- Types of angiopathy
- Hypertensive angiopathy
- Hypotonic angiopathy
- Angiopathy of dystonic type
- Diabetic retinal angiopathy
- Traumatic angiopathy
- Angiopathy of mixed type
- Angiopathy with myopia
- 1st degree of angiopathy initial
- 2nd degree of angiopathy moderate
- 3rd degree of angiopathy, the last
- Treatment of angiopathy with medications
- Physiotherapy
- Surgical intervention
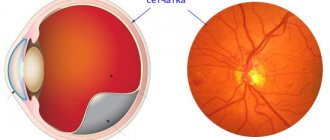
Retinal angiopathy is a specific change in the vessels of the retina, which is not an independent disease. The changes usually affect both eyes at once.
Types of angiopathy
Fundamentally, angiopathy can be divided into two groups: local damage to the retinal vessels and systemic.
In the first case, angiopathy is characterized by vascular damage at the local level (that is, at the level of the eye) - for example, changes in blood vessels with myopia.
In the second case, angiopathy reflects changes in the whole organism. Perhaps this is the most interesting and important group. Based on the condition of the blood vessels, diabetes mellitus, hypertension, atherosclerosis, systemic diseases, vascular pathology of the head and neck, even in some cases heart rhythm disturbances, etc. can be identified earlier than the therapist. An examination by an ophthalmologist is mandatory if a person has cardiac pathology, diabetes mellitus, hypertension and atherosclerosis.
Hypertensive
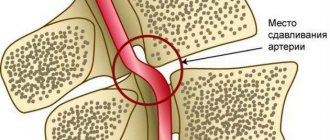
Due to high blood pressure, the inner walls of blood vessels (intima) are damaged. These special microdamages contribute to the development of hardening of the arteries, which disrupts the metabolism of the retina. The veins become congested, the outflow of blood from the retina becomes difficult, which leads to the development of oxidative stress. Dense arteries begin to compress the veins, creating favorable conditions for the formation of blood clots.
Hypotonic
Develops due to low pressure in the blood vessels. Perfusion decreases and ischemia develops.
Dystonic type
Vascular spasms significantly worsen and provoke the formation of dystrophy and retinal tears, which can lead to retinal detachment.
Diabetic
An increased level of glucose in the blood provokes metabolic damage to the vessel wall, especially in the microvasculature, which in turn incredibly aggressively disrupts metabolic processes in the retina.
Traumatic
Due to injuries to the skull, cervical spine, or eyeballs, increased pressure or disruption of blood flow may occur due to compression of the vessels leading to the eyeballs. Post-concussion paralysis of the arterial muscles develops.
Mixed type
Symptoms of several forms of angiopathy are layered on top of each other, the disease proceeds with severe symptoms and quickly progresses to complex stages.
For myopia
The arteries are usually narrow and their course is straight. In conditions of a stretched eyeball, the arteries do not reach the periphery, which leads to retinal ischemia and the development of dystrophies. This, in turn, threatens retinal detachment.
What happens to the retina?
During an ophthalmological examination, hypotonic retinal angiopathy has no clear signs. The arterial branches of the vessels are clearly visualized down to the smallest branches. However, upon examination, their pallor and opacity are revealed. There is practically no double contour; due to a decrease in the tone of the vascular wall, the vessels become tortuous.
It is known that the diameter of the arteries is normally larger than the diameter of the veins, but with hypotensive angiopathy their caliber becomes the same. The veins are filled with blood and their pulsation is detected. Due to prolonged standing of blood, tissue swelling develops, which creates conditions for thrombus formation.
As a rule, changes in the retina are dystrophies, small opacities along the main vessels, and vein thrombosis. But, in the case of prolonged hypotension, the opposite effect often occurs - hypertensive angiopathy develops due to deposits of lipids and calcium in dilated vessels. This leads to a loss of elasticity of the vascular wall, which loses the ability to change diameter.
Symptoms of retinal angiopathy
A person cannot identify angiopathy on his own. In advanced cases, complaints of decreased vision and optical phenomena may appear.
1st degree (initial)
- the retinal arteries narrow;
- retinal veins dilate;
- unevenness in the size and width of the vessels is visible;
- excessive tortuosity of blood vessels appears;
- with prolonged tension, pain, pain and pulsation occur in the eyes.
2nd degree (moderate)
- tortuosity and differences in vessel sizes increase;
- the vessels become similar in color and structure to thin copper wire, and with further progression of the disease, they turn gray and pale;
- hemorrhages and blood clots are observed;
- the fundus of the eye turns pale and takes on a waxy tint;
- the field of view changes;
- There may be a disturbance in light sensitivity;
- vision becomes foggy, sharpness is lost;
- myopia appears.
3rd degree (last)
- the optic nerve and inner lining of the eye swell;
- hemorrhages are noticeable;
- white lesions are visible on the retina;
- vision decreases greatly (complete blindness may occur).
