The terms “arterial hypertension” and “hypertension” are often perceived as synonymous words. Many people think that both diagnoses mean the same thing - high blood pressure. However, this is not entirely true.
One of these terms actually means high blood pressure, and the second is the name of a disease that can cause high blood pressure. In order not to confuse two similar names, let's look at the differences between the diagnoses of hypertension and hypertension.
Unfortunately, some patients and their relatives, having collected a lot of useful information about diseases, feel the desire to engage in treatment personally. However, this is strictly prohibited.
To perform such serious functions, it is necessary to have fundamental knowledge and a wide range of useful skills and abilities. Observation and treatment should be carried out by a doctor - a qualified specialist with experience.
Why is hypertension dangerous?
The heart pumps blood through the blood vessels, providing all the body's cells with oxygen and nutrients. When blood vessels become clogged or lose their elasticity, the heart begins to work harder and increases the pressure inside the vessels.
Against the background of the disease, if not treated in a timely manner, serious pathologies such as acute heart failure, hypertensive crisis, stroke, and myocardial infarction can occur.
The difficulty of hypertension is that it often remains virtually asymptomatic for years and the person does not know about the existence of the disease. Symptoms are often observed - headache, fatigue, memory loss, dizziness, high blood pressure, to which a person simply does not pay attention. This may indicate the beginning of the development of the disease.
Main features
Often high blood pressure (hypertension) is diagnosed after the age of 45-50 years. If a person is attentive to himself, he notices painful changes and may suspect an increase in blood pressure. But sometimes people are unaware of hypertension because they do not know its symptoms. This lasts until the first hypertensive crisis, when the pressure jumps sharply to the upper values.
A gradual increase in blood pressure may last for several months. Therefore, you need to know the symptoms of high blood pressure in order to diagnose the disease in time and begin treatment.
We list the main signs of high blood pressure (hypertension):
- Headache - surrounds the head with a “hoop” - spreads to the back of the head, temples and forehead;
- Redness of the facial skin;
- Feelings of pressure on the eyes from the inside;
- Swelling of the eyelids and face in the morning;
- Noise in ears;
- "Floaters" before the eyes.
If elevated blood pressure persists for some time, this causes changes in the functioning of the cardiac system. Heart pain appears, heart rhythm is disturbed, shortness of breath is possible.
Small blood vessels are also damaged. With chronic high blood pressure, they cannot withstand pressure, become depleted, and rupture. Vision, hearing, and tactile sensations deteriorate.
Hypertension is accompanied by chronic hypertension. Therefore, the signs of hypertension and hypertension are the same (headache, redness, swelling, spotting and noise). High blood pressure is the main symptom by which one judges the presence of hypertension and begins an examination.
Causes of hypertension
- Excess weight. People who are prone to obesity are several times more likely to suffer from heart disease. Also, excess weight causes increased levels of calcium and sodium in the blood, disruption of normal kidney function and diseases of internal organs. This, in turn, is an additional factor for the development of hypertension.
- Arterial sclerosis. Due to the presence of atherosclerotic plaques on the walls of blood vessels, normal blood circulation stops. The heart has to work harder to increase the pressure in the blood vessels.
- Stressful situations. During stress, blood pressure increases due to the release of the hormone adrenaline into the blood. By acting on the heart, adrenaline causes it to beat faster, throwing more blood into the vessels.
- Bad habits. Smoking, drinking alcohol, fatty and heavy foods increase pressure in blood vessels, form vascular spasms and lead to their damage.
- Age. Over the years, a person's heart wears out. The risk of developing hypertension increases with age if you do not pay due attention to your health. It is necessary to undergo preventive examinations and give up bad habits, if any. High blood pressure often develops in people over 35 years of age.
- Genetic predisposition. If first-degree relatives (father, mother, siblings, grandparents) suffer from hypertension, the risk of developing the disease increases.
- Sedentary lifestyle. At a low level of stress, metabolism slows down, the nervous system and other body systems are weakened, and immunity is reduced. The risk of developing hypertension increases by 50%.
Concepts
First, let's define what it is - hypertension and hypertension.
Let's look at the main reasons that cause diseases. Arterial hypertension and essential hypertension are most often observed in older people suffering from diseases of the heart and vascular system.
The key symptom is an increase in blood pressure. Experts note that the critical level becomes 120/80. If you see exactly this kind of data in the tonometer window, we are probably talking about hypertension here. To make sure that this is not a random result, not an episodic phenomenon, observation must be continued.
10-15 minutes have passed, but the pressure has not decreased? Is this not the first time you have noticed such a high indicator? Then it’s definitely time to talk about hypertension, identifying hypertension and cardiovascular disease with all the accompanying signs and side effects.
