Coronary heart disease (CHD), along with cancer, is not only a medical, but also a social problem. Massive studies of the 20th century made it possible to identify risk factors for coronary artery disease. These include heredity, age, excess body weight, physical inactivity, hypertension, diabetes and male gender. Among all the risk factors, there are avoidable ones, such as smoking, and irreparable ones.
Prevention of coronary heart disease can be primary and secondary. Primary prevention of coronary heart disease refers to the prevention of the occurrence and development of risk factors for diseases in people without clinical manifestations. Secondary prevention is aimed at eliminating risk factors that, under certain conditions, can lead to exacerbation or relapse of existing ischemic heart disease.
When to start prevention of coronary artery disease
Reasons for development
diseases can be divided into three categories.
Persons included in at least one of these groups should especially carefully monitor their health
and regularly see a doctor.
Risk factors for developing coronary artery disease
- Biological: elderly and advanced age, gender of the person (men are more predisposed to ischemia).
- Biochemical and physiological: dyslipidemia (impaired fat metabolism), hypertension, obesity, diabetes mellitus and impaired glucose tolerance.
- Behavioral: smoking, addiction to alcohol, poor diet, physical inactivity, exposure to stress.
Most often, early ischemic
changes in blood vessels appear due to behavioral factors - poor nutrition, bad habits and physical inactivity (decreased physical activity).
Therefore, the earlier a set of
special preventive measures is started, the greater the likelihood of reducing the risk of serious pathology of the heart and blood vessels to a minimum.
The most reliable prevention of ischemia is a healthy lifestyle
Primary prevention of coronary artery disease
is a list of rules, the totality of which is called a healthy lifestyle. They are recommended to be followed not only by people at risk, but by any person. These are simple and effective measures to help avoid problems with the heart and blood vessels.
Secondary
called
prevention
, which is aimed at reducing the risk of
developing
complications of an existing disease. These measures should be implemented from the moment of diagnosis, regardless of age.
Particularly carefully and to the primary
, and
secondary prevention
should be applied to people over 40 years of age - as part of monitoring the condition of the cardiovascular system.
Primary prevention of IHD is carried out among people without clinical manifestations of the disease, that is, practically healthy. Main directions of primary prevention of coronary heart disease
include:
- organization of rational nutrition,
- lowering cholesterol and blood sugar levels,
- body weight control,
- normalization of blood pressure,
- the fight against smoking and physical inactivity, as well as
- organizing the correct daily routine and alternating work and rest.
That is, prevention is aimed at eliminating modifiable risk factors and is not only a personal, but also a national problem.
The basis of proper nutrition
The principle is that calories consumed correspond to calories burned. The approximate diet of a thirty-year-old mental worker should contain no more than 3000 kcal, with protein should be 10-15%, carbohydrates (mostly complex) - at least 55-60%. As you age, you need to reduce your calorie intake by approximately 100-150 kcal every 10 years.
Healthy eating as a preventive measure for coronary heart disease
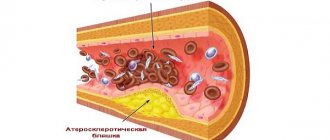
Scientists have long shown that lowering cholesterol levels
blood can lead not only to the prevention of the development of atherosclerosis and ischemic heart disease, but also to some regression of plaques already formed in the vessels.
At the initial stage, hypercholesterolemia must be combated through diet; if there is no effect, medications (statins) may be used. This is especially important for people with irreparable risk factors for developing coronary heart disease. The same goes for
normal blood glucose levels
To monitor body weight, doctors and nutritionists use an indicator called body mass index.
(BMI). This figure is obtained by dividing a person's weight in kilograms by the square of their height in meters. For example, with a height of 170 cm and a weight of 70 kg, the body mass index will be 24. Normal BMI values are in the range of 18.5-25.
Arterial hypertension is an independent risk factor for the development of coronary artery disease, therefore, at the first signs of an increase in pressure more than 140/90 mm Hg. it is necessary to contact a cardiologist to select therapy.
