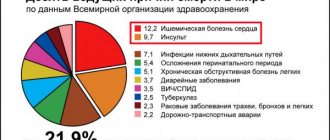
Cerebellar stroke is still one of the least studied diseases of the central nervous system. The variability of clinical manifestations, their similarity to symptoms of damage to the cerebral hemispheres and other features significantly complicate diagnosis. This pathology occurs relatively rarely: approximately 2% of patients with acute disorders of cerebral circulation have a localization of the lesion in the cerebellum. Men of middle and retirement age suffer more often. What are the characteristic symptoms of the disease and how to treat such a stroke? The answers to these questions are in our article.
Types of cerebellar stroke
According to the standard classification based on pathogenesis, two types of cerebellar stroke are distinguished:
- ischemic;
- hemorrhagic.
According to statistics, the first type significantly predominates. Ischemic lesions of the cerebellum, according to various sources, account for 80 to 90 percent of cases. However, according to expert forecasts, within 50 years the number of diseases with a hemorrhagic nature is expected to double - the result of aging and changes in the racial composition of the planet's population.
Ischemic cerebellar stroke
The development of ischemic damage to the cerebellum is based on partial or complete blockage of blood vessels bringing arterial blood by a thrombus. In this regard, nerve cells stop receiving oxygen and nutrients. As is known, nervous tissue is very sensitive to hypoxia, and if blood flow is not normalized, neurons begin to die.
Hemorrhagic cerebellar stroke
With the hemorrhagic nature of the disease, a sharp disruption of the blood supply to the cerebellum occurs due to rupture of the artery or capillary feeding this structure. Due to the anatomical features of blood circulation, the consequences of a vascular accident are very difficult to predict, since the brain stem is often involved in the pathological process.
Diagnostics
To confirm the diagnosis of cerebellar stroke, an ultrasound is performed. The study allows you to determine the displacement, see the area of edema, and detect a damaged artery.
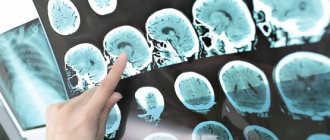
An informative diagnostic method is magnetic resonance imaging or computed tomography. Both methods provide an accurate picture of the changes, the size of the damage, the depth, and detect the cause of the disease.
A blood test is taken for general formula and biochemistry. The data will allow you to identify the level of sugar, cholesterol, and other substances that are signs of the diseases that provoked the attack.
Symptoms of cerebellar stroke
The clinical picture of both ischemic and hemorrhagic disorders of the blood supply to the cerebellum is varied, but there are characteristic symptoms that make it possible to suspect damage to the blood vessels in this particular area. These include cerebellar ataxia. This syndrome is associated with the functional activity of the cerebellum and includes:
- Balance imbalance. The patient cannot stand steadily and sways in different directions when walking.
- Changes in speech. Disturbance in the flow of arterial blood into the cerebellum is accompanied by scanned speech. The patient loudly tries to pronounce ordinary words.
- Loss of precision in movements. It is difficult for the patient to control fine motor skills, movements become sweeping.
- Tremor. Trembling of the limbs, head, and torso appears.
- Nystagmus. The eyeballs make involuntary oscillatory movements. Their frequency can reach several hundred per minute.
Among the general symptoms characteristic of acute cerebral circulation disorders are headache, dizziness, spontaneous vomiting, fever, loss of consciousness, difficulty swallowing, and muscle paralysis.
Ischemic stroke in the posterior cerebral arteries: problems of diagnosis and treatment
I.A. KHASANOV, E.I. BOGDANOV
Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, Kazan
Kazan State Medical University
Khasanov Ildar Akramovich
doctor of the neurological department for patients with acute cerebrovascular accidents
420064, Kazan, st. Orenburgsky Trakt, 138, tel. (843) 237-35-47, e-mail
In the light of modern data, the article examines the problems of diagnosis and treatment of ischemic strokes in the posterior cerebral arteries (PCA), taking into account the characteristics of their etiology, clinical picture and neuroimaging data. The paired posterior cerebral arteries, formed by the bifurcation of the basilar artery and being its terminal branches, serve as the main sources of blood supply to the upper part of the midbrain, the thalami and the posteroinferior parts of the cerebral hemispheres, including the occipital lobes, the mediobasal parts of the temporal lobes and the inferomedial parts of the vertex. Ischemic strokes in the posterior cerebral artery basin account, according to various sources, from 5-10 to 25% of cases of all ischemic strokes. The most common cause of isolated infarctions in the PCA territory is embolic occlusion of the PCA and its branches, which occurs in approximately 82% of cases. In 9% of cases, thrombosis in situ is detected in the PCA; in another 9% of cases, the cause of stroke is vasoconstriction associated with migraine and coagulopathy. A very rare cause of infarction in this region can also be arterial dissection affecting the PCA. The most common and characteristic signs of infarctions in the PCA region are visual disturbances (homonymous hemianopsia), central paresis of the facial nerve, headache, sensory disturbances, aphasic disorders, hemiparesis and nigility.
