When carrying out diagnosis and treatment, it is necessary to establish the location of the damage, the degree of stenosis and its causes. Therefore, patients are prescribed a wide diagnostic program, as well as treatment methods - today they are varied and effectively eliminate the problem.
Most often, the disease affects extracranial vessels, but pathology of intracranial arteries also occurs. This condition is responsible for half of the clinical cases of cerebral ischemia and about 30% of strokes. There are complete and incomplete obstruction (blockage) of the vascular lumen, which lead to disruption of the blood supply.
Normally, the common carotid arteries arise: the left one from the aortic arch, and the right one from the brachiocephalic trunk. They are directed vertically and are located on either side of the cervical spine. Next, it divides into the external and internal carotid arteries. The branches of the arteries supply blood to the intracranial parts, parts of the face, and organs of the head and neck.
Causes
Vascular occlusions are associated with a state of vascular insufficiency. The occlusion process occurs:
- as a result of injuries, if the artery is compressed.
- due to the fact that the lumen is blocked by a thrombus or embolus.
The formation of blood clots is promoted by a chronic disease - vascular atherosclerosis. As atheromatous plaques grow and increase in diameter, they interfere with normal blood flow. Atherosclerotic plaque leads to blood clotting and blood clot formation. Occlusion is caused by separated plaque fragments that move freely along the vascular bed. In addition, as a result of atherosclerosis, the walls of blood vessels lose their elasticity, become thinner and stratify under blood pressure, which causes the formation of aneurysms. Thrombosis or embolism is likely to occur in the area of the vessel where the dilatation has appeared.
Forecast and preventive recommendations
If the arterial lumen is blocked by half, the disease may occur without obvious signs. With such a picture, the risk of developing apoplexy is 10% of all cases within five years. A 75% vascular blockage leads to a 6% stroke rate in the first year. Complete thrombosis of the canal leads to inevitable neurological damage in 40% of incidents. Preventive surgical intervention with or without prosthetics makes it possible to reduce these risks to a minimum.
To prevent the closure of vascular walls, it is recommended to get rid of bad habits, balance your diet, and monitor weight gain. The lipid composition of the blood is determined by regular testing. If necessary, therapeutic recommendations help adjust the composition of the blood solution. If cardiac abnormalities are present, supportive treatment should be provided promptly. In case of congenital diseases of the cardiovascular system, it is also recommended to undergo regular examination as prescribed by a cardiologist.
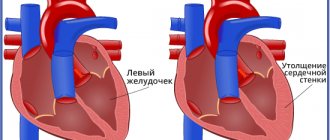
Occlusion of cardiac vessels
A dangerous condition is considered to be acute occlusion of the coronary arteries, which supply blood to the heart muscle. This occurs as a result of atherosclerosis of the coronary arteries and coronary heart disease. If, during the chronic course of the disease, a person experiences angina pectoris, then the acute form is fraught with a heart attack and even death of the patient. Typical signs of cardiac vascular occlusion are chest pain that lasts more than 10 minutes and does not go away with rest or after taking nitroglycerin. In this case, the concept of acute coronary syndrome is used: a patient with such symptoms should be immediately hospitalized.
The danger lies in the fact that a person initially ignores the symptoms of coronary artery disease or simply does not feel them without taking any measures. Vascular occlusion is characterized by suddenness and unexpectedness, so at the first signs of developing coronary artery disease, consult a doctor immediately.
What else causes stenosis?
More rare cases are associated with a specific pathology. Narrowing of the arterial vessel is observed with a disease of the connective tissue that forms the stroma of the artery. This is called fibromuscular dysplasia - the vessels cease to maintain tone and collapse, stopping blood flow. Stenosis can accompany some inflammatory diseases of the vascular wall - arteritis, systemic vasculitis, Takayasu's disease, Horton's disease. There are rare pathologies, for example moyamoya disease, in which there is a slow progressive narrowing of the lumen of the arteries.