It is very important to start therapy on time to prevent the development of numerous complications characteristic of hypertensive heart and vascular disease.
Types of cardiac hypertension
There are many classifications of the disease, which are based on the patient’s appearance, blood pressure level, causes of increased blood pressure, and the nature of the disease. However, doctors everywhere use a classification based on the severity of the disease.
Hypertension 1st degree
– is also called the preclinical stage. This is the mildest form of hypertension, in which blood pressure reaches 140/90 mmHg. mercury column. Mild headaches, decreased performance, and general fatigue are observed. While the patient is at rest, the pressure normalizes.
Hypertension 2 degrees
– moderate stage, at which the pressure increases to 180/110 mm. rt. Art. formation of atherosclerotic plaques, hypertrophy of the left ventricle of the heart, and increased concentration of creatinine are observed.
Hypertension 3 degrees
– pressure rises to 220/115 mm. rt. Art. in this case, the risk of complications is high. With this degree of development of the pathology, the blood supply to the internal organs is disrupted. Stage 3 disease can manifest itself as renal failure, hemorrhage from the eyes, and blindness.
Blood pressure indicators for hypertension
The main manifestation of hypertension is a long-term and persistent increase in blood pressure (BP).
There are systolic (or upper) blood pressure, which shows the level of blood pressure at the moment the heart contracts, and diastolic (lower), which shows the level of blood pressure at the moment the heart relaxes.
Normal blood pressure levels are considered to be 120-134/80-84 mmHg, but data may vary due to emotional shocks, physical activity, changes in air temperature, etc. These fluctuations are normal; they reflect the body’s naturally programmed reaction to changes in living conditions. However, constantly elevated blood pressure in the absence of obvious reasons for this is a significant reason to take care of your health.
Arterial hypertension is indicated by a stable increase in blood pressure (systolic - above 140 mm Hg, diastolic - above 90 mm Hg when measured at a doctor’s appointment; 135/85 mm Hg and above - when measured independently) , confirmed by repeated measurements. To establish a diagnosis of arterial hypertension, two measurements with elevated blood pressure in the absence of physical and emotional stress are sufficient.
How to diagnose the disease?
When the first symptoms of hypertension appear, consult a cardiologist. He will conduct an examination and refer you for tests:
- general blood and urine analysis;
- blood test for hemoglobin;
- urine test for protein and glucose;
- electrocardiography;
- echocardiography;
- chest x-ray;
- biochemical blood test to detect cholesterol, urea, glucose and calcium levels;
- phosphates and uric acid;
- CT scan;
- ultrasonography.
Based on the results of the tests, the attending physician will determine whether hypertension is present, the stability of the increase in pressure, the degree of development of pathological changes in the internal organs, and the cause of the increased pressure.
Prevention
Every patient who often experiences high blood pressure can get rid of hypertension and hypertension. It is enough to simply eliminate the risk factors that constantly destabilize the condition in a timely manner.
- Refusal of dishes containing animal fats. By stopping eating fatty, fried foods, the patient will be able to significantly reduce the level of cholesterol in the blood, which clogs the blood vessels.
- Minimize the amount of salt you consume. It retains water in the body, and this is a direct path to increased blood pressure.
- Monitor your body weight. Hypertension and hypertension are inextricably linked with excess weight, which increases muscle tone and, accordingly, blood pressure.
- Physical activity. It is worth noting that in this case it is necessary to seriously approach the issue of drawing up a training program. As a sport, physical therapy combined with interval running training is perfect.
- Quitting smoking and drinking alcohol. With a condition such as hypertension, drinking alcohol and smoking is strictly prohibited. These bad habits not only contribute to the narrowing of blood vessels, but also poison the body. Medicines prescribed by your doctor should not be taken together with alcohol, otherwise you will not be able to avoid intoxication of the body.
When the first symptoms of high blood pressure appear, you should not self-medicate; you should immediately seek qualified medical help. Monitoring the patient and prescribing treatment should be carried out only by a specialist.
Treatment of hypertension
The method of treatment depends on the degree of development of the disease. In the first preclinical stage, normal blood pressure levels can be maintained without the use of medications. The patient needs to balance their diet, give up bad habits, lead an active lifestyle and normalize their sleep and work patterns.
When treating stage 2 hypertension, the doctor prescribes a medication for long-term use and with a minimum number of contraindications, combined with moderate activity and giving up bad habits. The drug is prescribed by a cardiologist after examining the patient. The drugs must be taken continuously as this can cause a stroke or heart attack.