Key words:
ischemic stroke, cerebral infarction, posterior cerebral artery, neuroimaging, thrombolytic therapy
I.A. KHASANOV, EI BOGDANOV
Kazan State Medical University
Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, Kazan
Ischemic stroke in a system of posterior cerebral arteries: problems of diagnosis and treatment
In the article on the basis of present knowledge are considered the problems of diagnosis and treatment of ischemic strokes in a system of posterior cerebral arteries (PCA) taking into account their causation, clinical presentation and neuroimaging data. Paired posterior cerebral arteries, which are shaped by basilar artery bifurcation and are its terminal branches, are the main sources of blood supply of the upside of midbrain, thalamus and back and bottom parts of cerebral hemispheres, including occipital lobes, mediobasal branches of temporal lobes and lower medial crown branches. Ischemic strokes in a system of posterior cerebral arteries amount to 5-10% or up to 25% of all ischemic strokes. The most common cause of isolated heart attacks
in a system of PCA is the embolic occlusion of PCA and its branches, which occurs in about 82% of cases. In 9% of cases in PCA is revealed thrombosis, in other 9% of cases the cause of stroke are vasoconstriction associated with migraine, and coagulopathy. A very rarely reason for a heart attack in this system can be artery dissection which affects the PCA. The most frequent and characteristic features of heart attacks in a system of PCA are visual impairments (equilateral hemianopsia), central paresis of facial nerve, headache, sensation disorders, aphatic disorders, hemiparesis and neglect.
Key words:
ischemic stroke, cerebrovascular accident, posterior cerebral artery, neuroimaging, thrombolytic therapy.
Ischemic strokes in the posterior cerebral arteries (PCA) account, according to various sources, from 5-10 to 25% of cases of all ischemic strokes [1-4]. They can be the cause of a number of clinical symptoms, which are not always promptly and adequately recognized by the patients themselves, their relatives and doctors, because an acute gross motor deficit, which is usually associated with a stroke, in this case may be unexpressed or completely absent. A delay in timely diagnosis or incorrect diagnosis casts doubt on the possibility of providing the patient with adequate therapy (primarily thrombolysis), which in turn cannot but affect the outcome of the disease [5]. An important role in making a diagnosis is played by the possibility of using neuroimaging, the correct choice of method and competent interpretation of the results [2]. It seems important to present and analyze the features of the clinical picture, neuroimaging and treatment of ischemic strokes in the posterior cerebral arteries in the light of modern data.
The most common cause of isolated infarctions in the PCA territory is embolic occlusion of the PCA and its branches, which occurs in 82% of cases. At the same time, cardiogenic genesis is observed in 41% of cases, while arterio-arterial embolism from the vertebral and basilar arteries is observed in only 32% of cases. In 10% of patients, the source of the embolism cannot be determined. In 9% of cases, thrombosis in situ is detected in the PCA. Vasoconstriction associated with migraine and coagulopathies are the causes of cerebral infarction in 9% of cases [6]. If isolated infarctions in the PCA territory in most cases are of a cardioembolic nature, then involvement of the brainstem and/or cerebellum in combination with an infarction in the PCA territory is most often associated with atherosclerotic lesions of the vessels of the vertebrobasilar system [7, 8]. A very rare cause of infarction in this region can also be arterial dissection affecting the PCA [9]. Regardless of the cause of the infarction, it usually only partially involves the PCA territory [10, 11].
Paired posterior cerebral arteries, formed by the bifurcation of the basilar artery and being its terminal branches, serve as the main sources of blood supply to the upper part of the midbrain, thalamus and posteroinferior parts of the cerebral hemispheres, including the occipital lobes, mediobasal parts of the temporal lobes and inferomedial parts of the vertex [10, 12, 13].
In the early stages of development of the human body, the posterior cerebral artery is a branch of the internal carotid artery (ICA) and is supplied with blood from the carotid system, while the posterior communicating artery (PCA) plays the role of its proximal segment. Subsequently, blood begins to flow into the posterior cerebral arteries from the main artery, and the PCA, being a branch of the internal carotid artery, becomes the most significant anastomosis between the carotid and vertebrobasilar areas. According to various sources, from 17 to 30% of adults have a fetal (embryonic) type of PCA structure, in which the ICA remains the main source of blood supply to the PCA throughout life. The fetal type of PCA structure is in most cases observed unilaterally, with the opposite PCA usually starting from an asymmetrically located, curved basilar artery. In cases where both posterior cerebral arteries are branches of the internal carotid arteries, as a rule, well-developed large posterior communicating arteries are observed, and the superior segment of the basilar artery is shorter than usual (the basilar artery ends with the two superior cerebellar arteries arising from it). In approximately 8% of cases, both PCAs originate from the same ICA [7, 8, 12, 14, 15].
