Pathologies of the vascular system of the eye are recognized as one of the main factors of low vision, blindness, and therefore limited vision in people of various age categories. In recent years, there has been an increase in ischemic eye diseases, which is due to the widespread prevalence of atherosclerosis, hypertension, coronary heart disease, and diabetes mellitus.
A classification system for ocular ischemia has not yet been developed. There is a close relationship between lesions of individual parts of the circulatory system and the mechanisms responsible for the development of ischemia. In this regard, ischemic eye diseases are characterized by polyetiology, the absence of a single pathogenesis and the diversity of the clinical picture.
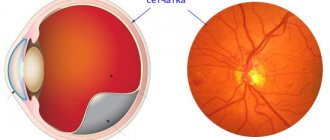
Thus, the clinical picture of ischemic damage to the posterior segment of the eye is largely determined by the characteristics of blood circulation in the area of the optic nerve and retina.
Ischemic processes occurring in the eye are usually divided into acute and chronic. Acute ischemia of the posterior ocular segment is characterized by circulatory disorders of the central retinal artery (CRA) or its central vein (CVS), anterior or posterior ischemic and acute toxic neuropathy.
Acute ischemia becomes a consequence of chronic ocular ischemia (diabetic or hypertensive angioretinopathy, degenerative changes in the retina, stenosis of the carotid or orbital arteries, temporal arteritis). The basis of ischemia is common angiospastic diseases, traumatic lesions of the eye and head. There have been cases of the occurrence of ischemic neuropathies with impaired blood flow in the CAS and CVS, as well as in their branches, with hypotension, taking certain medications and after surgical operations, if the predisposing factors were: microembolization, anemia, disorders of the blood coagulation or anticoagulation systems.
Acute disorders of the blood supply to the retina and optic nerve in the vast majority of cases cause partial loss of vision or blindness. The prognosis of the condition is always serious, but often not hopeless. Often, under the influence of treatment, the process improves or stabilizes. Quite often repeated courses of treatment are necessary.
Often, ischemic optovascular syndrome is a harbinger of ischemic coronary and cerebral attacks. In this regard, not only eye diseases, but also concomitant diseases require long-term careful treatment.
Acute circulatory disorder of the retinal vessels
With occlusion of the central retinal artery (OCAC), obstruction of the central retinal artery or its branches occurs, caused by thrombosis, embolism, or vascular spasm. Spasm manifests itself as vegetative-vascular disorders or organic changes in the vascular wall due to hypertension, atherosclerosis, etc., which is typical, in particular, for older people. In patients with ACAS, systemic diseases are distributed as follows: sclerotic lesions of the cardiovascular system - 35%, hypertension - 25%, heart defects - 8%, temporal arteritis - 3%. And in almost 25% of cases, the cause of CASC is never determined.
OCSA is a predominantly unilateral disease, without a clearly limited age category of patients (20 - 85 years). Men are more often affected by the disease.
Diagnostics
Diagnosis of pathology is carried out in a hospital setting. If a patient is suspected of developing a stroke, he urgently needs to undergo examination by a neurologist. The doctor evaluates a person’s reflexes, his speech, orientation in space, and vision. If a stroke is confirmed, consultation with an ophthalmologist is also required.
Among the instrumental diagnostic techniques used:
- computed tomography;
- CT angiography (vascular visualization);
- Magnetic resonance imaging.
These methods help to determine the location and degree of occlusion and select the necessary treatment measures. X-rays of the person are often performed to identify the presence of malformations, vascular aneurysms, and other abnormalities. Ultrasound and electrocardiography are used to identify pathologies that caused the development of an ocular stroke. Blood and urine tests show glucose concentrations, electrolytes and kidney metabolites.
To diagnose an attack, a comprehensive examination is used
In addition to confirming an ocular stroke, these techniques make it possible to identify at an early stage such dangerous conditions as renal failure, hypertensive crises, heart attacks and others.
Clinical signs
As a rule, patients note a sudden and persistent decrease in vision or sectoral loss of visual fields. Before the development of the characteristic pattern of ACAS, complete blindness occurs in approximately 15% of cases.
The decrease in visual acuity is significant: in 10% of cases, blindness occurs, in 50% of cases, fingers can be distinguished from the face, in 20%, visual acuity is 0.1-0.2. If any of the branches of the central nervous system is affected, visual acuity may be preserved, but defects occur in the visual field.