Diagnosis of retinal vasospasm
Anamnestic data, the results of a visual examination in combination with additional diagnostic methods allow the ophthalmologist to establish vasospasm of the retinal vessels as a diagnosis. The list of studies within the framework of pathology detection includes:
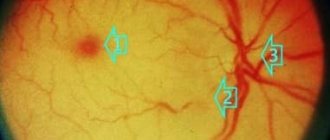
- Ophthalmoscopy. After examining the fundus of the eye, the doctor visually determines a sharp narrowing of the veins in the retina. The vessels are full of blood, but a somewhat swollen, pale pink optic disc is visible. The foveal reflex, like the macular reflex, is not diagnosed during vasospasm.
- OCT. During scanning of the central part of the retina, thickening is visible. In this case, the foveal recess is greatly smoothed, and retinal reactivity is reduced, while the shape of the curve is atypically straight.
- Non-contact tonometry method. During an attack, the specialist observes a slight increase in IOP (intraocular pressure), and after its relief, a normalization of ophthalmotonus.
- Angiography. The ophthalmologist visualizes the changes taking place in the retinal vessels. Diagnosis occurs as part of studying the characteristics of fluorescein circulation. During vasospasm, the internal blood-retinal barrier for contrast remains impenetrable.
Reasons for the development of the disease
Angiopathy develops against the background of vascular pathologies, so the reasons for the development of the disease are the risks that provoke vascular diseases:
- age from 30 years,
- smoking,
- alcoholism,
- pathological conditions of pregnancy,
- overweight,
- systematic intoxication (when working in toxic industries, during treatment),
- congenital disorders,
- diabetes,
- atherosclerosis,
- osteochondrosis and scoliosis,
- inflammation of the vascular wall,
- blood diseases and so on.
About arterial hypotension
It is worth understanding that arterial hypotension is not an independent disease; it is only a symptom that indicates an insufficiently high level of pressure in the vascular system.
In some cases, low blood pressure is a normal variant that does not require medication correction at all. For example, some people always have low blood pressure, which is their individual characteristic. Hypotension in athletes is an adaptive reaction in response to prolonged physical activity. People living in high mountains also have lower blood pressure numbers. In this case, their indicators are a compensatory reaction to lower atmospheric pressure.
But there are also pathological conditions that cause a decrease in blood pressure:
- Primary arterial hypotension. It occurs with neurocirculatory dystonia due to dysfunction of the autonomic nervous system with a predominance of its parasympathetic part. Experts call it hypotension.
- Secondary arterial hypotension. A symptomatic condition caused by a number of pathologies of the cardiovascular, nervous or endocrine systems. In addition, it can develop against the background of anemia, chronic intoxication, prolonged infectious lesions, irrational treatment tactics (large doses of antihypertensive or antihistamines, antidepressants).
Diagnosis of angiopathy
The disease is easy to detect with a standard fundus examination. During retinal imaging, you can identify:
- narrowing or dilation of arteries and veins,
- thickening of the vascular wall with the formation of pathological reflexes,
- tortuosity or straightening of the course of blood vessels,
- hemorrhages,
- areas of compression of arteries, veins, etc.
Important to remember! An annual examination by an ophthalmologist is mandatory if a person has hypertension, cardiac pathology, diabetes and atherosclerosis. In our clinic, it is possible to conduct not only examinations of the fundus of the eye with a description and conclusion of a specialist, but also to observe the dynamics of changes yourself using photographic recording of the condition of the retinal vessels (FundusFoto).
In some cases, additional examination is prescribed:
- Vascular ultrasound – determination of blood flow speed and the condition of the vascular walls;
- X-ray with the introduction of contrast - determination of vascular patency;
- MRI – assessment of the condition of eye tissues;
- visometry – determination of visual impairment;
- ophthalmoscopy - identification of the affected area of the retina;
- tonometry - determination of intraocular pressure.
The eyes are the only place on the human body where you can see blood vessels on the surface. This feature is successfully used in diagnostics. Based on the condition of the eye vessels, the following can be identified before the therapist:
- diabetes,
- hypertension,
- atherosclerosis,
- systemic diseases,
- pathology of the blood vessels of the head and neck,
- heart rhythm disturbance (in some cases).
Diagnosing retinal vascular angiopathy and monitoring its development can help in adequately assessing the course and success of treatment of the general disease. For example, the adequacy of the selection of antihypertensive therapy for hypertension is assessed by the degree of leveling of signs of hypertensive angiopathy.
Expert opinion
Klyuganov Vitaly Sergeevich
Qualified ophthalmologist
Work experience: 12 years
Retinal vascular angiopathy is not an independent disease, but only one of the manifestations of certain pathological conditions complicated by damage to the blood vessels of the retina or the entire body.