The PCA joins the PCA approximately 10 mm distal to the bifurcation of the basilar artery. Each PCA can be conditionally divided into 3 parts: the precommunication part, or P1 segment according to Fisher, - the section of the PCA proximal to the place where the PCA flows into it, the postcommunication part, or P2 segment, located distal to the place where the PCA flows into the PCA, and the final (cortical) the part that gives off branches to the corresponding areas of the cerebral cortex [12, 16]. The paramedian mesencephalic, posterior thalamoperforating and medial posterior choroidal arteries depart from the precommunicative part, participating primarily in the blood supply to the ventrolateral nuclei of the thalamus and the medial geniculate body. The left and right posterior thalamoperforating arteries may arise from a common trunk called the artery of Percheron; a similar variant of the structure usually occurs in combination with unilateral hypoplasia of the P1 segment and the fetal structure of the PCA. The branches of the postcommunication part are the peduncular perforator, thalamogeniculate and lateral posterior choroidal arteries, supplying the lateral geniculate body, dorsomedial nuclei and thalamic cushion, part of the midbrain and the lateral wall of the lateral ventricle [2, 12, 17]. The main cortical branches of the PCA are the anterior and posterior temporal, parietotemporal and calcarine arteries [10]. The boundaries of the watershed of the middle and posterior cerebral arteries basins fluctuate significantly. Usually the border of the PCA basin is the Sylvian fissure, but sometimes the middle cerebral artery supplies blood to the outer parts of the occipital lobe up to the occipital pole. At the same time, the PCA always supplies blood to areas of the cerebral cortex in the area of the calcarine sulcus, and the optic radiation in some cases receives blood from the middle cerebral artery; accordingly, homonymous hemianopsia does not always imply a heart attack in the PCA territory [12].
With ischemic strokes in the PCA region, depending on the location of the vessel occlusion, as well as on the state of collateral blood supply, the clinical picture may reveal symptoms of damage to the midbrain, thalamus and cerebral hemispheres. In general, up to 2/3 of all infarctions in the PCA territory are cortical, the thalamus is involved only in 20-30% of cases, and the midbrain in less than 10% of cases [7, 18, 19]. Accordingly, the most common variant of ischemic stroke in the PCA basin is an isolated infarction of the cerebral hemispheres, primarily the occipital lobes; combined damage to the thalamus and cerebral hemispheres is less common, in a small percentage of cases - an isolated infarction of the thalamus and, finally, a combination of damage to the midbrain, thalamus and /or hemispheres is the rarest option [2].
Sometimes there is bilateral damage to areas of the brain supplied by blood from the PCA. This occurs primarily in top of the basilar syndrome, which is an embolic occlusion of the distal basilar artery and is characterized by depression of consciousness, visual disturbances, oculomotor and behavioral disorders, often without motor dysfunction [2].
According to a number of authors, the most common and characteristic signs of infarctions in the PCA are visual disturbances (up to 95% of cases), homonymous hemianopia (66.7% of cases), central paresis of the facial nerve (52% of cases), headache, mainly in the occipital region. areas (50 cases), sensory disorders (40% of cases), aphasic disorders (38% of cases), hemiparesis (18% of cases) and niglect (10% of cases). Patients usually have a combination of symptoms [2, 7, 8, 11].
Homonymous hemianopia occurs on the contralateral side with infarctions in the areas of blood supply to the hemispheric branches of the PCA due to damage to the striate cortex, optic radiation or lateral geniculate body. In the absence of occipital pole involvement, macular vision remains intact. The visual field defect may be limited to only one quadrant. Superior quadrant hemianopsia occurs when there is an infarction of the striate cortex below the calcarine sulcus or inferior part of the optic radiation in the temporo-occipital region. Inferoquadrant hemianopsia is a consequence of damage to the striate cortex above the calcarine sulcus or the superior part of the optic radiation in the parieto-occipital region. Occlusion of the calcarine sulcus may also be associated with pain in the ipsilateral eye. Visual disturbances may also be more complex, especially with bilateral occipital lobe lesions, including visual hallucinations, visual and color agnosia, prosopagnosia (agnosia for familiar faces), blindness denial syndrome (Anton syndrome), visual attention deficits, and optomotor agnosia ( Balint's syndrome). Often, visual impairment is accompanied by afferent disorders in the form of paresthesia, disorders of deep, pain and temperature sensitivity. The latter indicate involvement of the thalamus, parietal lobe or brainstem (due to occlusion of the proximal vertebrobasilar region) [2, 8, 10, 20].
Neuropsychological abnormalities associated with PCA infarctions vary significantly and are present in more than 30% of cases. A stroke in the basin of the callosal branches of the left PCA in right-handed people, affecting the occipital lobe and splenium of the corpus callosum, is manifested by alexia without agraphia, sometimes color, object or photographic anomia. Right hemisphere infarctions in the PCA territory often cause contralateral hemiglect. With extensive infarctions involving the medial parts of the left temporal lobe or bilateral mesotemporal infarctions, amnesia develops. Also, with mono- or bilateral mesotemporal infarction, agitated delirium may develop. Extensive infarcts in the territory of the left posterior temporal artery may clinically manifest as anomia and/or sensory aphasia. Thalamic infarctions in the areas of blood supply to the penetrating branches of the PCA can cause aphasia (if the left pillow is involved), akinetic mutism, global amnesia and Dejerine-Roussy syndrome (disorders of all types of sensitivity, severe dysesthesia and/or thalamic pain and vasomotor disturbances in the contralateral half of the body, combined with usually transient hemiparesis, choreoathetosis and/or ballism). Also, infarctions in the PCA region may be associated with dyscalculia, spatial and temporal disorientation. [6, 12, 21, 22].