Stenosis can occur after an injury - a strong blow, a concussion. After some traumatic brain injuries, a special hematoma is observed - subintimal, which has the appropriate localization. A blood clot that forms due to increased blood clotting and rare types of anemia can block the lumen. There is antiphospholipid syndrome, in which young patients experience heart attacks and strokes precisely because of increased coagulation. Blood clots form when heart rhythm disturbances occur while taking certain medications.
The narrowing may be due to congenital structural features of the vessels - they can be tortuous and hypoplastic. Vascular pathology accompanies systemic diseases, diabetes, obesity and metabolic disorders.
Peripheral vascular occlusion
Large arteries of the extremities, more often the lower ones, are susceptible to vascular occlusion. Occlusions are an unpleasant consequence of vascular diseases of the legs. At the same time, the threat of an acute occlusive process in this area is dangerous due to the development of tissue necrosis, which leads to amputation of the affected limb. Characteristic signs of thromboangiitis obliterans, atherosclerosis of leg vessels and other common pathologies are:
- pain in the legs that does not go away with rest;
- pallor of the skin of the extremities;
- coldness in the legs;
- tingling sensation, numbness in the limb;
- impairment of motor functions of the limb.
If these symptoms appear, it is recommended to immediately examine and treat the vessels of the extremities: the slightest delay can result in the development of gangrene. In the early stages of the development of the disease, treatment of obliterating atherosclerosis of the lower extremities and other pathologies of sclerotic origin is carried out using conservative methods, whereas in an advanced form it is difficult to fight the disease.
Occlusive processes occur in the arteries of the kidneys, resulting in the development of renovascular hypertension and kidney dysfunction. The aorta is also affected, since it is the largest vessel. Read about the consequences of aortic atherosclerosis by clicking on the link.
What manifestations are accompanied by the pathology?
The clinical manifestations of the disease depend on where the problem is located. Also, the nature of the onset of the disease, which can be sudden or gradual, plays an important role. It is worth remembering that in the first stages of the disease, compensatory mechanisms always turn on. For example, if the blood flow is partially disrupted, a system of collaterals develops, which will provide alternative routes for blood supply to the brain. The lack of oxygen supply is also compensated - the pulse and breathing become more frequent, intracellular processes change. For short-term conditions this is enough, but for serious pathologies it is not. In such cases, symptoms of the condition develop. Naturally, with an abrupt onset and significant stenosis, compensatory forces do not work and the clinical picture has a pronounced character, which indicates a stroke.
One of the first alarm signals is transient cerebral ischemia. These are short-term episodes of circulatory disturbance that can be compensated by collateral blood flow. The condition can be recognized by decreased sensitivity and motor activity, as well as visual disturbances. Patients usually complain of a feeling of numbness in the upper limb, half of the face, and loss of visual fields. Decreased muscle strength in the arm or forearm. The patient feels the movement of dark spots in front of the eyes, as well as a decrease in visual acuity. In some cases, the section of the artery that supplies the retina is affected. In some localizations, corresponding disorders occur - difficulty speaking, hearing, swallowing, facial asymmetry, severe pain. More common symptoms are dizziness, feeling unwell, weakness, and convulsions.
If stenosis develops gradually, the clinical picture also develops slowly. In some cases, it is so nonspecific that it is difficult to recognize the disease. For a long time, both the patient and the doctor may mistakenly believe that the cause of poor health is fatigue or increased stress. Also, the symptoms of occlusion overlap with the symptoms of a tumor process and dementia. This is indicated by increased irritability, depressive disorders, sudden changes in mood, increased drowsiness, decreased memory and mental abilities.
Nonspecific symptoms require a high level of responsibility from the patient and the doctor, since high-quality diagnosis is necessary. The diagnosis determines how correct the treatment of the pathology and the result will be.
Occlusion of blood vessels supplying blood to the brain
Occlusive processes in the arteries supplying the brain are fraught with dangerous consequences. Impairment of cerebral blood supply is fraught with the development of a stroke or ischemic cerebral infarction, and this often ends in the patient’s death, paralysis or dementia. A common cause of this is carotid artery occlusion. It is accompanied by loss of consciousness, nausea and vomiting, impaired coordination, speech and vision, weakness and numbness of the limbs. A harbinger of strokes are transient (cerebral) ischemic attacks, which we described in detail earlier.
