An ophthalmological abnormality, known as hypertensive retinal angiopathy, often leads to a systematic and significant decrease in visual acuity. Despite the presence of complications, this pathology is not an independent disease. This type of angiopathy refers to the consequences of diseases of the cardiovascular system that occur against the background of a stable increase in blood pressure, that is, hypertension.
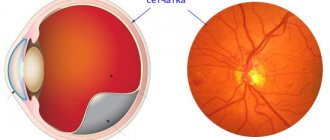
Essentially, retinal angiopathy of the hypertensive type is a complex change in the blood vessels in the fundus: arterioles narrow, and venules and veins, on the contrary, expand and become more tortuous. As a result of this process, the retina does not receive enough nutrients, swells, and pinpoint hemorrhages appear on it. Without timely detection and correction, the disease ends in widespread atrophy or retinal detachment, accompanied by loss of vision.
Causes of diabetic microangiopathy
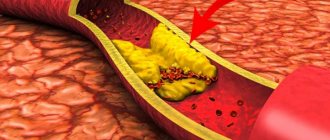
As the disease progresses, the inner membrane of the artery thickens and atherosclerotic plaques form on it. Further hardening of the artery and necrosis lead to the formation of blood clots, which leads to impaired circulation in certain places.
The development of diabetic microangiopathy in diabetes mellitus is promoted by obesity, hyperglycemia, increased blood clotting, systemic inflammation and arterial hypertension. Smoking and occupational intoxication also increase the risk of developing atherosclerosis.
Diagnosis of retinal angiopathy
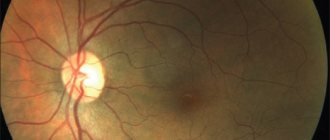
After examination and history taking, patients with suspected hypertensive retinopathy must undergo the following ophthalmological examinations:
- Ophthalmoscopy with a dilated pupil for a detailed examination of the fundus;
- Ultrasound of the internal structures of the eye (A and B – scanning) with opacity of the internal ocular media;
- Electrophysiological study;
- Fluorescein angiography;
- OCT - optical coherence tomography of the retina.
To confirm the diagnosis, it is necessary to carry out a differential diagnosis with diabetic retinopathy, anemia, autoimmune diseases, and retinal vein occlusion.
Classification of microangiopathy
At the first stage of compensation of peripheral blood circulation, stiffness of movements occurs, especially in the morning, frequent fatigue, sweating of the feet and hands, and variable lameness.
The second stage of subcompensation is manifested by an acute perception of cold and a feeling of numbness in the feet, changes in the nail plates and pale skin also appear. There is hair loss in the lower leg area. Also at the second stage, variable claudication and regional systolic pressure may be observed.
The third stage is characterized by joint pain and muscle cramps, dry skin and plantar ischemia. There is hypostatic swelling of the feet and legs, poor mobility of the foot joints, and necrotic ulcers appear on the fingers.
The fourth stage is manifested by gangrene on the fingers and feet, the appearance of large necrotic areas of tissue on the lower leg.
In patients with diabetes mellitus, changes in the somatic nervous system are often detected, and already in the early stages changes in varying degrees of severity are possible.
With diabetic microangiopathy, there are often complaints of increased fatigue when walking, an acute perception of cold - paresthesia in the form of a burning sensation, a feeling of numbness in the legs and lower legs. Such symptoms often occur in diabetes mellitus during the period of decompensation during physical activity.
Paresthesias also appear at rest; they signal the development of organic vascular damage. When paresthesia appears in a certain area of the foot or leg and accompanying symptoms and pain, one can judge the degree of vascular changes.
Also, the area of localization and the nature of the pain can characterize the degree of vascular damage and the involvement of neighboring nerves.
Partial, mild pain in the area of the feet or legs in the absence of trophic disorders may indicate an initial angiospastic stage. Pronounced pain symptoms in the legs during prolonged walking or hypothermia, or with trophic disorders may indicate organic lesions and the initial stage of obliteration. Ischemic pain also indicates obliteration of areas of blood vessels; such pain is constant and stops only when the limbs warm up.
In diabetes mellitus, calf cramps are also common and occur not only when walking. Quite often, cramps appear at night due to increased excretion of potassium in the urine. In this situation, potassium salts are taken and the convulsions stop in a short time.
Clinical studies help determine the degree of trophic disorders and pulse changes. In the initial stage, characteristic signs of trophic disorders may not be observed. The earliest signs of diabetic microangiopathy are changes in the color and temperature of the skin, which becomes white and some areas are cold to the touch. With the appearance of organic changes in blood vessels, a pronounced pallor of the skin around the fingers and feet, with a bluish tint, is observed. Next, trophic changes begin to appear, the skin loses its former elasticity, becomes dry and flabby, and peeling of the skin begins. Hair on the lower extremities also begins to fall out and nail growth slows down significantly. The nail plate becomes deformed and becomes thick and crumbly.