Therapy of stage 3 hypertension is carried out with the help of 1-2 drugs from different drug groups in combination with an active lifestyle and stabilization of nutrition and sleep patterns.
- diuretics with a diuretic effect are prescribed for salt and water retention in the body;
- to normalize blood circulation - ACE inhibitors;
- calcium antagonists - to reduce the oxygen demand of the heart muscle;
- beta blockers for atrial fibrillation or other concomitant pathologies.
Therefore, when determining therapeutic therapy, the doctor must know the patient’s entire medical history, take into account contraindications, lifestyle and physical characteristics (body weight, height).
Hypertension is treated in Krasnoyarsk at the medical level. We have experienced cardiologists who will conduct a complete examination and examination, friendly medical staff and high-quality equipment. To make an appointment with a specialist or find out more detailed information, leave a request on the website or by calling the clinic 201-03-03.
Publications in the media
Arterial hypertension (AH, systemic hypertension) is a condition in which systolic blood pressure exceeds 140 mm Hg. and/or diastolic blood pressure exceeds 90 mmHg. (as a result of at least three measurements made at different times against the background of a calm environment; the patient should not take drugs that either increase or decrease blood pressure) • If the causes of hypertension can be identified, then it is considered secondary (symptomatic) • In the absence obvious cause of hypertension, it is called primary, essential, idiopathic, and in our country - hypertension • Isolated systolic hypertension is diagnosed when systolic blood pressure increases more than 140 mm Hg. and diastolic blood pressure less than 90 mm Hg • Hypertension is considered malignant when diastolic blood pressure is more than 120 mm Hg.
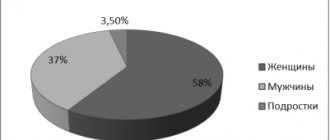
Statistics • 20–30% of the adult population suffers from hypertension. The prevalence increases with age and reaches 50–65% in people over 65 years of age, and in the elderly, isolated systolic hypertension is more common, which occurs in less than 5% of the population under the age of 50 years. Before the age of 50, hypertension is more common in men, and after 50 years - in women. Among all forms of hypertension, mild and moderate account for about 70–80%, in other cases severe hypertension is observed • Secondary hypertension accounts for 5–10% of all cases of hypertension, the remaining cases are essential hypertension (hypertension). However, according to specialized clinics, using complex and expensive research methods, secondary hypertension can be detected in 30–35% of patients.
Etiology and pathogenesis • The etiology of hypertension is currently far from completely clear; genetic abnormalities have been identified (see Genetic aspects below). Etiology of secondary hypertension - see Symptomatic arterial hypertension • The main factors determining the level of blood pressure are cardiac output and peripheral vascular resistance. An increase in cardiac output and/or peripheral vascular resistance leads to an increase in blood pressure and vice versa • In the development of hypertension, both internal humoral and neurogenic (renin-angiotensin system, sympathetic nervous system, baro- and chemoreceptors) and external factors (excessive consumption of table salt, alcohol, smoking, obesity) •• Prevalence of vasopressor factors - renin, angiotensin II, vasopressin, endothelin •• Vasodepressor factors - natriuretic peptides, kallikrein-kinin system, adrenomedullin, nitric oxide, Pg (PgI2, prostacyclin).
Genetic aspects. There are many known genetic abnormalities that contribute to the development of hypertension: mutations: angiotensin gene, aldosterone synthetase, b-subunit of amiloride-sensitive sodium channels of the renal epithelium, as well as a lot of loci of the so-called predisposition to the development of hypertension.
Risk factors • Complicated family history •• Lipid metabolism disorders in the patient and his parents •• Diabetes in the patient and his parents •• Kidney disease in parents (polycystic disease) • Obesity • Alcohol abuse • Excessive consumption of table salt • Stress • Physical inactivity • Smoking • Patient's personality type.
At-risk groups. Due to the involvement of various organs and systems in the pathological process, their influence on the course of the disease, groups of patients with high and very high risk are distinguished • The high-risk group includes patients with three or more risk factors, patients with target organ damage or patients with diabetes • The very high-risk group includes patients with concomitant diseases and risk factors.
Classification. Currently, two classifications are common in Russia - WHO and the International Society of Hypertension (1999) and WHO (1978).