Treatment and recovery methods
The basis of treatment in most cases is surgery. The tactics of surgical invasion are selected individually, depending on the degree of damage to the pathways, the location of the blood clot, and the level of alternative brain nutrition. With progressive apoplexy, mortality from surgery after 6-8 hours from the onset of the attack accounts for almost half of the episodes. That is why doctors try to start treatment before stroke changes form in the brain. After the first TI attacks, preventive treatment is carried out. With minimal neurological consequences, stenting and endarterectomy can be performed. Surgically, “bypass” pathways for blood supply to abnormal areas are created. To do this, stents (prostheses) are inserted into healthy areas of the carotid artery in the subclavian region.
Pathogenesis
When the blood thickens, there is an accumulation of fibrin in its composition, which leads to thrombus formation . Venous formations are characterized by constancy - they are located in one area and clog the vessels of the extremities, leading to necrosis and gangrene . Arterial formations are characterized by migration; they often break away from the original source and disrupt the blood supply to large organs, provoking the development of stroke , heart attack and other dangerous conditions.
Basic principles of nutrition
In case of deep vein thrombosis of the lower extremities, it is necessary to eat a balanced, varied diet. The diet should consist of fruits, vegetables, whole grain cereals, lean meat, and natural dairy products. All dishes must be baked or steamed. It is necessary to completely exclude fatty, fried, salty, and sweet sodas from the diet. You also need to minimize your consumption of sugar and flour products. This will help not only reduce the load on the cardiovascular system, but also strengthen the entire body.
Recommendations for the management of patients with central retinal artery occlusion
Central retinal artery occlusion (CRAO) is a form of acute ischemic stroke [1]. Despite more than 150 years of study, there are no effective proven forms of therapy for this condition. Restoration of functional visual acuity in the affected eye occurs in less than 20% of patients [2,3]. Similar to cerebral ischemic stroke, ACSA is associated with a risk of recurrent vascular events [4–8].
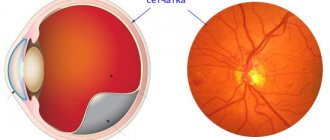
Definitions. OCSA is a circulatory disorder (thromboembolism, vasospasm) in the CAS or its branches with (or without) the development of infarction of the inner layers of the retina. The diagnosis of ACAS is made on the basis of classical clinical data (sudden painless loss of vision), impaired direct response to light and fundoscopy data (signs of retinal hypoperfusion). With retinal transient ischemic attack (amaurosis fugax), transient, painless monocular blindness occurs without residual visual impairment.
Anatomy. The anatomy of the arterial blood supply to the eye is shown in Fig. 1.
Figure 1. Arterial blood supply to the eye.
Classification:
— OCSA without arteritis (95%);
— OCSA in arteritis (5%, occurs in inflammatory diseases such as giant cell arteritis (GCA)) [9].
Epidemiology
Incidence of ACAS:
— 1.9 per 100,000 person-years in the USA [10];
— 1.8 per 100,000 person-years in South Korea [11];
- 2.5 per 100,000 person-years in Japan [12].
The incidence increases to 10.1 per 100,000 person-years in persons over 80 years of age [11]. The incidence is slightly higher in men than in women [11,13].
Etiology
OCSA is most closely associated with ipsilateral internal carotid artery (ICA) stenosis [16]. The incidence of ICA stenosis ≥70% in patients with OCSA in the study by Lavin P. et al (2019) was 37%, in the EAGLE study - 40% [17,18]. Another cause of ACAS is cardioaortic embolism (atrial fibrillation (AF) - 20%, valve defects - 17%, heart failure - 5%) [18]. According to the EAGLE study, 67% of patients have at least 1 cardiovascular risk factor [18]. Longer cardiac monitoring is associated with a higher detection rate of AF in patients with ACSA [22]. At the same time, OCSA in patients with AF increases the likelihood of recurrent stroke [21]. Rare causes of OCSA include a hypercoagulable state with thrombosis of the CAS [34] and iatrogenic injury (a complication of cosmetic facial injections when synthetic material accidentally enters the facial arteries anastomosing the ophthalmic artery) [35].