Rapidly progressing vascular disease of the lower extremities can probably result in the development of ulcers and gangrene. The development and course of gangrene may differ and are determined by the form of vascular lesions.
Here are several types of gangrene development:
- atherosclerotic;
- complicating the development of diabetic microangiopathy;
- appeared with a combination of different vascular lesions;
- developing with obliterating endarteritis;
- developing during a purulent inflammatory process in patients with diabetes mellitus who do not suffer from vascular damage.
Such development can occur with low tissue resistance. Diabetic gangrene is divided into dry and wet types. The dry type occurs spontaneously and is accompanied by a hemorrhagic blister on the finger, formed due to mechanical or thermal injury. Swelling appears and tissue nutrition is disrupted. The onset of gangrene may lie in the area of callus or keratinization, which also reduces blood circulation in tissues and compression of adjacent small vessels occurs.
Wet gangrene will most often develop with obliterating atherosclerosis and endarteritis.
Stages of hypertensive retinopathy
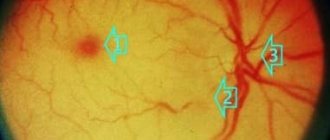
In the development of the process of hypertensive retinopathy, experts distinguish four stages:
- Hypertensive angiopathy, the first stage with reversible functional changes that affect only the retinal vessels.
- The second stage is hypertensive angiosclerosis, when organic changes occur in the retinal vessels.
- The third stage is hypertensive retinopathy. It is characterized by the appearance of pathological foci of opacification around altered retinal vessels, hemorrhages and dystrophic lesions of the central part of the retina, a “star” or “half-star” pattern, which is determined from case to case.
- The fourth stage is called hypertensive neuroretinopathy. When it occurs, angiopathy, angiosclerosis and retinopathy are complicated by edema and clouding of the retina over the optic nerve head. Changes in the retina and optic nerve are more pronounced; there is a significant deterioration in visual acuity and a narrowing of its fields.
Symptoms of diabetic macroangiopathy
With atherosclerosis of the coronary arteries, coronary heart disease appears in acute or chronic forms. Diabetic microangiopathy is often diagnosed together with aneurysms and arrhythmia, heart failure. Patients with diabetes die from heart attacks twice as often as patients without diabetes.
Atherosclerosis of the cerebral arteries is often accompanied by chronic cerebral ischemia.
Diabetic microangiopathy is characterized by numb feet, lameness in gait, swelling of the limbs, pain in the muscles of the thighs and buttocks during physical activity. A sharp disruption of blood flow causes critical ischemia, with the development of which comes necrosis of the foot and leg. Gangrene also occurs against the background of skin damage due to cracked feet or fungal infection. In more minor disturbances of blood flow, a chronic trophic ulcer develops.
Prevention and prognosis
The prognosis for ocular angiopathy depends entirely on the course of hypertension. Patients who manage to maintain normal blood pressure readings for a long time are not at risk of blindness. Patients facing aggressive forms of hypertension need to prepare for a serious decrease in visual acuity.
There are no specific preventive measures for this disease, because hypertension is often a hereditary disease. To avoid complete loss of vision, people prone to high blood pressure should regularly measure this indicator and take medications prescribed by their doctor. Twice a year they need to be examined by an ophthalmologist, and if signs of angiopathy are detected, follow additional instructions.
Diagnosis of diabetic macroangiopathy
Diagnosis of diabetic microangiopathy helps to identify the stage of damage to coronary, cerebral, and peripheral vessels. The determination will also involve an endocrinologist, diabetologist, cardiologist, neurologist and cardiac and vascular surgeon.
Diagnostics of diabetic angiopathy takes place in two directions, in the first, the research method is aimed at assessing the general condition of the patient, the second is aimed at determining the degree of damage to the vessels of the limb and performing reconstructive surgery to save the limb.
A research method assessing the patient’s general condition helps determine the severity of diabetes mellitus, pathological changes in the heart and kidneys. During outpatient diagnosis, blood tests, electrocardiography, and X-rays of the affected foot are used. Purulent discharge from the foot wound is also taken for analysis to determine the microflora. Blood pressure is measured in the tibial arteries.
A biochemical blood test is performed to determine glucose and cholesterol levels. The cardiovascular system is examined using ECG, myocardial perfusion scintigraphy and computed tomography angiography.
Signs of hypertensive retinopathy
A complex change in the condition of the retinal vessels (angiopathy) in hypertension, accompanied by a persistent increase in blood pressure in ophthalmology is usually called hypertensive retinopathy. Hypertensive retinopathy is one of the most commonly identified complications of high blood pressure. It is manifested by severe hemorrhages and exudate in the fundus, in some cases, swelling of the optic nerve.