Classification of hypertension by WHO and International Society of Hypertension (1999) • Optimal •• Systolic blood pressure: <120 mm Hg •• Diastolic blood pressure <80 mm Hg • Normal •• Systolic blood pressure <130 mm Hg •• Diastolic blood pressure < 85 mm Hg • High normal: •• Systolic blood pressure 130–139 mm Hg •• Diastolic blood pressure 85–89 mm Hg • Grade I (mild) •• Systolic blood pressure 140–159 mm Hg •• Diastolic blood pressure 90–99 mm Hg • subgroup: borderline •• Systolic blood pressure 140–149 mm Hg •• Diastolic blood pressure 90–94 mm Hg • Grade II (moderate) •• Systolic blood pressure 160–179 mm Hg .st •• Diastolic blood pressure 100–109 mm Hg • III degree (severe) •• Systolic blood pressure >180 mm Hg •• Diastolic blood pressure >110 mm Hg • Isolated systolic •• Systolic blood pressure >140 mm Hg .st •• Diastolic blood pressure <90 mm Hg • subgroup: borderline •• Systolic blood pressure 140–149 mm Hg •• Diastolic blood pressure <90 mm Hg • Note. When determining the degree, the highest blood pressure value should be used, for example 140/100 mmHg. — II degree of hypertension.
WHO classification of hypertension (1978) • Stage I - increased blood pressure more than 160/95 mm Hg. without organic changes in the cardiovascular system • stage II - high blood pressure •• with hypertrophy of the left ventricle of the heart •• either with proteinuria and/or a slight increase in the concentration of creatinine in the blood plasma (not more than 176.8 µmol/l) •• or with widespread or localized ( retina) changes in arteries • Stage III - high blood pressure with damage to the heart, brain, retina, kidneys (myocardial infarction, heart failure, cerebrovascular accident, retinal hemorrhage, renal failure).
Blood pressure measurement
• Measurement must be carried out after resting for 5 minutes. 30 minutes before this, it is not recommended to eat, drink coffee, drink alcohol, exercise, or smoke. When measuring, your legs should not be crossed, your feet should be on the floor, your back should rest on the back of the chair. A hand rest is required, and the bladder must be emptied before measurement. Failure to comply with these conditions can lead to an increase in blood pressure: after drinking coffee - by 11/5 mm Hg, alcohol - by 8/8 mm Hg, smoking - by 6/5 mm Hg, with a full urinary bladder - 15/10 mm Hg, in the absence of support for the back - systolic by 6–10 mm Hg, in the absence of support for the arm - by 7/11 mm Hg.
• The shoulder should be at the level of the IV–V intercostal space (a low elbow position increases systolic blood pressure by an average of 6 mm Hg, a high elbow position underestimates blood pressure by 5/5 mm Hg). The shoulder should not be compressed by clothing (measurement through clothing is unacceptable) - systolic pressure may be overestimated by 5–50 mmHg. The lower edge of the cuff should be 2 cm above the elbow (improper application of the cuff can lead to an overestimation of blood pressure by 4/3 mmHg), and it should fit snugly to the upper arm. The air in the cuff should be inflated to 30 mm Hg. above the disappearance of the pulse on the radial artery. The stethoscope should be placed in the cubital fossa. The moment the first sounds appear will correspond to phase I of Korotkoff sounds and shows systolic blood pressure. The rate of decrease in pressure in the cuff is 2 mm/s (slow decompression increases blood pressure by 2/6 mm Hg, fast decompression increases diastolic blood pressure). The moment of disappearance of the last sounds will correspond to the V phase of Korotkoff sounds and corresponds to diastolic blood pressure.
• Measured parameters should be indicated with an accuracy of 2 mmHg. When measuring, it is necessary to listen to the area of the cubital fossa until the pressure in the cuff decreases to zero (you should remember about possible aortic valve insufficiency and other pathological conditions with high pulse pressure, large stroke volume of the heart). During each examination of the patient, blood pressure is measured at least twice on the same arm and the average values are recorded. During the first examination, the pressure is measured on both arms, and subsequently on the arm where it was higher. The difference in blood pressure between the left and right arms should not exceed 5 mmHg. More significant differences should be alarming regarding vascular pathology of the upper extremities.
• When measuring blood pressure with the patient lying down, his arm should be slightly elevated (but not suspended) and be at the level of the middle of the chest.
• Repeated measurements should be carried out under the same conditions. It is necessary to measure blood pressure in a patient in two positions - lying and sitting - in the elderly, with diabetes, in patients taking peripheral vasodilators (to identify possible orthostatic arterial hypotension).
Clinical manifestations are nonspecific and depend on target organ damage.
• Cerebral symptoms •• The main symptom is headache, often on awakening and usually in the occipital region •• Dizziness, blurred vision, transient cerebrovascular accident or stroke, retinal hemorrhages or papilledema, movement disorders and sensory disorders • Intellectual-mnestic disorders.