Bilateral thalamic infarcts are often associated with deep coma. Thus, occlusion of the Percheron artery causes the development of bilateral infarcts in the intralaminar nuclei of the thalamus, which leads to severe impairment of consciousness [2, 12].
Hemiparesis during infarctions in the PCA region occurs in only 1/5 of patients, is often mild and transient and is usually associated with involvement of the cerebral peduncles in the pathological process [23, 24]. Cases of infarctions in the PCA region have been described, when patients exhibited hemiparesis without involvement of the cerebral peduncles. These patients had damage to the distal parts of the PCA, primarily involving the thalamogeniculate, lateral and medial posterior choroidal arteries [23, 25]. It is assumed that hemiparesis during infarctions in the posterior choroidal arteries may be associated with damage to the corticobulbar and corticospinal tracts, even in the absence of visible damage to the internal capsule or midbrain according to neuroimaging data [23]. There are opinions that the development of hemiparesis is associated with compression of the internal capsule by edematous tissue of the thalamus [12].
Infarctions in the PCA territory mimic infarctions in the carotid system in 17.8% of patients [24], especially with combined lesions of the superficial and deep branches of the PCA, which is observed in approximately 38% of cases [7, 19, 26]. Differential diagnosis can be difficult due to the presence of aphasic disorders, nigella, sensory deficits, and usually mild and transient hemiparesis resulting from the involvement of the pyramidal tracts. In addition, memory impairment and other acute neuropsychological disorders can significantly complicate the examination of such patients [2, 18, 19].
Among other conditions that often clinically mimic infarctions in the PCA, we should highlight some infectious diseases (primarily toxoplasmosis), posterior reversible leukoencephalopathy syndrome, neoplastic lesions, both primary and metastatic, and thalamic infarctions caused by deep cerebral vein thrombosis [2 , 27]. Neuroimaging methods often play a decisive role in making a diagnosis.
The main requirements for neuroimaging in the acute period of ischemic stroke are the speed of the study and the information content of the data obtained. The main tasks facing the doctor when using these methods are to exclude a non-ischemic cause of the patient’s symptoms, determine the location and size of ischemic foci and the presence of viable brain tissue, determine the condition of the cerebral vessels, identify cerebral edema and displacement of the midline structures, as well as the presence of hemorrhagic impregnation of ischemic foci. These data should help in quickly determining the patient’s treatment tactics—the possibility of intravenous or intra-arterial thrombolysis, mechanical plaque removal, and brain decompression surgery [28, 29].
Computed tomography (CT) usually does not detect ischemic changes in the brain parenchyma during the first few hours after the onset of stroke, the time most important for initiating therapy, and sometimes even later in the disease. Visualization of the posterior regions of the brain is especially difficult due to artifacts caused by the bones of the skull. However, with strokes in the territory of the PCA, as well as with strokes in the territory of the middle cerebral artery, in some cases, CT may show a hyperintense signal from the PCA itself, which is the earliest sign of a stroke in its territory and is detected in 70% of cases within the first 90 minutes from onset of the disease and in 15% of cases within 12 to 24 hours. This sign appears due to visualization of a calcified embolus or atherothrombosis in situ. On a standard CT scan, the slice plane is parallel to the orbitomeatal line (the line connecting the outer corner of the eye with the external auditory canal and then going to the first cervical vertebra). Based on the course of the SMA, its lumen is usually visualized in one section, which makes it easy to identify hyperdense SMA, especially in the presence of atrophic changes in the brain. The course of the PCA is more complex. Typically, its proximal segment ascends laterally around the cerebral peduncles and, reaching the bypass cistern, goes horizontally inward to the temporal lobe, in close proximity to the tentorium cerebellum. The circular part (P1 and P2 segments) ends in the quadrigeminal cistern, where the cortical part of the PCA begins. Only the P2 segment runs parallel to the cut inside the bypass tank and, accordingly, hyperdensity, if present, can most likely be detected in this area. Subsequently, CT signs of ischemic changes appear as areas of hypointensity in the brain parenchyma [2, 3, 30].
Magnetic resonance imaging (MRI) makes it possible to more accurately determine the presence and nature of ischemic changes in the brain during stroke. Diffusion-weighted imaging (DWI) can detect early ischemic changes, often within an hour of symptom onset, and localize and extend lesions more accurately than CT [2]. The combined use of DWI, ADC and FLAIR modes makes it possible to differentiate acute, subacute and chronic ischemic changes in the brain parenchyma, as well as to distinguish cytotoxic brain edema observed in ischemic stroke from vasogenic edema in the syndrome of posterior reversible leukoencephalopathy and hypertensive encephalopathy [2, 27, 31 , 32].
