Retinal angiospasm is an emergency condition in ophthalmology, which is characterized by disruption of metabolic processes in cells due to cessation of blood flow. Like any emergency form of the disease, vasospasm requires surgical intervention by a specialist. Observation of people who have suffered this condition allows us to draw the following conclusions:
- disruption of the cardiovascular system is one of the causes of vasospasm, as evidenced by 91.2% of cases;
- in particular, atherosclerosis and arterial hypertension lead to retinal vasospasm, 60% of cases prove this connection;
- in 25-30% of cases it is not possible to determine what caused the vasospasm;
- this emergency condition usually occurs in people over 40 years of age;
- the number of sick men is twice as high as women.
What are the causes of this condition?
The causes of retinal circulatory disorders have not been fully elucidated. In childhood, the reduction of the middle layer of blood vessels occurs due to the development of the peripheral nervous system. In adults, the causes of the disease include the following:
- Hypertension leads to a sharp reflex contraction of blood vessels, this also applies to the eye area.
- Diabetes. This disease causes diabetic retinopathy. The latter condition is accompanied by episodes of vasospasm.
- Atherosclerosis leads to increased blood pressure and impaired blood flow through the vascular system of organs and tissues.
- Bad habits. Smoking and alcohol abuse can lead to retinal vasospasm, since nicotine and ethyl alcohol are substances that lead to vasoconstriction, disrupting the blood supply to the retina.
- Intoxication is often observed in people who have been in unhealthy conditions for a long time. In particular, compounds of carbon disulfide and lead increase the tension of the vascular wall, which changes the diameter of the lumen of blood vessels, leading to impaired blood flow.
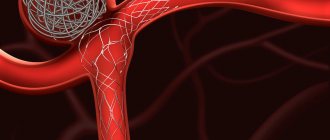
The mechanism of the onset of the disease can be described as follows: an increased concentration of calcium ions and a decrease in potassium and sodium ions lead to changes in the smooth muscle layer. As a result, the lumen of the vessels narrows, slowing down blood flow. Long-term intoxication leads to an increase in the tone of the sympathetic nervous system, which leads to vasospasm. Observations of insulin-dependent patients indicate an increase in the degree of rigidity of their vascular walls. This fact also leads to retinal vasospasm.
How the destructive process is formed
As a result of deviations in the transport of electrolytes in the intracerebral vessels, a change in the alternation of time allocated to the phases of contraction of the muscular membrane with the phase of its relaxation is formed.
The result is a significant increase in the duration and force of compression of the arterioles - cerebral ischemia. Local blood flow in the brain structures either slows down significantly and the tissues do not receive enough nutrients and oxygen, or stops altogether - if the lumen of the vessel is completely blocked, for example, in response to a rupture of a cerebral aneurysm.
In such a situation, it is not recommended to delay consultations with specialized specialists and prescribing treatment measures.
Symptoms
Retinal vasospasm typically affects both eyes, and in rare cases, only one. Characteristic complaints of patients are blurred vision and the appearance of flickering dots before the eyes. If vasospasm is short-term, the symptoms go away. Such a spasm may also be accompanied by a distortion of visual perception, similar to meta- and photomorphopsia. Some patients complain of discomfort in the orbital area of the affected organ of vision. During the spasm, the patient may experience headache and dizziness, pulsation in the temples. After the attack, the general condition returns to normal, visual function is restored. If the resulting vasospasm is prolonged, the consequence may be irreversible loss of visual acuity.
Main causes and predisposing factors
Angiospasm of cerebral vessels can be provoked by the simplest everyday situations, for example, intellectual or psycho-emotional overload, lack of sleep, as well as somatic pathologies that a person has.
However, vascular spasms can also cause more serious reasons:
- VSD;
- dystrophic lesions of spinal structures;
- tumor processes in the brain area;
- diseases of the cardiovascular system;
- impaired renal function;
- dystrophic changes in the myocytes of the cerebral vessels themselves;
- trauma to the skull;
- atherosclerotic lesion;
- diabetes;
- vasculitis.