• Cardiac symptoms •• Palpitations, pain in the heart area, shortness of breath (due to pronounced changes in the heart with hypertension, every second patient has cardiac symptoms) •• Clinical manifestations of coronary artery disease •• Left ventricular dysfunction or heart failure.
• Kidney damage: thirst, polyuria, oliguria, nocturia, microhematuria.
• Peripheral arterial disease: cold extremities, intermittent claudication.
• Hypertension is often asymptomatic.
• It is possible to detect (by palpation) volumetric formations in the kidney area, as well as listen to a systolic murmur over the kidney area.
• Examination - signs of some endocrine diseases accompanied by hypertension: hypothyroidism, thyrotoxicosis, Itsenko-Cushing syndrome, pheochromocytoma, acromegaly.
• Palpation of peripheral arteries, auscultation of vessels, heart, chest, abdomen suggest vascular damage as the cause of hypertension, suspect aortic disease, suggest renovascular hypertension.
Features of collecting anamnesis • Family history of hypertension, diabetes, lipid metabolism disorders, coronary heart disease, stroke, kidney disease • Duration of hypertension and its evolution, previous blood pressure level, results and side effects of previous antihypertensive treatment • Presence and course of coronary artery disease, heart failure, stroke, other diseases in this patient (gout, bronchospastic conditions, dyslipidemia, sexual dysfunction, kidney disease) • Clarification of symptoms of presumably secondary hypertension • Detailed questioning about taking medications that increase blood pressure (GCs, oral contraceptives, NSAIDs, amphetamines, epoetin beta, cyclosporine) • Lifestyle assessment (consumption of table salt, fat, alcohol, smoking, physical activity) • Personal, psychosocial and external factors influencing blood pressure (family, work).
Laboratory and special research methods. It is necessary to exclude symptomatic hypertension, identify risk factors and the degree of target organ involvement.
• OAC (anemia, erythrocytosis, leukocytosis, increased ESR - secondary hypertension).
• OAM - leukocyturia, erythrocyturia, proteinuria, cylindruria (symptomatic hypertension), glucosuria (DM).
• Biochemical tests to determine the concentration of potassium ions, creatinine, glucose, cholesterol (secondary hypertension, risk factors). It should be remembered that a rapid decrease in blood pressure with long-term hypertension of any etiology can lead to an increase in creatinine levels in the blood.
• ECG - left ventricular hypertrophy, rhythm and conduction disturbances, electrolyte disturbances, signs of ischemic heart disease (changes in the terminal part of the ventricular complex, scar changes).
• EchoCG to detect left ventricular hypertrophy, assess myocardial contractility, and identify valvular defects as a cause of hypertension.
• Ultrasound of the kidneys, adrenal glands, renal arteries, peripheral vessels to identify secondary hypertension.
• Fundus examination: hypertensive retinopathy - narrowing and sclerosis of the arteries (symptoms of copper or silver wire), Salus phenomenon.
Diagnostic tactics. The diagnosis of hypertension (essential, primary hypertension) is established only by excluding secondary hypertension. Goals of diagnostic measures for hypertension • Determination of a possible cause • Identification of concomitant diseases • Identification of risk factors for coronary artery disease. Since hypertension itself is one of the risk factors for CHD, the presence of another risk factor further increases the likelihood of developing CHD; in addition, the prescribed treatment can seriously affect risk factors - for example, diuretics and non-selective beta-blockers in the presence of dyslipidemia and insulin resistance can aggravate these disorders • Identification of target organ involvement in the hypertensive process. Their defeat has the most serious impact on the prognosis of the disease and approaches to its treatment.
Differential diagnosis • Renoparenchymal hypertension - see Arterial hypertension, renoparenchymal • Vasorenal hypertension - see Arterial vasorenal hypertension • Endocrine hypertension constitutes approximately 0.1–1% of all hypertension (up to 12% according to specialized clinics) •• With pheochromocytoma (see Pheochromocytoma ) •• With primary hyperaldosteronism (see Hyperaldosteronism) •• With hypothyroidism - high diastolic blood pressure; other manifestations of the cardiovascular system - decreased heart rate and cardiac output •• In hyperthyroidism - increased heart rate and cardiac output, predominantly isolated systolic hypertension with low (normal) diastolic blood pressure; an increase in diastolic blood pressure in hyperthyroidism is a sign of another disease accompanied by hypertension or a sign of hypertension • Drug hypertension - vasoconstriction due to sympathetic stimulation or direct effects on vascular SMCs, increased blood viscosity, stimulation of the renin-angiotensin system, ion retention may be important in the pathogenesis sodium and water, interaction with central regulatory mechanisms - for more details, see Symptomatic Arterial Hypertension.