Based on the condition of the blood vessels, diabetes mellitus, hypertension, atherosclerosis, systemic diseases, vascular pathology of the head and neck, heart rhythm disturbances, etc. can be identified earlier than the therapist. An examination by an ophthalmologist is mandatory if a person has cardiac pathology, diabetes mellitus, hypertension and atherosclerosis.
It is not difficult for an experienced specialist to detect the disease. In the process of visualization of the retina, one can identify narrowing or expansion of arteries and veins, thickening of the vascular wall with the formation of pathological reflexes, tortuosity and straightening of the course of blood vessels, hemorrhages, areas of compression of veins, and much more. Taking into account the stage of angiopathy determined by the ophthalmologist, the therapist, endocrinologist, and cardiologist can assess the severity of the underlying disease.
Therefore, examination of the fundus with a wide pupil is mandatory during a full ophthalmological examination.
Retinal angiopathy during pregnancy
The causes of retinal angiopathy during pregnancy include:
- increase in blood volume in the body;
- presence of autoimmune diseases;
- development of gestational diabetes mellitus;
- chronically high or low blood pressure.
- gestational diabetes
- toxicosis
- bleeding disorder
Angiopathy in pregnant women most often goes away on its own and therefore does not require treatment. However, if the patient suffered from pathology before bearing the child, then the disease can progress and lead to complications: thrombosis, retinal detachment and hemorrhage. In severe cases, the disease can provoke termination of pregnancy.
When retinal angiopathy appears, treatment of concomitant diseases that provoked the development of pathology will be required. The woman is recommended to be monitored by a therapist and endocrinologist.
Most often, medications are prescribed that improve blood circulation and reduce the permeability of vascular walls. To normalize blood flow in the eyeball, special drops are used. In case of severe retinal angiopathy of both eyes, additional physiotherapeutic procedures may be prescribed.
Retinal angiopathy in a child
The development of angiopathy in a child is usually associated with the following factors:
- Increased intracranial pressure
- Deviation in the innervation of blood vessels, leading to a change in their tone
- Traumatic brain injuries
- Kidney diseases
- Diabetes mellitus type 1
- Autoimmune diseases
- Scoliosis
- Congenital malformations of the cardiovascular system
- Systemic pathologies of the hematopoietic organs
- Oxygen starvation of the fetus in late gestation or during labor
The disease in childhood can cause serious complications. Thus, retinal angiopathy in newborns often becomes chronic and leads to irreparable organic changes in the circulatory structure of the eye. With the development of pathology in a teenager (the so-called Eales disease), the vitreous body of the eye is replaced with fibrous tissue, which often provokes glaucoma and cataracts.
Treatment of the disease most often consists of prescribing medications that affect blood circulation and prevent platelets from sticking together. However, such treatment of retinal vascular angiopathy is prescribed only to children of preschool and school age. Newborns require regular monitoring by a doctor, since sometimes pathology occurs during a difficult birth and does not require additional therapy.
In case of severe angiopathy and its spread to both eyes, surgery may be performed to remove fibrous tissue.
Types of treatment
With angiopathy, the underlying disease must first be treated. Thus, for the treatment of retinal angiopathy of the hypertensive type, medications are prescribed to lower blood pressure; for diabetic angiopathy, diet and drugs that lower sugar levels are prescribed.
Treatment with medications
To eliminate the symptoms of angiopathy, relieve the disease and restore the ocular vessels, drug treatment is effectively used:
- Trental, Arbiflex improve blood circulation;
- Vitamins B, C, E and A, nicotinic acid normalize microcirculation;
- Calcium dobesilate, Xanthiol nicotinate, Ginkgo Biloba strengthen the walls of blood vessels;
- Cocarboxylase and ATP activate metabolism in tissues;
- Trombonet, Ticlodipine, Magnicor, Dipyridamole prevent the formation of blood clots.
Taking medication lasts about two weeks.
In case of stabilization of angiopathy, which is caused by an incurable or chronic disease, treatment is carried out every six months in courses of 2-3 weeks.
It is important to remember that treatment must be prescribed by a doctor. Self-administration of medications may do more harm than good.
Physiotherapy
In combination with other treatment methods, the following are used:
- acupuncture,
- magnetotherapy,
- laser irradiation.
Surgical intervention
To prevent vision loss at a late stage of the disease, laser coagulation of blood vessels is performed.
The operation takes 20 minutes and is performed under local anesthesia.
Table of contents:
What is retinal angiopathy Classification Causes of manifestation Symptoms and diagnosis Methods of treatment of retinal angiopathy Cost of treatment at the Santa Clinic
Retinal angiopathy is a collective term denoting the manifestation of pathologies affecting the blood vessels of the retina. Changes in the ocular vessels are caused by a violation of nervous regulation. The pathological process is accompanied by hemorrhages in the retina, the formation of microaneurysms, atherosclerotic plaques, and thrombosis. Treatment of retinal angiopathy at the Santa Clinic in Chelyabinsk is carried out using medication or laser therapy.