Spasm of blood vessels in the head can also be caused by the following factors:
- excessive passion for strong drinks, for example, coffee;
- abuse of tobacco and alcohol products;
- chronic stressful situations;
- daily lack of oxygen - work in a stuffy room;
- negative state of the environment;
- chronic lack of sleep;
- dehydration;
- intellectual overload;
- negative hereditary predisposition.
After a thorough history taking, the specialist will identify predisposing factors and possible causes of the formed cerebral vasospasm. In the future, diagnostic procedures will confirm them.
Complications
Prolonged spasm can lead not only to a decrease in visual acuity, but also to its complete loss. The frequency of attacks causes severe discomfort and disability due to the fact that patients lack the ability to anticipate the period of development of the next fragment. The progressive form of the disease entails an increase in intraocular pressure. Over time, the patient develops secondary ophthalmopyrtension and develops ocular migraine. Rapid attacks are tolerated without complications.
Symptoms of vasospasm of cerebral vessels
Previously, the disease occurred only in elderly patients. In recent years, pathology has become “younger”. It is facilitated by the unfavorable environmental component that prevails in large cities and industrial zones, and the presence of toxic elements in the air. The latter penetrate the respiratory system and are transported directly to the brain, having a negative effect on the blood vessels.
Angiospasm is a fairly powerful and long-term compression of blood vessels. Spasm occurs due to incorrect blood circulation and supply of nutrients. This disease requires immediate treatment, since untimely assistance contributes to the development of complications, such as stroke.
You should consult a doctor if you have the following symptoms:
- Painful sensations in the occipital and temporal region;
- Frequent dizziness;
- High pressure;
- Tinnitus that occurs when a person is in a calm or active state;
- Loss of coordination, speech impairment.
Diagnostics
The disease is diagnosed based on medical history and examination; in some cases, additional diagnostic methods are used. During vasospasm, such phenomena as overflow of blood vessels and swelling of the conjunctiva are present; after the end of the attack, changes in the anterior area of the eyes are absent upon visual examination.
When diagnosing retinal vasospasm, the following methods are used:
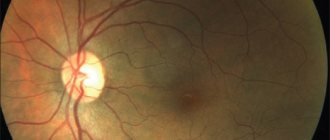
— Ophthalmoscopy. A sharply narrowed central artery and its branches of small diameter are visible upon examination. Venous arteries are filled with blood. There is swelling of the optic nerve and its pale pink color.
— Non-contact tonometry. Diagnosis by this method is based on the presence of increased intraocular pressure during vasospasm. After the symptoms disappear, the indicator returns to normal. If this phenomenon is not observed, it is necessary to refer to electronic tonography of the eye.
— Antiography of the retina. Provides an opportunity to examine the dynamics in the retinal vessels using fluorescein circulation analysis. In case of disease, the blood-retinal barrier does not allow contrast to pass through.
— Optical coherence tomography of the retina. The scan reveals a sharp enlargement of the macula (macula). The foveal fossa is leveled, the retinal reaction is reduced. The curve has an atypical straight appearance.
Features of the clinical picture
The severity of the symptoms of cerebral vasospasm will directly depend on the diameter of the affected vessels, their location and the duration of ischemia itself.
The main sign of pathological narrowing of cerebral vessels is intense headache - starting in one area of the brain, it often spreads over large areas. It can manifest itself in the form of heaviness, a feeling of being squeezed by a hoop in the head.
Additional symptoms that indicate cerebral vasospasm:
- possible irradiation of pain impulses to the neck, forehead, eyes;
- repeated increase in discomfort if the victim lies on his stomach;
- intense dizziness, nausea;
- when coughing and sneezing, symptoms worsen;
- deterioration of memory parameters;
- excessively rapid fatigue;
- decreased performance;
- flashing of flies, zigzags before the eyes;
- the presence of increased sweating;
- less often – pale skin discoloration, changes in pulse parameters;
- numbness and tingling in the temple area.