CT angiography (CTA) plays a significant role in the non-invasive diagnosis of steno-occlusive lesions of large extra- and intracranial arteries. This technique makes it possible to identify the degree of stenosis, plaque morphology, as well as the presence of arterial dissection in both vertebrobasilar and carotid vessels. In addition, the anatomical features of collaterals and circulation options of the PCA are assessed [2, 33, 34]. Additional information about vascular anatomy can be obtained using contrast-enhanced MR angiography, which, in combination with CTA, allows for data that previously could only be obtained using classical angiography. In addition, these methods are important in assessing the effectiveness of thrombolytic therapy in the case of arterial recanalization [2].
Currently, thrombolytic therapy for ischemic stroke can be used for damage to the arteries of both the carotid and vertebrobasilar areas. Nevertheless, all currently existing guidelines for thrombolysis are focused primarily on vascular catastrophe in the carotid region, primarily the middle cerebral artery; this is primarily due to the presence in such patients of obvious neurological deficits in the form of severe paresis and sensory disturbances. A typical functional deficit in a patient with a heart attack in the PCA region in the acute period is not always regarded by the doctor as disabling. The assessment of neurological deficit according to the National Institutes of Health Stroke Scale (NIHSS), which is one of the criteria for selecting patients for thrombolytic therapy, usually is not able to fully reflect the severity of the condition of a patient with a vertebrobasilar infarction [7]. There are no recommendations at all regarding an isolated visual field defect in acute infarction in the PCA territory [2]. Therefore, thrombolytic therapy in patients with infarctions in the PCA is not widely used. However, given that hemiparesis in some cases is a significant clinical component of infarctions in the PCA territory, such patients, in the absence of contraindications, are justifiably treated with systemic and/or intra-arterial thrombolysis [35].
When comparing the efficacy and safety profiles of intravenous thrombolysis administered within the first three hours from the onset of symptoms in patients with carotid infarctions and PCA infarctions, no significant difference in safety and treatment outcome was found [7]. At the same time, according to a number of authors, when conducting intravenous thrombolytic therapy for ischemic lesions in the vertebrobasilar region, and in particular the PCA, it is possible to expand the therapeutic window to 6.5-7 hours and even more compared to 4.5 hours for infarctions in the carotid pool [36, 37].
Intra-arterial thrombolysis for occlusion of the middle cerebral artery is recommended within 6 hours from the onset of symptoms, and for occlusion of the basilar artery - no later than 12 hours [28]. However, to date there are no clear recommendations on the time limits for intra-arterial thrombolysis in patients with PCA lesions [15]. N. Meier et al. (2011) described 9 cases of intra-arterial thrombolysis in patients with PCA occlusion within the first 6 hours from the onset of the disease. 3 months after treatment, functional independence (modified Rankin scale 0-2 points) was detected in 67% of patients, which correlates with similar data for the carotid system [15].
An early diagnosis of ischemic stroke in the PCA allows the doctor to promptly determine the patient’s treatment tactics and, in the absence of contraindications, consider the possibility of thrombolytic therapy, which undoubtedly makes the prognosis for the patient more favorable.
LITERATURE
1. Brandt T., Steinke W., Thie A., Pessin MS, Caplan LR Posterior cerebral artery territory infarcts: clinical features, infarct topography, causes and outcome. Multicenter results and a review of the literature // Cerebrovasc. Dis. - 2000. - Vol. 10. - P. 170–182.
2. Finelli P. Neuroimaging in acute Posterior Cerebral Artery Infarction // The Neurologist. - 2008. - Vol. 14. - P. 170-180.
3. Krings T., Noelchen D., Mull M. et al. The hyperdense posterior cerebral artery sign // Stroke. - 2006. - Vol. 37. - P. 399-403.
4. Hill MD Posterior cerebral artery stroke // e-medicine, 2005.
5. Khasanov I.A. Features of infarctions in the basin of the posterior cerebral arteries // Neurological Bulletin. - 2012. - T. XLIV, issue. 3. - pp. 69-74.
6. Caplan L. Posterior Circulation Ischemia: Then, Now, and Tomorrow: The Thomas Willis Lecture-2000 // Stroke. - 2000. - Vol. 31. - P. 2011-2023.
7. Breuer L., Huttner H. B., Jentsch K. et al. Intravenous Thrombolysis in Posterior Cerebral Artery Infarctions // Cerebrovasc Dis. - 2011. - Vol. 31. - P. 448-454.
8. Caplan L., Bogousslavsky J. Posterior cerebral artery syndromes // Cerebrovascular Disease: Pathology, Diagnosis and Management. - 1998. - P. 1028.
9. Caplan L., Estol C., Massaro A. Dissection of the posterior cerebral arteries // Arch Neurol. - 2005. - Vol. 62. - P. 1138-1143.