Diagnostics.
- sudden, painless monocular loss of visual acuity and peripheral vision (> 80% of patients have counting fingers visual acuity or worse). With a intact cilioretinal artery, central visual acuity is preserved, but its periphery is impaired.
- decreased direct reaction to light, while concomitant pupillary reaction is preserved (if there is no contralateral optic neuropathy).
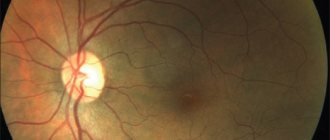
- Typical fundoscopy findings (Fig. 2): retinal edema (blanching of the retina), cherry red spot (preserved choroidal circulation surrounded by pallor due to retinal ischemia), slow segmental blood flow in the retinal arteries, direct visualization of emboli (<10% of cases) ). In this case, the optic disc usually looks normal (if there is disc swelling, the patient may have a rare combination of ACAS and anterior ischemic neuroopticopathy, more often observed in GCA). An ophthalmologic examination is also necessary to rule out other causes of vision loss (vitreous hemorrhage, chorioretinal hemorrhage, retinal detachment, and acute optic neuropathy). Additional imaging techniques (optical coherence tomography and angiography, fluorescein angiography) can confirm the diagnosis, especially in the absence of typical symptoms.
Figure 2.
A - normal picture (intact right eye), note normal fovea (thin arrow) and normal arteries (short arrows).
B – picture of OCSA in the left eye: diffuse retinal blanching (black arrow), cherry-red spot (yellow arrow), weakened arterial signal (orange arrows).
C – normal retina on optical coherence tomography of the right eye (normal retinal layers and fovea).
D - Optical coherence tomography of the left eye with acute OCSA (thickening and irregularity of the inner layers of the retina, consistent with edema secondary to acute retinal ischemia (white arrow)).
E, fibrin-platelet emboli in the superior branch of the retinal artery (red thin arrows) with slow segmental blood flow in the distal retinal arteries (red short arrow).
F – preservation of the cilioretinal artery in acute OCSA (diffuse blanching of the retina (black arrows) with a normal central area (white arrow) supplied by the cilioretinal arteries).
Arteritis in patients with ACAS should be suspected in patients over 50 years of age in the presence of systemic symptoms (intermittent claudication of the lower jaw, polymyalgia rheumatica, headache, increased inflammatory markers) [36–38]. An examination is indicated to detect ICA stenosis (ultrasound, CT - or MR angiography; when verifying stenosis, it is considered symptomatic), transthoracic/transesophageal echocardiography (detection of structural pathology of the heart), ECG monitoring (if AF is detected, a patient with ACAS has 2 points on the scale CHA2DS2-VASc for embolic event). Screening for less common causes of ACSA (including hypercoagulable states, paradoxical and septic embolism) should be considered in high-risk groups.
Natural history of the disease
A meta-analysis of 8 studies reporting the visual outcomes of 396 untreated patients with ACAS demonstrated that only 17.7% (70 of 396) of patients had functional visual recovery [2]. However, unilateral vision loss was associated with an increased likelihood of falls (OR 2.86 [95% CI, 1.16–7.08]) and functional dependence (OR 7.50 [95% CI, 1.97–28.6] ) [42].
Urgent Care.
Providing emergency care has 2 features:
1) examination of the fundus to confirm the diagnosis and exclude alternative causes,
2) evaluation for arteritis (for immediate steroid therapy to preserve vision in the contralateral eye) [48].
Stroke centers should develop relationships with local ophthalmologists to promptly admit patients with CASC within the therapeutic window for thrombolysis. Public awareness campaigns should highlight that painless unilateral vision loss is a possible symptom of stroke.