In young people, embolism of the central nervous system or its branches is more often observed. This occurs due to endocrine and septic diseases, acute infections, rheumatism, and injuries.
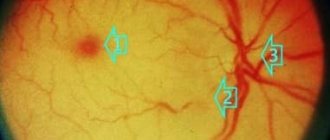
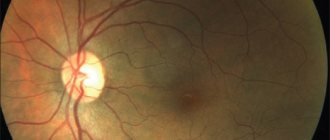
When examining the fundus, a typical finding is gray-white diffuse opacification of the retina, narrowing of individual or all branches of the central retina. In the area of the central fovea, an area of bright hyperemia is detected, standing out against the background of blanching of the retina, called the “cherry pit” symptom. This is explained by the thinning of the retina and the translucency of the bright red lining of the vessel in the indicated place. At the beginning of the disease, the optic disc remains pink in color and only then gradually turns pale due to its atrophy.
Sometimes a characteristic ophthalmoscopic picture may be absent: the area of retinal edema is localized only paramacularly or in the form of scattered areas. In such cases, the arteries are narrowed slightly, which indicates a small degree of occlusion. The presence of an additional cilioretinal artery often eliminates the “cherry pit” symptom and provides high visual acuity due to the preservation of central vision.
With embolism of the central nervous system, the prognosis is always pessimistic. In young people, after a spasm, vision can return almost completely; the prognosis in older people is much worse.
Blockage of any of the branches of the central nervous system partially reduces vision, and only the corresponding sector of the visual field is lost.
What it is
The disease is a condition accompanied by spasm, blockage (ischemic) or rupture (hemorrhagic) of a blood vessel in the eyeball. An attack can develop acutely or be sluggish. In the first case, we are talking about the appearance of severe pain, loss of certain parts of vision or complete blindness, numbness of the limbs. A sluggish stroke can cause alternations between deterioration and improvement of well-being, and minor visual disturbances. Whatever the symptoms, you should not let the disease take its course; you should consult a doctor as soon as possible.
Treatment
In case of acute obstruction of the central nervous system or its branches, it is necessary to immediately administer general and local vasodilators: a nitroglycerin tablet under the tongue, inhalation of amyl nitrite (a few drops on a cotton swab), 0.5 ml of atropine solution 0.1% retrobulbar, intravenous 0.3-0, 5 ml of xanthinol nicotinate solution 15%, intravenously 10 ml of aminophylline solution, intramuscularly or intravenously 1-2 ml of papaverine solution or xanthinol nicotinate solution 15%.
For thrombosis of the central nervous system, anticoagulant therapy, control of blood clotting and prothrombin time are recommended: fibrinolysin with retrobulbar heparin (5-10 thousand units), heparin up to 10 thousand. ED subcutaneously 6 times a day, then use indirect anticoagulants - finilin up to 4 times a day, 0.03 mg for the first few days, then once a day.
Additionally, anti-sclerotic and vitamin therapy is used (miscleron, methionine, vitamins A and C, B6, B12).
By contacting the Moscow Eye Clinic, each patient can be sure that highly qualified refractive surgeons - one of the best Russian specialists in this field - will be responsible for the results of surgical intervention. The high reputation of the clinic and thousands of grateful patients will certainly add to your confidence in the right choice. The most modern equipment for the diagnosis and treatment of eye diseases, some of the best specialists and an individual approach to the problems of each patient are a guarantee of high treatment results at the Moscow Eye Clinic.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 (800) 777-38-81 (daily from 9:00 to 21:00, free for mobile phones and regions of the Russian Federation) or using the form online entries.
Treatment tactics
Treatment for stroke always depends on several aspects. This includes the type of pathology, features of its course, causes, symptoms in the patient and some other factors. Laser coagulation is considered the most effective and safe method. The use of a laser allows you to effectively get rid of a blood clot, which helps restore blood flow in the affected area and prevent dangerous complications. The same technique is used for retinal detachment.
Another type of therapy is hyperbaric oxygen therapy. Its essence is the use of oxygen under pressure. In this case, the patient is in a hermetic pressure chamber.