Smoking
- not just a bad habit. It has been established that smoking even 1 cigarette a day leads to a 2-fold increase in the risk of death from coronary heart disease. That is why so many social policy programs are aimed at combating smoking.
It is not so easy to get a young healthy man to give up, say, smoking or eating fatty foods. Not everyone thinks about the future, and IHD, which can develop in 20-30 years, is not the best motivating factor. To make it easier for the doctor to convey information about the primary prevention of coronary heart disease
to the population, special tables of the absolute risk of developing IHD have been developed. These nomograms allow us to determine the risk of developing coronary artery disease now and by age 60 years. If, according to parameters (age, gender, smoking, systolic pressure, blood cholesterol concentration), the risk of developing IHD reaches 20%, then immediate intervention and correction of risk factors is necessary.
Secondary prevention of coronary artery disease
The main areas of secondary prevention are:
- Addressing risk factors that are not necessarily the same as those considered in primary prevention.
- Drug prevention of coronary vascular spasms.
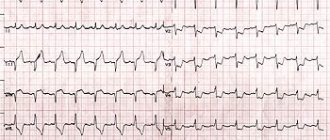
- Treatment and prevention of arrhythmias.
- Rehabilitation of patients with the help of physical training and medications.
- Surgical care for patients, if the need arises.
All of these measures are aimed at preventing repeated exacerbations of coronary artery disease, increasing the duration and quality of life, increasing working capacity and preventing sudden death of patients.
An important role is played by the patient himself, who must be an active ally of the doctor in the fight to preserve his health.
To do this, the patient is required to strictly comply with all medical recommendations, actively participate in rehabilitation plans, and timely inform the doctor about changes in his well-being. Prevention should begin in childhood
Although the first symptoms of coronary heart disease (CHD) usually appear in middle-aged and older people, atherosclerosis begins to develop in childhood. In addition, most habits, including harmful ones, leading to the emergence of risk factors for coronary artery disease, are formed already in childhood and adolescence. According to WHO, in many countries around the world children first try smoking at the age of 6-11 years. Smoking very quickly becomes a habit: by the age of 15, 40% of boys and girls already smoke, and by the age of 19 - 50%. Sample studies have shown that at the age of 13 years, 7% of boys smoke at least three cigarettes a week, at the age of 14 years - 30% at the age of 15 years. - 36% and at the age of 16 years - 41.2%, i.e. these figures practically do not differ from those given by WHO. Moreover, in recent years, there has been a trend towards an increase in the number of girls smoking throughout the world.
Eating habits that contribute to obesity and lipid metabolism disorders are also established in childhood. Moreover, it was found that the elevated level of cholesterol in the blood detected in children persists quite persistently in their subsequent years.
High blood pressure also occurs in adolescence. Of course, not all children with high blood pressure will later become persistently hypertensive, but their risk is undoubtedly higher than that of children with normal blood pressure. According to epidemiological studies, in different countries, increased blood pressure is detected in 6-8% of adolescents. Moreover, according to observational data, in 42% of children who were found to have high blood pressure at the age of 13 years, it remained elevated at the age of 18 years, i.e. these are already real candidates for hypertension.
Currently, in various countries of the world, including Russia, programs are being carried out aimed at combating risk factors for cardiovascular diseases, starting from childhood. Preliminary results show that by teaching the basics of a healthy lifestyle and promoting the cessation of bad habits, the prevalence of risk factors for cardiovascular disease can be reduced. Promotion of a healthy lifestyle should be carried out in the family, school and by teenagers themselves. The example of parents plays an important role: children of smoking parents smoke more often; children of parents leading a sedentary lifestyle are also physically inactive. Eating habits also largely depend on parents. Teenagers, especially those who have authority among their peers, can successfully promote a healthy lifestyle. Moreover, often the example of a friend and the desire to be like him have a stronger influence on the behavior of a teenager than the recommendations of parents.