In some cases, the above symptoms preceded a vascular accident - a stroke or rupture of an aneurysm. Patients complained of acute hearing and vision disorders, difficulty with motor and speech activities.
The condition worsened until loss of consciousness, convulsions, and the presence of various paresis and paralysis.
Treatment
Etiotropic treatment has not been developed. Pathogenetic therapy is aimed at dilating spasmodic vessels to restore retinal blood flow in the ischemic area. It is extremely important to stop the symptoms of vasospasm in a timely manner, since prolonged disruption of microcirculation entails complete or partial loss of vision. For this reason, immediately after examining the fundus, infusions of plasma substitutes and antispasmodics are prescribed. The next stage of treatment is performing electrophoresis with vasodilators (drotaverine) and peripheral vasodilators (bendazole).
In order to reduce intraocular pressure, saluretics and carbonic anhydrase inhibitors are used. If there is no effect, an irrigation system is installed in the retrobulbar space. Instillation of solutions of beta-adrenergic receptor blockers (timolol, pilocarpine hydrochloride) is indicated. If accompanied by an increase in systemic blood pressure, drugs are administered intramuscularly. In order to stimulate the regeneration of the receptor apparatus, peptide bioregulators are used. If the pathology is severe, retrobulbar administration of M-anticholinergics (atropine) is additionally indicated.
Diagnostic methods
To most accurately identify abnormalities in the activity of cerebral vessels, a specialist will carry out diagnostic procedures:
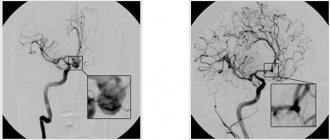
- duplex scanning of brachycephalic and intracranial arteries - allows for a comprehensive examination of the structure of the vessels, the speed of blood flow in them, as well as the presence of atherosclerotic and thrombotic deposits;
- MRI - the most accurate diagnosis;
- radiography with contrast if it is not possible to perform an MRI.
The full amount of information obtained after the above diagnostic procedures allows the specialist to make an adequate diagnosis.
Forecast and preventive measures
The prognosis for vasospasm is influenced by the nature of the attack. A short-term narrowing of the small branches of the central nervous system of the eyeball passes without a trace. Vasospastic reactions lasting 15 minutes or more, when irreversible changes in the retina occur, are considered unfavorable in terms of prognosis. Specific preventive measures are currently unknown. Nonspecific prevention consists of monitoring blood pressure and blood glucose levels, taking statins for atherosclerosis, and using personal protective equipment when working with pesticides in production conditions.
Providing quick help to yourself
A full treatment course should only be prescribed by a neurologist. If there is a deterioration in health caused specifically by cerebral vasospasm, the following measures can be taken at home:
- wash with cool distilled water;
- lie down in a darkened room, place an orthopedic pillow under your head;
- drink 25-30 drops of valerian;
- if there are no contraindications, take an analgesic or antispasmodic tablet;
- conduct a self-massage session;
- Drink slowly in small sips of warmed water with a drop of honey.
If you cannot cope with the attack on your own, then it is not recommended to delay consultation with a specialist.
Consequences of cerebral vasospasm and its prevention
If you do not seek medical help in a timely manner, a negative condition can cause quite serious consequences:
- severe cerebral ischemia – high risk of heart attacks and strokes;
- delayed intellectual development in children;
- complete blindness and deafness in adult patients;
- aneurysm rupture;
- various paresis and paralysis;
- persistent attacks of severe migraine.
To avoid the above consequences, experts recommend adhering to the following rules:
- diet correction - avoidance of fatty, heavy, fried foods;
- get rid of existing bad habits;
- avoid chronic stressful situations;
- visit fitness centers and gyms more often;
- eliminate somatic pathologies in a timely manner.
Treatment of cerebral vasospasm, as well as its prevention, is impossible without the desire for a healthy lifestyle - eat right, avoid physical inactivity, get proper rest at night, and adjust your work and rest schedule.