According to WHO statistics, cardiovascular diseases are among the top three causes of death. Blood clots in blood vessels are one of the main factors in the development of ischemia of the heart muscle, as well as heart attacks and strokes. That is, increased blood clotting provokes acute diseases that lead to severe, often irreversible complications and death of the patient.
Causes of bleeding disorders
- Genetic. Sometimes the blood clotting mechanism has congenital defects caused by mutations in genes. Some mutations are inherited and lead to diseases such as hemophilia.
- Medicinal. Taking drugs that affect blood clotting (aspirin and other non-steroidal anti-inflammatory drugs, anticoagulants, fibrinolytics).
- Somatic. They occur against the background of other diseases (blood diseases, liver diseases, vitamin K deficiency, massive blood loss, etc.).
Most causes of bleeding disorders require immediate treatment. To detect them, you must first do a general blood test for blood clotting. Coagulation disorders can manifest themselves in two ways: increased and decreased blood clotting. The danger of increased blood clotting is explained by the high risk of blood clots in the vessels and the deterioration or complete cessation of blood supply to a tissue or organ. Reduced blood clotting, which can be congenital or acquired, poses a particular danger during injuries and operations.
Treatment
For treatment of this condition to be effective, the causes of the disease must be determined. It is very important to promptly identify and treat the main disorders - liver pathologies or oncological lesions.
Additional therapy methods include:
- injection of vitamin K;
- drugs to improve clotting;
- transfusion of frozen blood plasma;
- Other medications include hydroxyurea and oprelvekin, which help eliminate platelet problems.
The patient's diet should include foods high in calcium, folic acid, vikasol, and amino acids.
These include dairy products: cheese, cottage cheese, kefir. Fish and meat will also help eliminate the symptoms of pathology. It is equally important to eat leafy vegetables - green onions, spinach, cabbage.
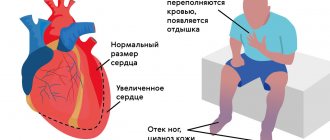
Consequences of increased blood clotting
Under these conditions, the risk of blood clots is significantly increased. Inflammation of thrombosed veins leads to thrombophlebitis, accompanied by:
- pain;
- swelling;
- redness of the skin over the vein.
Blood clots in blood vessels lead to narrowing of their lumen and damage to tissue areas due to a lack of blood supply. When blood flow through a vessel is completely stopped due to a blood clot, an area deprived of blood supply appears in the tissue, which is called an ischemic focus. In this area, cells quickly die and the normal functioning of the organ is disrupted. Irreversible damage to the brain and heart are the most dangerous consequences of thrombosis. Another insidious complication is the detachment of a blood clot. Often the diameter of the blood clot is smaller than the diameter of the vessel, so the patient is unaware of its presence for a long time. However, with injuries and concussions of the body, at the beginning of taking medications that thin the blood, as well as when getting up on your feet after a long stay in bed (for example, after surgery), the clot can break off and continue to move through the bloodstream until it clogs the lumen of the vessel somewhere. It is because of such blood clots that a formidable and very dangerous complication develops - pulmonary embolism, which can result in the death of a person if medical assistance is not provided in time. They can only be detected by carrying out certain studies, including a general blood test for blood clotting.
Diagnosis of pathology
Diagnostic procedures are performed by doctors of several specializations: neonatologist, pediatrician, geneticist and hematologist. For concomitant pathologies, consultation with a gastroenterologist, orthopedist, otolaryngologist and neurologist may be required.
At-risk couples should visit a doctor before conceiving a child. Molecular genetic research of biomaterials from future parents will allow us to take into account the risk of having a child with hemophilia. After conception, prenatal screenings may be performed. Their results will confirm or refute the fact that the child inherited hemophilia.
Neonatal tests performed in the first days of a baby’s life are no less effective. A coagulogram provides the neonatologist with comprehensive information about the production of coagulation factors by the newborn’s body.
In case of hemarthrosis, the child is prescribed an X-ray examination of the joints. Ultrasound diagnostics is performed when signs of internal bleeding and retroperitoneal hematomas are detected.
Consequences of decreased blood clotting
With this condition, a person has an increased risk of bleeding. One of the common consequences is gastrointestinal bleeding against the background of an existing ulcer. Blood loss in such conditions due to the duration of bleeding can be very serious. Low blood clotting increases the risk of internal bleeding, which is often noticed too late. Therefore, it is necessary to conduct a general blood test for blood clotting before any operation, as well as during treatment with drugs that have a blood thinning effect (anticoagulants, antiplatelet agents, fibrinolytics, etc.).
2. Symptoms of the disease
Symptoms of hemophilia may include:
- Bleeding in a joint or muscle area that causes pain and swelling;
- Abnormal bleeding after wounds or surgery;
- Bruising;
- Frequent nosebleeds;
- Blood in the urine;
- Bleeding after dental surgery.