10. Brazis P. Topical diagnostics in clinical neurology / P. Brazis, D. Masdew, H. Biller - M.: MEDpress-inform, 2009. - 736 p.
11. Caplan L. Posterior Circulation disease: Clinical Findings, Diagnosis and Management / Boston, MA: Butterworth-Heinemann, 1996. - 533 p.
12. Beer M. Topical diagnosis in neurology according to Peter Duus / M. Beer, M. Frotscher. - M.: Practical Medicine, 2009. - 468 p.
13. Tatu L., Moulin T., Bogousslavsky J. et al. Arterial territories of the human brain // Neurology. - 1998. - Vol. 50 - P. 1699-1708.
14. de Monye C, Dippel DW, Siepman TA et al. Is a fetal origin of the posterior cerebral artery a risk factor for TIA or ischemic stroke? A study with 16-multidetector-row CT angiography // J. Neurol. - 2008. - Vol. 255 - P. 239-245.
15. Meier N., Fischer U., Schroth G. Outcome after thrombolysis for acute isolated posterior cerebral artery occlusion // Cerebrovasc. Dis. - 2011. - Vol. 328. - P. 79-88.
16. Phan T., Fong A., Donnan G. et al. Digital map of posterior cerebral artery infarcts associated with posterior cerebral artery trunk and branch occlusion // Stroke. - 2007. - Vol. 38. - P.1805-1811.
17. Chaves CJ Posterior cerebral artery. Stroke syndromes. 2nd edition / Chaves CJ, Caplan LR Cambridge, New York: Cambridge University Press. — 2001. — 747 p.
18. Cals N., Devuyst G., Afsar N. et al. Pure superficial posterior cerebral artery territory infarction in the Lausanne Stroke Registry // J. Neurol. - 2002. - Vol. 249. - P. 855-861.
19. Kumral E., Bayulkem G., Atac C., Alper Y. Spectrum of superficial posterior cerebral artery territory infarcts // Eur. J. Neurol. - 2004. - Vol. 11. - P. 237-246.
20. Ng YS, Stein J, Salles SS et al. Clinical characteristics and rehabilitation outcomes of patients with posterior cerebral artery stroke // Arch. Phys. Med. Rahabil. - 2005. - Vol. 86. - P. 2138-43.
21. Brandt T., Thie A., Caplan L. et al. Infarkte in Versorgungsgebiet der A. cerebri Posterior // Nervenarzt. - 1995. - Vol. 66. - P. 267-274.
22. Savitz SI, Caplan LR Vertebrobasilar disease // N. Engl. J. Med. - 2005. - Vol. 352. - P. 2618-26.
23. Finelli P. Magnetic Resonance Correlate of Hemiparesis in Posterior Cerebral Artery Infarction // Journal of Stroke and Cerebrovascular Disease. - 2008. - Vol. 17. - P. 378-381.
24. Maulaz AB, Bezerra DC, Bogousslavsky J. Posterior cerebral artery infarction from middle cerebral artery infarction // Arch. Neurol. - 2005. - Vol. 62. - P. 938-941.
25. Neau J.-P., Bogousslavsky J. The syndrome of posterior choroidal artery territory infarction // Ann. Neurol. - 1996. - Vol. 39. - P. 779-788.
26. Lee E., Kang DW, Kwon SU, Kim JS Posterior cerebral artery infarction: diffusion-weighted MRI analysis of 205 patients. Cerebrovasc. Dis. - 2009. - Vol. 28. - P. 298-305.
27. Bogdanov E.I., Khasanov I.A., Mamedov Kh.I. and others. Posterior reversible leukoencephalopathy syndrome in patients with preeclampsia and eclampsia // Neurological Journal. - 2011. - No. 5. - P. 35-40.
28. Adams H., Del Zoppo G., Alberts M. et al. Guidelines for the early management of adults with ischemic stroke // Stroke. - 2007. - Vol. 38. - P. 1655-1711.
29. Wahlgren N., Ahmed N., Davalos A. et al. Thrombolysis with alteplase for acute ischemic stroke & the Safe implementation of thrombolysis in stroke - monitoring study (SITS-MOST): an observational study // Lancet. - 2007. - Vol. 369. - P. 275-282.
30. Berge E., Nakstad PH, Sandset PM Large middle cerebral artery infarctions and the hyperdense middle cerebral artery sign in patients with atrial fibrillation // Acta Radiol. - 2001. - Vol. 42. - P. 261-268.
31. Covarrubias DJ, Leutmer PH, Caumpeau NG Posterior reversible leukoencephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR image // AJNR Am J. Neuroradiol. - 2002. - Vol. 23, N 6. - P. 1038-1048.
32. Garg R. Posterior leukoencephalopathy syndrome // Postgrad. Med. J. - 2001. - Vol. 77, N 903. - P. 24-28.
33. Choi C., Lee D., Lee J. et al. Detection of intracranial atherosclerotic steno-occlusive disease with 3D time-of-flight magnetic resonance angiography with sensitivity encoding at 3T // AJNR Am J. Neuroradiol. - 2007. - Vol. 28. - P. 439-446.