Often the disease is virtually asymptomatic. In the later stages of its course, a significant decrease in visual acuity is noted.
Hypertensive retinopathy can occur in people of any age and gender, but is especially common among older people and people with high blood pressure (including hypertension due to kidney and adrenal disease).
Treatment of diabetic macroangiopathy
During treatment, the progression of dangerous vascular complications that threaten the patient with disability or death slows down. Therapy for diabetic macroangiopathy is aimed at correcting the syndrome of hyperglycemia and arterial hypertension.
To replenish carbohydrate metabolism, patients undergo insulin therapy with monitoring of blood glucose levels. Correction of carbohydrate metabolism occurs through the administration of lipid-lowering drugs and a diet limiting animal fats.
Symptoms
Signs and treatment of hypertensive macroangiopathy depend on the main factors in the occurrence of the disease and the condition of the blood vessels in general. The types of damaged vessels are also important. If the disease affects the limbs, the person feels pain, discomfort, swelling and bluish skin. It is even possible to develop gangrene if the vessels become clogged. With macroangiopathy, the patient sometimes limps, and the gait changes.
If the disease affects the brain, then strokes and ischemic attacks occur, from which the brain suffers. Typically, such patients suffer from constant headaches, memory loss, dizziness to the point of fainting, pressure changes and darkening in the eyes. It is important to know that these are signs of hypertensive macroangiopathy.
If the disease affects the heart vessels, then ischemia and then a heart attack may develop. A person suffers from shortness of breath from any physical activity, he suffers from constant pain in the back and chest, feels tired and overwhelmed. The symptoms of the disease worsen if the patient does not take any measures to cure it. Further development of cardiac vascular macroangiopathy threatens myocardial infarction, severe pain and exercise intolerance.
If angiopathy affects the kidneys, then cure is almost impossible. The kidneys begin to suffer from edema, which impairs the electronic and water processes in them. As a result, kidney failure develops. So, we learned what hypertensive macroangiopathy is and the signs (symptoms) of this disease. How to identify it and with what?
Preventive measures
You can protect yourself from such a disease - just listen to the following advice and follow them unquestioningly.
- The diet should include vegetables, fruits, fish and dairy products. We exclude fatty and fried foods. Salt is also an enemy, so it is necessary to reduce its amount.
- Bad habits are bad for your health. Alcohol and smoking are prohibited.
- The patient must monitor his mental state, avoid stress, depression, and be sure to follow the correct daily routine. At the request of the patient, the attending physician may prescribe sleeping pills or sedatives.
- If you have a sedentary lifestyle, you need to walk in the fresh air more often, engage in light sports: swimming, walking, physical therapy.
- Even if you don't have diabetes, it's a good idea to check your blood sugar levels daily.
Acute short-term complications of diabetes mellitus
Ketoacidosis
Diabetic ketoacidosis DKA is an acute insulin deficiency. If diagnosed late without treatment, it can lead to coma and death. It can develop in any type of diabetes, but is more common in type I.
Reasons for development
Without insulin, glucose does not enter cells. Instead, the body begins to break down fats as a source of energy. As a result, toxic ketone bodies are formed in excess. Within a few days they enter the blood and urine.
Early signs of pathological process:
- dry mouth, thirst, dry skin;
- high blood sugar level – 13 mmol/l and above;
- constant fatigue;
- frequent urination;
- weight loss.
When the level of ketone bodies in the body becomes critical, acute ketoacidosis develops. Its symptoms:
- abdominal pain, nausea and vomiting;
- a characteristic fruity smell from the mouth (usually felt by others, and not by the patient himself);
- high levels of ketone bodies in the blood and urine;
- drowsiness, lethargy;
- frequent, deep, sometimes difficult breathing;
- inability to concentrate;
- disturbance of consciousness.
From the moment vomiting appears, the pathology begins to progress rapidly to a life-threatening condition. If these symptoms appear, you should urgently call a doctor or an ambulance.
Therapeutic tactics for symptoms of DKA
First, blood glucose levels are measured. If it is 13 mmol/L or higher, measure the level of ketone bodies in the urine using test strips.
If this indicator is normal:
- short-acting or ultra-short-acting insulin is administered;
- Prescribe plenty of fluids - an average of 1 l/hour;
- monitor blood sugar levels and the level of ketone bodies in urine every 4-6 hours (the interval is determined by the doctor);
- treat concomitant pathologies (if any);
- limit physical activity to the minimum possible (it promotes more intense formation of ketone bodies).
If the level of ketone bodies is higher than normal, infusion therapy is indicated (carried out in a hospital or at home under the supervision of a doctor).