Some people with mild hemophilia may not experience all of these symptoms, especially as the person gets older. However, in infants it is usually possible to diagnose hemophilia based on some signs. So, signs of hemophilia in infancy may be an unusual reaction to the most common vaccination - intramuscular bleeding and serious bruising. Or, for example, bleeding that begins after cutting the umbilical cord and does not stop for a long time (but this happens very rarely).
Visit our Therapy page
Who needs to determine blood clotting?
To reduce the risk of developing vascular accidents and unexpected bleeding, it is necessary to periodically monitor the state of the blood coagulation system using a laboratory method. This is especially important for:
- people over 40 years old;
- women during and after menopause;
- women during pregnancy;
- people who regularly take blood thinners (aspirin);
- patients suffering from varicose veins;
- those preparing for surgery, etc.
The doctor must prescribe blood clotting tests if hemophilia is suspected (usually this disease is detected in early childhood and young adulthood) or when treating an existing thrombosis with fibrinolytic therapy and anticoagulants.
Reasons for the development of pathology
The mechanism and type of inheritance of hemophilia have been studied in sufficient detail. Genes that provoke insufficient production of blood clotting factors are linked to the X chromosome. The pathology is inherited recessively through the female line. Hereditary pathology occurs exclusively in boys.
The sons of a healthy man and a woman who is a carrier of the pathological gene are equally likely to be born without signs of hemophilia or with them. A man suffering from bleeding disorders will be able to conceive healthy children with a woman who is not a carrier of the altered gene.
Medicine knows of isolated cases of hemophilia in women. Their mothers were carriers of a mutated gene, and their fathers suffered from insufficient production of blood clotting factors. The cause of hemophilia in such cases is a combination of recessive and dominant genes.
How to test your blood clotting
Blood coagulation is a complex process consisting of several different parts and stages. Therefore, a blood clotting test should help evaluate the performance of each component link. Blood clotting occurs through the interaction of many factors along a chain. The results of a general blood test for blood clotting help determine which of the factors is impaired, which facilitates further diagnosis and choice of treatment. For example, an analysis to evaluate APTT (Activated partial thromboplastin time) helps to identify a violation of the “intrinsic” coagulation pathway and determine the tendency to bleeding. And prothrombin time allows you to evaluate the “external” pathway of blood coagulation, detect liver dysfunction and vitamin K deficiency. Another important indicator that greatly helps doctors when planning operations and assessing the risk of thrombosis (including during pregnancy) is a blood test to D-dimer. It allows you to:
- determine the risk level of acute and severe cardiovascular conditions;
- predict the further course of thrombosis;
- monitor the results of treatment over time.
Conducting a general blood clotting test is an important study that helps to significantly reduce the risk of unexpected complications and mortality after illness, surgery, or childbirth. The analysis data gives the doctor the opportunity to expect objective results from the upcoming treatment and control it, and the patient a chance to protect himself from the undesirable consequences of blood clotting disorders.
How quickly does hemocoagulation occur?
With normal coagulation, the process begins almost immediately after damage to the vessel. The approximate clotting time is 5-7 minutes. During this time, the blood clot should normally form completely. There is a disease, namely hemophilia, in which hemocoagulation does not occur. In addition, it worsens in the cold, as well as from exposure to hirudin, heparin, fibrinolysin, sodium citrate and potassium.
The process of hemostasis protects the body from blood loss due to damage to tissues and blood vessels
Clotting phases
Visually, the process of blood coagulation can be represented as a proenzyme-enzyme cascade. At the same time, its elements are in an active state. For detailed consideration, coagulation processes can be divided into three stages. Main phases:
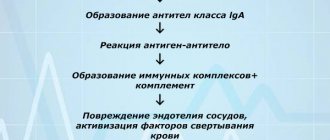
- Activation. It is represented by a complex of reactions that provoke the formation of prothrombinase. It ends with the transition of prothrombin to thrombin.
- Coagulation. It involves the formation of fibrin from fibrinogen.
- Retraction. Consists in the formation of a dense fibrin clot.
The biochemical coagulation chain is a reaction of soluble proteins that polymerize into a network. Individual processes are represented by cascade chains that retain their physical meaning. Auxiliary reactions provide a regulatory function, promoting the conversion of fibrinogen into fibrin at the required moment.
Attention! An important component of blood involved in clotting is calcium salt. If it is removed from the biological fluid, the process will not proceed.
Components and substances involved in the process
The process of thrombus formation is complex and specific. To ensure it, a coordinated interaction of proteins and enzymes found in plasma, tissues and platelets themselves is necessary. When interpreting the analysis, the concentration of components in plasma is indicated by Roman numerals. Arabic is used only to characterize platelets.
The coagulation system prevents bleeding. It involves individual components contained in the liquid part of the plasma. There are 12 of them. If there is no damage to blood vessels and capillaries, they are passive. After an injury, a continuous chain of reactions is launched due to the activation of one enzyme. Next there will be a series of transformations.