TREATMENT
The goal is to reduce cardiovascular morbidity and mortality by normalizing blood pressure, protecting target organs, eliminating risk factors (smoking cessation, compensation for diabetes, reducing the concentration of cholesterol in the blood and excess body weight).
• Recommendations of WHO and IAH (International Society of Arterial Hypertension; 1999) •• In young and middle-aged people, as well as in patients with diabetes, it is necessary to maintain blood pressure at the level of 130/85 mm Hg •• In elderly people, the target blood pressure level is £140 /90 mmHg
• Excessive rapid decrease in blood pressure with significant duration and severity of the disease can lead to hypoperfusion of vital organs - the brain (hypoxia, stroke), heart (exacerbation of angina, myocardial infarction), kidneys (renal failure).
Treatment plan • Control of blood pressure and risk factors • Lifestyle changes • Drug therapy.
Non-drug treatment is indicated for all patients. In 40–60% of patients with the initial stage of hypertension with low blood pressure values, it is normalized without the use of drugs. In case of severe hypertension, non-drug therapy in combination with medication helps to reduce the dose of drugs taken and thereby reduces the risk of their side effects. The mechanisms leading to a decrease in blood pressure are considered to be a decrease in cardiac output, a decrease in peripheral vascular resistance, or a combination of both mechanisms.
• Diet •• Limiting table salt intake to less than 6 g/day (but not less than 1–2 g/day, since in this case compensatory activation of the renin-angiotensin system may occur) •• Limiting carbohydrates and fats, which is very important in the prevention of coronary heart disease , the likelihood of which is increased in hypertension (risk factor). A decrease in excess body weight by 1 kg leads to a decrease in blood pressure by an average of 2 mm Hg •• An increase in the content of potassium and calcium ions in the diet •• Refusal or significant limitation of alcohol intake (especially if it is abused).
• Physical activity - sufficient cyclic activity (walking, light jogging, skiing) in the absence of contraindications from the heart (coronary artery disease), blood vessels of the legs (atherosclerosis obliterans), central nervous system (cerebrovascular accidents) reduces blood pressure, and at low levels it can normalize his. Moderation and gradual dosing of physical activity is recommended. Physical activity with a high level of emotional stress (competition, gymnastics), as well as isometric efforts (weight lifting) are undesirable.
• Other methods - psychological (psychotherapy, autogenic training, relaxation), acupuncture, massage, physiotherapeutic methods (electrosleep, diadynamic currents, hyperbaric oxygenation), water procedures (swimming, shower, including contrast), herbal medicine (chokeberry, tincture of hawthorn, motherwort, mixtures with marsh cudweed, hawthorn, immortelle, sweet clover).
Drug therapy
Basic principles: • It is necessary to begin treatment of mild hypertension with small doses of drugs • Combinations of drugs should be used to increase their effectiveness and reduce side effects • It is preferable to use long-acting drugs (12–24 hours with a single dose).
• b-blockers •• Preference should be given to b-blockers when hypertension is combined with coronary artery disease (angina pectoris and unstable angina, post-infarction cardiosclerosis, heart failure), tachyarrhythmias, extrasystoles •• After abrupt withdrawal of b-blockers, withdrawal syndrome may develop, manifested by tachycardia, arrhythmias, increased blood pressure, exacerbation of angina, development of myocardial infarction, and in some cases even sudden cardiac death. To prevent withdrawal syndrome, a gradual reduction in the dose of the b-blocker is recommended for at least 2 weeks. There is a high-risk group for the development of withdrawal syndrome - these are people with hypertension in combination with angina pectoris, as well as with ventricular arrhythmias •• Drugs ••• Non-selective (blockade of b1- and b2-adrenergic receptors): propranolol 40–240 mg/day at 3 doses, pindolol 5–15 mg 2 times/day, timolol 10–40 mg/day in 2 divided doses ••• Selective (cardioselective) b1-blockers: atenolol 25–100 mg 2 times/day, metoprolol 50–200 mg/day in 2 doses, nadolol 40–240 mg/day, betaxolol 10–20 mg/day.
• Diuretics •• Varieties ••• Thiazides and thiazide-like diuretics (used most often in the treatment of hypertension) are diuretics of moderate potency, suppress the reabsorption of 5–10% of sodium ions (drugs: hydrochlorothiazide 12.5–50 mg/day, cyclopenthiazide 0, 5 mg/day, chlorthalidone 12.5–50 mg/day) ••• Loop diuretics (characterized by the rapid onset of action when administered parenterally) are strong diuretics, suppress the reabsorption of 15–25% of sodium ions (the main drug is indapamide 2.5 mg /day in one dose; furosemide at a dose of 20–320 mg/day is rarely prescribed for continuous use for antihypertensive purposes) ••• Potassium-sparing diuretics are weak diuretics, cause additional excretion of no more than 5% of sodium ions (drugs: spironolactone 25–100 mg / day, triamterene 50–100 mg 4 times / day.) •• Preference for diuretics in the treatment of hypertension is given if there is a tendency to edema and in old age.