34. Lev M., Farkas J., Rodrigues V. et al. CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus // J Comput Assist Tomogr. - 2001. - Vol. 25. - P. 520-528.
35. Ntaios G., Spengos K., Vemmou AM et al. Long-term outcome in posterior cerebral artery stroke // European Journal of Neurology. - 2011. - P. 156-162.
36. Forster A., Gass A., Kern R. et al. MR Imaging-Guided Intravenous Thrombolysis in Posterior Cerebral Artery Stroke // AJNR Am J. Neuroradiol. - 2011. - Vol. 32. - P. 419-421.
37. Montavont A., Nighoghossian N., Derex. L et al. Intravenous r-TPA in vertebrobasilar acute infarcts // Neurology. - 2004. - Vol. 62. - P. 1854-1856.
Causes and factors of cerebellar stroke
The ischemic type of cerebellar stroke is usually considered the outcome of atherosclerotic disease. The thrombus travels through the vertebral or basilar artery through the bloodstream. Embolism can also occur with fresh myocardial infarction or atrial fibrillation. Surgical interventions on the neck are very dangerous, since during their implementation it is possible to traumatize the vertebral arteries with further disruption of blood flow.
The main causes of hemorrhagic stroke of the cerebellum:
- high blood pressure or sudden changes;
- cerebral amyloid angiopathy - deposition of amyloid in small blood vessels through which blood enters the central nervous system;
- taking antithrombotic drugs (“blood thinners”);
- neoplasms;
- inflammatory diseases of the walls of blood vessels.
Wrong lifestyle
In addition to the immediate causes, risk factors play a significant role in the development of cerebellar stroke. One of the key ones is the wrong lifestyle. It includes:
- low mobility during the day;
- food based on foods high in fat and sodium;
- smoking, alcohol abuse, taking narcotic drugs;
- constant nervous tension, chronic stress.
These factors contribute to disruption of normal blood circulation in organs, including the nervous system.
Diseases and medications
Diseases of the internal organs can provoke a cerebellar stroke. The relationship between cerebral circulatory disorders and the following somatic diseases has been proven:
- arterial hypertension;
- metabolic syndrome, accompanied by high levels of cholesterol and low-density lipoproteins in the blood;
- diabetes mellitus and other endocrine pathologies;
- cardiac ischemia;
- diseases in which blood clotting increases.
Uncontrolled use of medications that affect the functioning of the heart, change hormonal levels, and thin the blood can also cause acute impairment of cerebral circulation (including in the cerebellum).
Other reasons
Other causes of vascular accident include genetic predisposition and age factor. A number of genes are currently being studied that are potentially associated with an increased risk of cerebral circulatory disorders.
Causes of hemorrhage
The trigger mechanism for hemorrhage in the cerebellum is most often hypertension. Basically, the reasons for this type of hemorrhage do not differ from the reasons for the occurrence of other types of strokes that affect the brain. Most often these are the following phenomena and conditions:
- A sharp rise in blood pressure;
- Severe anxiety, stress;
- Physical fatigue;
- Intense mental activity;
- Taking inappropriate medications;
- Alcohol consumption;
- Excessive overheating (in the sun, in a bath, a very hot bath, and so on);
- Smoking can cause vascular damage, which, in turn, starts a whole chain of diseases, ultimately leading the patient to stroke, paralysis or death.
First aid for stroke
When providing first aid, it is necessary to understand what a cerebellar stroke is, otherwise there is a huge risk of harming the patient. The main goal is to prevent further death of neurons, and inept and incorrect actions can lead to extremely negative consequences. Recommend:
- Lay the patient on the bed, if the circulatory disorder occurred at home, or on the ground, slightly elevate the torso.
- Turn your head to the side to avoid vomit getting into your respiratory tract.
- Seek medical attention immediately.
- Try to calm the victim down and calm down yourself.
- Provide sufficient fresh air and avoid tight clothing.
Stroke treatment
The volume, tactics and duration of treatment depend on the type of vascular disorder. Common activities include:
- Ensuring the supply of oxygen to brain tissue.
- Correction of blood pressure indicators.
- Prevention of convulsive syndrome.
- Maintaining water-electrolyte and energy balance, normal body temperature.
Drug treatment of cerebellar stroke
The use of medications is possible only after the cause of the vascular accident has been established. For the treatment of ischemic stroke of the cerebellum, the following is used:
- Thrombolytics. Such drugs are able to dissolve blood clots in blood vessels, relieving areas of nervous tissue from ischemia.
- Neuroprotectors. Used to reduce the sensitivity of neurons to oxygen starvation. The use of these drugs allows you to avoid further death of nerve cells and gradually restore the functions of damaged areas.
- Diuretics are medications that help fight swelling of the brain.
In the treatment of acute circulatory disorders in the cerebellum of the hemorrhagic type, neuroprotectors and diuretics are also used, but the key drugs are hemostatic agents.