At the same time, children can positively influence the habits of their parents, being promoters of a healthy lifestyle. Teenagers themselves can actively influence the bad habits of their friends, helping to get rid of them. This is one of the most effective methods of influence.
Thus, the basis of primary prevention of cardiovascular diseases is the fight against risk factors for these diseases. It's better, of course, to avoid the habits that create these risk factors, but at the same time, it's never too late to try to give them up.
If we analyze the essence of the recommended healthy lifestyle, then there is nothing in it that is very difficult to live without. To keep your heart healthy, you need to eat rationally (a diet containing moderate amounts of calories, salt, fat, cholesterol), monitor your body weight, exercise regularly, stop smoking and drinking alcohol, and regularly monitor your blood pressure. As you can see, there is nothing fundamentally new or impossible. Following these simple recommendations will help you avoid many diseases without any restrictions on your active and enjoyable lifestyle.
Primary prevention of coronary artery disease
Save your heart
The following rules will help keep your blood vessels healthy:
- Balanced diet. The diet should include daily consumption of fresh vegetables and fruits, as well as limiting the menu of meat products, table salt and glucose. You should completely avoid fatty, fried, smoked foods and baked goods - these products increase the content of low-density lipoproteins ("bad" cholesterol), and also provoke obesity, the constant companions of which are hypertension and atherosclerosis.
The number of thermally unprocessed vegetables and fruits in a healthy menu is not limited
- Enrichment of the diet with microelements, especially B vitamins, magnesium, potassium and iron. They regulate the heart rhythm
, improve
the condition
of blood vessels and myocardium, slow down the progression of
coronary artery disease
. The lack of microelements in the diet can also be compensated for with preparations containing magnesium, vitamins, etc. - Moderate consumption of caffeine-containing drinks - coffee and tea. Caffeine has effects on the body similar to those of adrenaline: it stimulates cardiac activity, increases blood pressure, accelerates the pulse and increases the risk of arrhythmia.
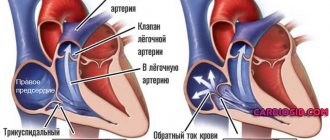
- Physical activity. Physical inactivity leads to weakened contractility hearts
and significantly increases vascular risks: the speed of blood flow in arteries and veins decreases, creating conditions for thrombus formation.
Daily morning exercises and a couple of workouts a week lasting 20-40 minutes will protect the heart
from ischemia. - Complete rest. Stress and lack of sleep deplete the body. Due to overwork and increased adrenaline and cortisol (stress hormones), normal work becomes difficult hearts
, and also increases the risk of hypertension.
- Rejection of bad habits. Smoking increases the likelihood of cardiac ischemia by 57% due to an increase in fibrinogen in the blood, a specific protein that becomes the basis for blood clots. In addition, smoking increases the level of “bad” cholesterol, leading to the development of atherosclerosis - a precursor IHD
.
Alcohol worsens the rheological properties of blood, causing thrombus formation, and also disrupts heart rhythm
and myocardial trophism. - Maintaining normal body weight. Excess weight has an extremely negative effect on the condition of both the heart and blood vessels: fat deposits in the myocardium lead to its atrophy, lipocytes “steal” oxygen from cardiac
muscles, and increased lipid levels thicken the blood and stimulate blood clots.
Secondary prevention of coronary artery disease
Patients with an established diagnosis of ischemic
heart disease must especially carefully observe measures to prevent the further
development
of the pathology and its complications - unstable angina, chronic heart failure, myocardial infarction.
A set of secondary prevention measures
- Avoiding any nervous tension or learning self-control techniques that will help reduce the risks of stress spasm of the coronary arteries.
- Therapeutic physical education (therapeutic physical education). The initial level of activity and the dynamics of its growth are determined by the doctor based on body weight, level of fitness, age and severity diseases
.
- Reception appointments medications
.
After assessing the severity condition
, the cardiologist prescribes statins (lowering low-density lipoprotein levels), antiarrhythmics, antihypertensives and blood thinners. - Surgical treatment methods in cases where the disease progresses rapidly despite the implementation of the above measures prevention
.