Hyperosmolar coma
Hyperosmolar diabetic coma is an extreme degree of metabolic disorder without ketoacidosis and background critical hyperglycemia (33 mmol/l and above). The body becomes dehydrated, and the levels of nitrogen, sodium and chlorine in the blood increase. With late diagnosis and treatment, mortality in hyperosmolar coma is 30-50%.
Causes of the condition:
- blood loss;
- a significant increase in the volume of urine excreted - due to the use of diuretics or other medications, dialysis, administration of saline solutions;
- diarrhea and vomiting;
- acute circulatory disorders;
- injuries and burns;
- severe infectious diseases.
Aggravating factors are increased blood glucose levels and the addition of concomitant diseases.
Signs of hyperosmolar coma
For 5-14 days before the attack, there is increased thirst and appetite, frequent and/or excessive urination, loss of strength and muscle weakness, up to the complete cessation of physical activity.
What to do
It is necessary to call an ambulance - treatment is carried out in the intensive care unit or intensive care unit. Treatment tactics include:
- rehydration - drip intravenous administration of medicinal solutions under the control of venous and blood pressure, the level of dehydration and the level of electrolytes in the blood plasma;
- insulin therapy.
Hypoglycemia
A decrease in blood glucose levels below 3.9 mmol/l. In a relatively mild form it is not dangerous: the patient himself can restore normal sugar levels. Severe forms of hypoglycemia damage brain cells and are life-threatening.
The condition occurs:
- due to insulin overdose;
- overdose of glucose-lowering drugs;
- increased insulin sensitivity due to exercise;
- local heating, massage, excessive depth of injection;
- increasing the interval between insulin and food;
- skipping meals;
- lack of carbohydrates;
- fasting;
- slowing down the evacuation of stomach contents;
- drinking alcohol.
Signs of hypoglycemia
Most patients feel an increase in hypoglycemia - they develop warning symptoms:
- shiver;
- heartbeat;
- pallor;
- fatigue;
- inability to concentrate;
- anxiety;
- sweating;
- increased appetite;
- sensory disturbances - goosebumps, numbness, etc.;
- nightmares.
As the sugar level decreases, dizziness, speech and vision disturbances, and convulsions are added. In a hypoglycemic coma, a person loses consciousness.
Treatment
In case of hypoglycemia, it is important to restore normal blood glucose levels. For relatively mild forms, it is enough to eat sugar, candy, a piece of chocolate, or honey. In severe forms, you need to call a doctor or an ambulance. Dextrose or glucan is administered intravenously to the patient.
Lactic acid coma
A sharp increase in the level of lactic acid in the blood.
Causes
Develops due to oxygen deficiency in tissues due to anemia, shock, carbon monoxide poisoning, alcohol or certain medications. It may occur against the background of kidney, liver, bone marrow, or bleeding diseases. The cause may also be myocardial infarction, serious illness or excessive physical activity.
Signs of lactic acidotic coma
The condition develops rapidly, within a few hours. The main manifestations are chest pain, diarrhea, noisy breathing, abdominal pain and vomiting, drowsiness or insomnia. Reflexes may disappear and motor activity may be impaired - muscle activity decreases or, on the contrary, involuntary movements appear. The patient's body temperature drops, urine ceases to be excreted, the contractility of the heart muscle decreases, blood clots form and even necrosis of the fingers.
Treatment
- Drip administration of a solution of soda, methylene blue or triamine, as well as small doses of insulin in 5% glucose.
- In severe cases, connection to an artificial kidney apparatus is indicated.
Prevention of diabetes complications:
- correct treatment regimen - correctly selected drug and dose (sugar levels are always normal);
- fulfilling all doctor's orders;
- weight normalization;
- normal motor activity;
- sufficient sleep;
- balanced diet;
- regular examinations by an endocrinologist, vascular surgeon, neurologist, ophthalmologist, podologist, nephrologist.
Professional medical supervision, patient self-discipline and a healthy lifestyle can reduce diabetes complications to a minimum or even prevent them altogether.
Diet for diabetic angiopathy
Diet 9th table
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1400 - 1500 rubles per week
A huge role in normalizing the condition of blood vessels in diabetes is played by diet therapy, which helps normalize the state of all types of metabolism and hormonal balance. The main techniques are:
- limiting the consumption of simple carbohydrates, but at the same time ensuring sufficient daily calorie intake according to height, weight, physical activity, etc.;
- replacing animal fats with vegetable ones;
- compliance with the drinking regime;
- control the consumption of table salt - no more than 5 g per day;
- if nephropathy is suspected, switch to a low-protein diet;
- increasing the consumption of lipotropic substances, mostly found in cottage cheese, fish, and oatmeal;
- the presence of plant foods in the diet - fruits and vegetables.