The amount of drug therapy is selected individually for each patient. It expands in the presence of paralysis, concomitant somatic or endocrine pathology.
Surgery
In parallel with drug treatment, the issue of surgical intervention is being resolved. Its functions:
- Removal of a blood clot or hematoma.
- Redistribution of blood flow to supply affected areas of nervous tissue.
- Stopping bleeding when drug therapy is ineffective.
Traditional surgery is performed openly or using an endoscope.
Rehabilitation
During the recovery period, a set of measures is used: physiotherapy, drug treatment, massage, classes with psychologists and speech therapists.
Depending on the clinical picture and each individual case, rehabilitation courses are selected individually.
Their main goals are:
- restoration of motor functions and motor skills;
- renewal of everyday skills;
- speech restoration;
- memory restoration.
The rehabilitation period depends on the severity of the disease. On average, it takes six months or more for the patient to feel significant improvements.
After a stroke, to minimize the possibility of relapse, you must adhere to the following recommendations:
- monitor blood cholesterol levels;
- undergo MRI periodically;
- control blood pressure levels;
- avoid stressful situations;
- do not give in to bad habits: smoking, drinking alcohol;
- If possible, play sports and lead a healthy lifestyle.
Recovery and rehabilitation after cerebellar stroke
Early initiation of rehabilitation treatment makes it possible to more effectively activate the relationship between neurons, returning lost functions to nerve structures. Rehabilitation measures should be varied and include both medications and physical procedures, special physical exercises, and occupational therapy. The main goals of rehabilitation treatment:
- regaining control over motor activity;
- normalization of speech;
- restoration of lost self-care skills;
- improvement of muscle tone after paralysis;
- prevention of complications (contractures).
The cerebellum and its functions
Below the occipital hemispheres in the lower part of the skull, close to the spinal column, is the cerebellum. It consists of two hemispheres and a worm. The weight of an adult reaches 160 g. At the time of birth, the child is very small, but is distinguished by noticeable development during the first year of life. By the age of 6 it reaches the minimum size for an adult.
On top, the cerebellum is covered with gray matter, inside it consists of white matter - it contains four nuclei.
Nutrition is provided by three cerebellar arteries, originating from the vertebral and main trunks.
The cerebellum receives information about the current position of the body or its parts. At the same time, an adjustment comes to him from the cerebral cortex regarding what next movement needs to be made. This allows him to correct voluntary and involuntary actions.
The main functions of this part of the brain are coordination of movements, regulation of muscle tone, balance, and muscle memory.
- Stroke on the left side: consequences and features of recovery. How long do people live with this diagnosis?
Stroke in the cerebellum: possible consequences, prognosis
Despite its low prevalence, cerebellar stroke has a poor prognosis for the patient and is accompanied by high mortality, reaching thirty percent or more. Common consequences of cerebellar stroke:
- Disability. According to statistics, only 20% of patients who have suffered an acute cerebellar circulatory disorder are able to care for themselves independently by six months from the onset of the disease. The rest of the victims need help from others.
- Paresis and paralysis. Restoration of motor activity in damaged limbs is slow and not always complete.
- Speech impairment. Some patients still have scanned speech.
Often such severe consequences of a cerebellar stroke cause despair in the patient. However, you should not give up: daily rehabilitation activities can partially or even completely restore lost skills.
Forecast
At the moment, acute manifestations of cerebellar stroke are practically impossible to treat. Unfortunately, almost all patients with severe manifestations of hemorrhage in the cerebellum do not survive, even if they receive appropriate medical care in a timely manner.
Basically, hemorrhage into the cerebellum, the consequences of which can be very severe even if the patient survives, is characterized by high mortality and dangerous complications. The situation is also aggravated by the age of the patient - mostly old people have a large “set” of chronic diseases and a greatly weakened body, which has difficulty resisting such a serious lesion as a stroke.
For a faster and better recovery for a patient who has experienced hemorrhage, it is important to create a calm, friendly, emotionally balanced atmosphere. His family and friends will have to show maximum tact, as the patient can be irritable, capricious and even whiny. Only a gentle attitude and love, combined with competent professional treatment, can return a person to a normal, fulfilling life.
Stroke Prevention
To prevent acute cerebral circulatory disorders, WHO specialists have developed simple recommendations:
- Control and correction of blood pressure.
- Prevention of heart rhythm disturbances.
- Minimizing risk factors.
- Annual examination of the condition of the great vessels.
- Monitoring blood parameters.
Cerebellar stroke is an extremely serious disease, but a number of modern diagnostic and treatment methods increase patient survival and improve their quality of life in the future.
First aid
If there is a suspicion that a stroke is developing, then the most important thing is to immediately call an ambulance .
Then you need to check whether the person can breathe, help him by emptying the oral cavity in a position lying on his side. If possible, record blood pressure and pulse readings. If the patient is on the floor, then lay him on his back, placing a towel folded in several layers under his head. It is very important to establish when the attack occurred, this will help in the correct prescription of therapy. You cannot independently lower blood pressure, give water, and especially feed the patient.
First aid for stroke