Risk of developing the disease
When assessing the risk of developing coronary artery disease, the following characteristics should be taken into account: age, gender, the presence of cardiovascular diseases in the patient in the past and present, family history.
During the survey, you should pay attention to such lifestyle characteristics as diet, smoking, level of physical activity, it is necessary to measure body weight, blood pressure levels, and assess the level of lipids and glucose in the blood. The risk of developing coronary artery disease is assessed based on a study of all these characteristics.
A strategy to combat risk factors is then developed together with the patient or family.
An interesting direction in the study of preventive strategies was highlighted at the Congress of Cardiologists in 2006. The possibilities of prevention and the effectiveness of this process in cardiology were made dependent on two primary groups of parameters: the formation of new relevant risk factors and the achievability of prevention goals. Thus, in Europe, the INTERHEART study was organized, which showed the relevance of new risk factors, such as the Apo-B/Apo-A-1 ratio for cases of acute myocardial infarction, hyperhomocysteinemia for atherosclerosis and hypercoagulation. Target indicators among lifestyle modification parameters were presented in an interesting way:
- to give up smoking;
- blood pressure control <140/90;
- control of blood cholesterol concentration <5 mmol/l for all and <4.5 mmol/l for patients with coronary artery disease;
- control of low-density lipoprotein cholesterol concentration <3.5 mmol/l for all and 2.5 mmol/l for patients with coronary artery disease;
- maintaining waist circumference <91 cm for men and <88 cm for women;
- achieving an optimal BMI of 20-25 kg/m2
To illustrate the second group of indicators that influence the effectiveness of measures to prevent diseases and complications, we can cite the EUROACTION study, which studies new approaches to preventive cardiology. The study includes groups of patients: those suffering from ischemic heart disease, relatives of patients with juvenile forms of ischemic heart disease; patients with a SCOR index > 5% (systemic coronary risk evaluation in 10 years) and their relatives.
EUROACTION program studies:
- main risk factors (lifestyle, smoking, nutrition, physical activity);
- other risk factors (BMI, obesity, blood pressure, cholesterol and blood glucose levels, etc.);
- possibilities and effectiveness of drug prevention of cardiovascular diseases.
The program uses a family-based approach and contains a multidisciplinary team of researchers; has a hospital observation program for patients and programs for observation by general practitioners in outpatient settings. The main purpose of the EUROACTION analysis is to determine the achievability of European prevention targets.
At the current level of knowledge, it should be noted that various clinical recommendations for the prevention of coronary artery disease differ significantly from each other in the number of people needing treatment, the number of deaths prevented, as well as the number of people who need to be treated to prevent one death. To evaluate the effectiveness of various statin therapy recommendations in the prevention of CAD, Dr. Manuel Douglas and colleagues (Institute of Clinical Quantitative Research, Toronto, Canada) compared recommendations from the Canadian, Australian, New Zealand, British, American and European Societies of Cardiology regarding management and prognosis. study participants in persons 20-74 years old. It turned out that the Australian and British recommendations are the most effective - their implementation will save more than 15,000 lives over 5 years. The New Zealand guidelines save 14,700 lives, with only 12.9% of people requiring treatment, compared with 17.3% in the Australian and UK guidelines. The number of patients who need to be treated to prevent one death for the New Zealand recommendations is 108, for the Australian and British - 139. In contrast, according to the American recommendations, twice as many people need to be treated, 24.5%, while the number of lives saved will not increase. To prevent one death, 198 people need to be treated. European and Canadian recommendations occupy an intermediate position.
Thus, preventive strategies are actively used and studied in foreign cardiological practice, which indicates the need for their study and application in domestic cardiology. It seems more reasonable to apply the above strategies in practice specifically in general medical practice and family medicine, when the ideal goals of primary prevention are still achievable and where the main observation of elements of secondary and tertiary prevention takes place.