• ACE inhibitors •• Preferred for the treatment of hypertension with the following concomitant conditions (diseases): ••• left ventricular hypertrophy (ACE inhibitors are most effective in its regression) ••• hyperglycemia ••• hyperuricemia ••• hyperlipidemia (ACE inhibitors do not aggravate these conditions) ••• history of myocardial infarction ••• heart failure (ACE inhibitors are among the most effective drugs for the treatment of heart failure; they not only weaken its clinical manifestations, but also increase the life expectancy of patients) ••• older age •• Drugs ••• captopril 25–150 mg/day ••• enalapril 2.5–40 mg/day ••• fosinopril 10–60 mg/day ••• lisinopril 2.5–40 mg/day ••• ramipril 2, 5–10 mg/day ••• benazepril 10–20 mg/day.
• Slow calcium channel blockers •• Preferred in the treatment of hypertension in combination with angina (especially vasospastic), dyslipidemia, hyperglycemia, broncho-obstructive diseases, hyperuricemia, supraventricular arrhythmias (verapamil, diltiazem), left ventricular diastolic dysfunction, Raynaud's syndrome •• With bradycardia or predisposition to it, a decrease in myocardial contractility, conduction disturbances, verapamil or diltiazem, which have pronounced negative inotropic, chronotropic and dromotropic effects, should not be prescribed, and, conversely, the use of dihydropyridine derivatives is indicated •• Due to the different sensitivity of patients to slow calcium channel blockers, treatment begins with small doses •• Drugs ••• Diltiazem 120–360 mg/day ••• Isradipine 2.5–15 mg/day ••• Nifedipine (extended dosage form) 30–120 mg/day ••• Nitrendipine 5–40 mg /day ••• Verapamil 120–480 mg/day ••• Amlodipine 2.5–10 mg/day ••• Felodipine 2.5–10 mg/day.
• Angiotensin II receptor blockers •• These drugs are preferable when a dry cough appears during treatment with ACE inhibitors, renal failure (especially in diabetes mellitus) •• Drugs ••• losartan 25–100 mg in 1 or 2 doses ••• valsartan 80 mg 1 time / day ••• eprosartan 600 mg 1 time / day ••• candesartan.
• a-blockers •• For long-term treatment of hypertension, selective a1-blockers are mainly used (prazosin 1–20 mg/day, doxazosin 1–16 mg/day, terazosin) •• This group of drugs is widely used in urology in the treatment of benign hyperplasia prostate gland •• Despite many positive effects, drugs in this group are rarely used as monotherapy. Apparently, this is due to disadvantages and side effects, although the danger of most of them is most likely exaggerated. The main indications are combination therapy •• Disadvantages: “first dose phenomenon” (pronounced decrease in blood pressure after the first dose), orthostatic arterial hypotension, long-term selection of the drug dose, development of tolerance (effect evasion), withdrawal syndrome. To prevent the “first dose phenomenon”, it is recommended to take an a-blocker in bed, followed by staying in a lying position for several hours (it is better to take it at night).
• Centrally acting drugs (in recent years they have gradually lost their importance) •• Centrally acting drugs cause a decrease in blood pressure due to inhibition of the deposition of catecholamines in central and peripheral neurons (reserpine), stimulation of central a2-adrenergic receptors (clonidine, guanfacine, methyldopa, moxonidine) and I1 -imidazoline receptors (clonidine and especially the specific agonist moxonidine), which ultimately weakens the sympathetic influence and leads to a decrease in peripheral vascular resistance, a decrease in heart rate and cardiac output •• Drugs in this group are mainly used orally for the treatment of hypertension. Preference should be given to imidazoline receptor agonists as first-line agents for diabetes and hyperlipidemia (they do not aggravate metabolic disorders), COPD (the drugs do not affect bronchial patency), severe hypersympathicotonia, left ventricular hypertrophy (they cause its regression). Methyldopa is most often used in the treatment of hypertension in pregnant women •• Drugs: reserpine and combination drugs containing it (reserpine + dihydralazine + hydrochlorothiazide, reserpine + dihydroergocristine + clopamide), methyldopa up to 2 g / day (when combined with other antihypertensive drugs, no more than 500 mg /day), clonidine at an initial dose of 0.075 3 times / day in 2 divided doses, moxonidine up to 0.4 mg / day in 2 divided doses, guanfacine 1-3 mg / day.