Drug therapy includes groups of drugs designed to eliminate a blood clot, normalize blood circulation, relieve spasms, and normalize blood pressure. Treatment includes:
- antihypertensive drugs. To normalize blood pressure, the patient is prescribed diuretics, beta blockers, calcium antagonists, and ACE inhibitors. The decision on the type of drug in a particular case is made by the attending physician, depending on the characteristics of the course of the disease;
- anticoagulants. The main goal of therapy for ocular stroke is to restore normal blood flow. Since the cause of circulatory disorders is most often a blockage with a blood clot, to eliminate it, agents are prescribed that help dissolve blood clots;
- antispasmodics. These medications relieve spasm and pain that develop during an attack.
Treatment tactics depend on the characteristics of the pathology
Depending on the patient’s concomitant pathologies, other medications may be prescribed, for example, non-steroidal anti-inflammatory drugs, corticosteroids, narcotic analgesics, etc.
What are the causes of stroke?
What is the cause of stroke? Given the statistics, there may be various reasons. For example, arterial hypertension or atherosclerosis. Plus, unhealthy diet, dyslipidemia, alcoholism, severe stress, etc. Heredity also plays an important role.
An ischemic stroke develops as a result of a disruption in the passage of blood through one of the blood vessels supplying the brain. For example, due to occlusion of the carotid arteries. The cause of a sharp deterioration in cerebral blood supply may be a minor vascular spasm or thromboembolism. In turn, the cause of the latter is often cardiac pathology. The occurrence of the second type of stroke, that is, hemorrhagic, may be associated with the presence of various vascular pathologies. For example, cerebral atherosclerosis, systemic vasculitis and collagenosis. Rarely, but there are still cases when this type of stroke directly depends on blood clotting or incorrect therapy with anticoagulants and fibrinolytics.
Recommendations
Stroke is an extremely serious disease that leads to damage not only to the visual organs, but also to other organs. Therefore, immediate contact with specialists at the first signs of a stroke is of paramount importance. It is also important to note that an independent disease such as an eye stroke often occurs. In this case, a separate course of treatment is prescribed. The recovery period will directly depend on how quickly medical care was provided and, of course, on the degree of damage and the age of the patient. Today, strabismus after a stroke can be cured in various ways or using an integrated approach. What kind of therapy will be determined solely by the ophthalmologist.
Prevention
Testing for cardiovascular disease is key to preventing ocular strokes. This may include regular cholesterol and blood pressure checks, as well as discussion of other risk factors for heart disease, such as family history, diet and lifestyle.
Heart disease risk factors play a role in the risk of ocular strokes. An article in the journal Eyes found that 64% of people had at least one new, undiagnosed risk factor for heart disease that was discovered after a stroke. The biggest factor for these people was high cholesterol.
In general, to maintain healthy blood vessels and prevent eye stroke, people should do the following:
- exercise regularly; The Physical Activity Guidelines for Americans recommend 2.5 hours per week.
- Eat a healthy diet including plenty of fruits, vegetables, whole grains and unsaturated fats.
- work with a nutritionist, as recommended for some people.
- avoid smoking or quit smoking
- work with your doctor to treat other conditions, such as diabetes.
Prevention
Prevention comes down to the treatment and prevention of affecting diseases. Regular visits to a therapist, vision and fundus examinations should be carried out at least once a year.
Precautionary measures:
- avoid eye strain, wear safety glasses when working with a computer and telephone;
- avoid smoking, drinking alcohol;
- dose physical and emotional stress;
- maintain a sleep-wake schedule;
- do not take any medications without first consulting your doctor;
- know and treat chronic and hereditary pathologies;
- take courses of vitamin complexes to improve immunity, especially in the spring and autumn.
Taking precautions and knowing the basic symptoms and methods of recognizing an eye stroke will help you avoid such a terrible condition. If this happens, react in time and correctly and maintain your health.
diagnosing
Sudden vision loss is a medical emergency.
To diagnose an eye stroke, doctors may need to perform tests on the retina. These may include
- Eye dilation with drops for easier vision on the retina.
- Using a dye and camera to take photographs of the retina, known as fluorescein angiography. The dye is injected through the arm and allows the doctor to better see the veins and arteries of the retina.
- Checking the pressure in the eyes using air flow.
- A slit lamp examination, which uses eye drops, a special light, and a microscope to examine the inside of the eyes.
- Vision tests, such as reading eye charts and testing side or peripheral vision.
These tests are painless and are performed by an eye doctor known as an ophthalmologist.