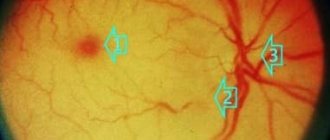
Help algorithm. Patients are advised to undergo an immediate ophthalmological and neurological examination, NIHSS score, CT scan of the brain without contrast (up to 30% of patients with ACAS have cerebral infarction on neuroimaging [56]), if coagulopathy is suspected, a blood test for platelet count and coagulogram, if suspected for GCA - assessment of ESR and C-reactive protein (before making a decision on thrombolysis). The help algorithm is shown in Fig. 3.
Intravenous thrombolytic therapy (ITT). In a meta-analysis of observational studies, Schrag M. et al. (2015) patients with acute ACSA who received TLT within 4.5 hours from the onset of symptoms showed clinical improvement in 50% (versus 17.7% in the group without TLT, OR 4.7 [95% CI, 2.3– 9.6]; P <0.001) [2]. Currently, the incidence of TLT for ACAS in the United States is 5.8% [15]. Updated meta-analysis by Mac Grory B. et al. (2020) also demonstrated the high effectiveness of TLT when treated within a “therapeutic window” of 4.5 hours [28]. Currently, there are three large studies on TLT for ACAS (THEIA (alteplase), REVISION (alteplase), TenCRAOS (tenecteplase)). Pending study results, we believe that the possibility of intravenous TLT (risk/benefit) should be discussed between the physician and the patient. The most commonly used drug for TLT is alteplase (0.9 mg/kg, 10% administered over 1 minute, rest over 59 minutes). The risk of symptomatic intracranial hemorrhage during TLT for ACAS is low.
Carrying out TLT beyond 4.5 hours requires further study (including using biomarkers of retinal viability). Emerging evidence suggests that immediate optical coherence tomography may be useful in identifying patients within the 4.5-hour window if they are unable to report the time of symptom onset [57].
Intra-arterial TLT. Administration of alteplase via superselective microcatheterization (0.60 mm microcatheter) of the ophthalmic artery ostium has the theoretical advantage of reducing the risk of intracranial and systemic hemorrhage, however, with an increased risk of arterial dissection, catheter-induced spasm, and distal embolization [58]. Therefore, intra-arterial TLT may be considered in patients with contraindications to intravenous alteplase (recent surgery, gastrointestinal bleeding, or coagulopathy).
Mechanical thrombectomy in OCSA is impossible due to the size of the arteries (the diameter of the ophthalmic artery is 1.3 mm, the diameter of the terminal part of the OCSA is 160 µm).
Conservative treatment
Several conservative approaches have been proposed (anterior chamber paracentesis, ocular massage, topical IOP-lowering agents, sublingual isosorbide dinitrate, systemic β-blockers, carboxytherapy (95% O2/5% CO2 inhalation), and paper bag breathing). The proposed rationale is modulation of intraocular pressure or dilation of retinal vessels for peripheral migration of the embolus. As a rule, a combination of two or more methods was used, but there is no evidence of the effectiveness of these methods (on the contrary, there is evidence of their negative effect). Hyperbaric oxygen therapy (HBOT) is used as a retinal tissue salvage treatment for acute CASA. Normally, >50% of oxygen enters the retina through passive diffusion from the choroid, while with HBOT this figure reaches 97% [65]. Thus, HBOT may be beneficial as a temporary measure while reperfusion therapy is administered.
Secondary prevention
The optimal approach is interdisciplinary collaboration between a neurologist, ophthalmologist and internist. The role of the ophthalmologist is to optimize residual visual acuity and its dynamic assessment; monitoring complications associated with neovascularization; maintaining the health of the contralateral eye. The role of the neurologist and therapist is to determine the cause and initiate an appropriate pharmacological strategy for secondary prevention (treatment of hypertension, dyslipidemia, diabetes, obesity, obstructive sleep apnea syndrome; smoking cessation; diet; regular physical activity; antithrombotic therapy; surgical treatment of ICA stenosis).
In patients with NIHSS ≤3, it is reasonable to use dual antiplatelet therapy for 21 days followed by long-term use of a single antiplatelet agent (usually aspirin 81 mg/day or clopidogrel 75 mg/day) [49,72]. If AF is detected, anticoagulants are indicated.
Figure 3. Treatment protocol for OCSA.