Combination therapy. According to international multicenter studies, the need for combination therapy occurs in 54–70% of patients. Indications for combination therapy are as follows: • Ineffectiveness of monotherapy. Monotherapy with an antihypertensive drug is effective on average in 50% of patients with hypertension (a higher result can be achieved, but then the risk of side effects will increase). To treat the remaining part of the patients, it is necessary to use a combination of two or more antihypertensive drugs • The need for additional protection of target organs, primarily the heart and brain.
Rational combinations of drugs. The most common combination of a diuretic and some other class of drug is used. In some countries, combination therapy with a diuretic is considered a mandatory step in the treatment of hypertension • The most effective combination is a combination of a diuretic and an ACE inhibitor (possibly a fixed combination, for example, capozide, Korenitek) • The combination of a diuretic and an angiotensin II receptor blocker is rational • Approximately the same additive effect has a combination of a diuretic and a beta-blocker (this combination is not the most successful, since both the diuretic and the beta-blocker affect the metabolism of glucose and lipids).
Irrational combinations of antihypertensive drugs can lead to both increased side effects and an increase in the cost of treatment if there is no effect. A striking example of an irrational combination is the combination of beta-blockers and slow calcium channel blockers (verapamil, diltiazem), since both groups of drugs worsen both myocardial contractility and AV conduction (increased side effects), while the combination of beta-blockers with dihydropyridines (for example, nifedipine) is positive.
Treatment of certain types of hypertension
• Resistant (refractory) hypertension - the inability to achieve a reduction in blood pressure to target values (less than 140/90 mm Hg) for more than 1 month in patients with hypertension during combination therapy with two or three antihypertensive drugs in sufficient dosages •• To confirm the diagnosis, it is necessary to test all rational combinations of drugs (primarily including diuretics, the combination “ACE inhibitor + slow calcium channel blocker” is also effective), then prescribe a triple combination in a variety of options, then a combination of four drugs (usually minoxidil is used as one of the components) • • One should remember about possible pseudo-resistance, the cause of which may be symptomatic hypertension, non-compliance with the rules of taking medications, inappropriate dosage, irrational combination of drugs, taking alcohol and drugs that increase blood pressure, weight gain, increased blood volume (for example, in heart failure), deliberate administration the patient misleads the doctor (simulation) •• In each case of resistant hypertension, a thorough examination of the patient is necessary, preferably in a specialized hospital to exclude symptomatic hypertension.
• Hypertension in the elderly •• Treatment should begin with non-drug measures, which in this case quite often reduce blood pressure to the target level. Of great importance is limiting the consumption of table salt and increasing the content of potassium and magnesium salts in the diet •• Drug treatment is based on the pathogenetic features of hypertension at a given age. In addition, it should be remembered that various concomitant diseases often occur in the elderly ••• It is necessary to start treatment with smaller doses (often half the standard) ••• The dose should be increased gradually over several weeks ••• The dose is selected under constant monitoring of blood pressure, and it is better to measure it in a standing position to identify possible orthostatic arterial hypotension ••• It is advisable to use a simple treatment regimen (1 tablet - 1 time / day) ••• You should use medications with caution that can cause orthostatic arterial hypotension (methyldopa, prazosin, labetalol) , and centrally acting drugs (clonidine, methyldopa, reserpine), the use of which in old age is quite often complicated by depression or pseudodementia. When treating with diuretics and/or ACE inhibitors, it is advisable to monitor renal function and blood electrolyte composition.
• Endocrine hypertension - see Symptomatic arterial hypertension.
• “Alcoholic” hypertension - see Symptomatic arterial hypertension.
Complications of hypertension: • MI • acute cerebrovascular accident • heart failure • renal failure • hypertensive encephalopathy • hypertensive retinopathy • hypertensive crisis • dissecting aortic aneurysm.
The prognosis significantly depends on the adequacy of the prescribed therapy and the patient’s compliance with medical recommendations.
Reduction. AH - arterial hypertension.
ICD-10 • I10 Essential (primary) hypertension • I11 Hypertensive heart disease [hypertensive disease with predominant damage to the heart] • I12 Hypertensive [hypertensive] disease with predominant damage to the kidneys • I13 Hypertensive [hypertensive] disease with predominant damage to the heart and kidneys • I15 Secondary hypertension • O10 Pre-existing hypertension complicating pregnancy, childbirth and the puerperium • O11 Pre-existing hypertension with associated proteinuria