.
Connects their appearance with stressful situations that arise at work and at home. Smoking has been a bad habit for the last 30 years. History of peptic ulcer of the gastric antrum and duodenal bulb. General examination and auscultatory picture are without any features. There was a slight increase in blood pressure to 135/85 mm Hg. Blood test showed Hb 169 g/l, erythrocytes 5.7 cells/l. Clinical examination of urine is unchanged. During a 3-day Holter monitoring of the electrocardiogram during the next night attack, ST segment elevation of up to 6 mm in the precordial leads was noted, followed by restoration to the isoline upon its completion. The diagnosis was made: IHD. Prinzmetal's angina pectoris NCo CHO (NYHA) . Treatment with a calcium channel antagonist, Verapamil, was prescribed; during the attack, the use of nitrates in the form of a spray (Nitromint) was allowed. A complete cessation of smoking was also recommended.
The patient returned again 2 months later and noted a noticeable improvement in his general condition and the complete disappearance of night and daytime attacks.
Do you have friends or relatives who are bothered by night attacks of chest pain? Share your experience in the comments, and our expert will express his opinion.
Diagnostic features
Despite the fact that modern science has already well studied Prinzmetal's angina, the symptoms and treatment of this pathology, diagnosing the disease is still a serious problem. It was not possible to develop an instrumental method showing sufficient reliability.
Coronary angiography is considered the most correct and informative method. In this case, the heart vessels are examined by injecting a contrast agent into the patient’s body, after which X-ray irradiation is performed.
If a contrast agent is injected into the body or a catheter is placed in the vessel, this can provoke a spasm. It is this fact that is studied during medical experiments on a patient, since such a spasm of the vessel makes it possible to speak with a high degree of reliability about Prinzmetal’s angina. The drug ergonovine is usually used, which enhances the ability of smooth muscles to contract. To remove the narrowing, nitroglycerin is injected into the vein.
Complications: are there any?
Medical statistics show that the likelihood of complications directly depends on how severe and frequent the attacks are, and how long they last. In particular, the situation is relatively mild if the coronary arteries are not affected. On average, about 0.5% of patients with Prinzmetal's angina die per year with this development of pathology.
In some patients, attacks are severe, last a long time and occur frequently. Here the risk of death is significantly higher; up to a quarter of all patients with angina die per year.