Treatment tactics
Treatment of pulmonary artery diseases depends on the severity of the process. As for stenosis, in the absence of pronounced manifestations, there is no need for surgical intervention, but clinical observation and symptomatic therapy are required.
As the pathology progresses, the question of surgical treatment arises. When the pressure gradient increases above 50 mmHg, the question of surgery is not discussed - it must be performed immediately. Operation options are different. Valvuloplasty can be open, closed, endoscopic - balloon. Indications for a specific intervention are determined by a specialist.
The main directions in the treatment of pulmonary hypertension are the prevention of thrombosis, elimination of spasm of vascular smooth muscle fibers, stopping the proliferation of connective tissue structures of the vascular wall. In this case, the following application is indicated:
· drugs that normalize blood clotting;
· diuretics;
cardiac glycosides;
· vasodilators;
· oxygen therapy.
In case of hypertension, called secondary, complex measures should correct the underlying pathology - the root cause of the increase in pressure in the artery. The list often includes bronchodilators and corticosteroids.
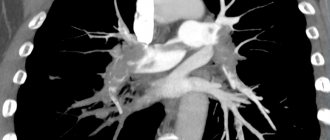
Surgical treatment for hypertension: embolectomy, lung transplant, pulmonary-cardiac complex transplant.
Publications in the media
Pulmonary valve insufficiency is the inability of the pulmonary valve to prevent the reverse flow of blood from the pulmonary trunk into the right ventricle during diastole.
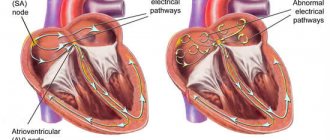
Etiology • Relative deficiency in pulmonary hypertension • Congenital defects • Infectious endocarditis in drug addicts • Marfan syndrome • Rheumatism • Carcinoid syndrome • Syphilis • Idiopathic dilatation of the pulmonary artery. Pathophysiology • Pulmonary valve regurgitation leads to volume overload of the right ventricle • In the absence of pulmonary hypertension, the right ventricle is able to cope with significant volume overload as long as its normal contractility is maintained and there is no severe tricuspid valve regurgitation • When pulmonary valve regurgitation and pulmonary hypertension combine, overload occurs right ventricle both volume and pressure • In acute severe pulmonary valve insufficiency - right ventricular failure.
Clinical picture and diagnosis • Complaints arise due to associated right ventricular failure and tricuspid insufficiency. • Objective data •• Swelling of the jugular veins •• Palpation detectable pulsation of the right ventricle •• Palpation detectable II tone and diastolic tremor •• Strengthening of the pulmonary component of the II sound •• In case of leaflet defects, the pulmonary component of the II tone is weakened or absent •• Decreasing diastolic Graham Still murmur . The duration of the noise depends on the rate of equalization of diastolic pressure in the pulmonary artery and right ventricle.
Special studies • ECG: signs of hypertrophy and overload of the right heart. • Jugular venogram: wave V indicates tricuspid regurgitation due to right ventricular failure. • Chest X-ray •• Bulging of the pulmonary artery arch •• Increased pulmonary vascular pattern and dilatation of the right heart depend on the presence or absence of pulmonary hypertension. • EchoCG •• Vegetations, dilatation of the fibrous ring of the pulmonary artery, bulging of the interventricular septum into the cavity of the left ventricle •• Severity of regurgitation (see Aortic valve insufficiency) •• Increased systolic pressure in the right ventricle and pulmonary artery. • Catheterization of the cardiac cavities •• Increasing end-diastolic pressure in the right ventricle and central ventricle •• Carrying out tests with aminophylline and oxygen to determine the reversibility of pulmonary hypertension. • Pulmonary angiography: the flow of contrast material from the pulmonary artery into the right ventricle during its diastole.
TREATMENT • Drug therapy •• Treatment of right ventricular failure (diuretics and venous vasodilators) •• For any organic damage to the valve - prevention of infective endocarditis; for relative failure, prevention is not indicated. • Surgical treatment •• Indications: clinically pronounced right ventricular failure in severe infective endocarditis that does not respond to antibiotic therapy •• Methods of surgical treatment: valve replacement with a biological or, less commonly, mechanical prosthesis. See also Tricuspid valve insufficiency.
Specific complications • PE • Secondary infective endocarditis • Thrombosis of the prosthesis • Degenerative changes in the biological prosthesis and the need for re-prosthesis. The prognosis depends on complications and concomitant pathology; Pulmonary valve insufficiency itself usually does not affect the prognosis.
ICD-10 • I37 Pulmonary valve lesions
Pulmonary stenosis
Pulmonary artery stenosis (narrowing) can be caused by isolated valvular, subvalvular or peripheral obstruction, and also occurs in combination with more severe congenital heart defects.
Pulmonary stenosis with an isolated valve occurs in 8-12% of cases of congenital heart defects in children. Subvalvular stenosis can result in a funnel-shaped appearance of the artery and is often found in children with a normal pulmonary valve. This condition may be caused by tetralogy of Fallot.
Peripheral narrowing of the pulmonary artery can lead to obstruction at the level of the main pulmonary artery, at the bifurcation, or in more distal branches. In some places, there is difficult patency, but stenosis can be caused by other congenital cardiac anomalies, for example, a ventricular septal defect or patent ductus arteriosus, etc.
Stenosis can be diagnosed in utero or shortly after birth. Critical narrowing of the pulmonary artery is considered potentially dangerous for newborns.
Ultrasound imaging of the heart during pregnancy may show isolated valve stenosis due to abnormal thickening or bicuspidity of the valve. Also, with the help of ultrasound, the doctor can detect stenosis caused by rubella infection during fetal development or accompanied by other congenital anomalies, such as tetralogy of Fallot or Noonan syndrome.
In infants, the condition is usually diagnosed by the presence of systolic murmurs while listening to the lungs with a phonendoscope.
Symptoms and diagnosis of pulmonary artery stenosis
Symptoms of stenosis depend on the severity of the pathology. The mild form may be asymptomatic; a more severe form of the pathology may cause the following symptoms:
- dyspnea
- chest pain
- fainting during exercise
- causeless fainting
Soft pulmonary systolic murmurs are heard when the child is lying down, but such murmurs can also be heard in healthy children and may be associated with physiological changes in the respiratory system.
Diagnosis of pulmonary artery stenosis may consist of the following procedures:
- echocardiography – allows you to confirm the presence of a valve defect;
- ECG - shows the presence of ventricular hypertrophy, right atrium and other abnormalities in the physiology of the heart;
- angiography allows you to confirm the diagnosis and is often prescribed to children with multiple cardiac anomalies;
- A chest x-ray allows the doctor to determine the enlargement of the right ventricle and atrium.
Treatment of pulmonary stenosis
Initial treatment of critical heart disease in a newborn includes general resuscitation and medications to dilate the ductus arteriosus. In the absence of pathological symptoms and the blood pressure in the right ventricle is less than 60 mm Hg. Art. The child is seen by a cardiologist every 1-2 years. These routine examinations include ECG, echocardiography and chest x-ray.
For infective endocarditis, surgical treatment is performed:
- in case of symptoms and blood pressure in the ventricle more than 60 mm Hg. Art. Cardiac catheterization is performed using valvotomy, which leads to the elimination of pulmonary valve insufficiency. If the procedure does not correct the problem, the pulmonary valve may need to be replaced;
- Percutaneous pulmonary valve implantation is an alternative to surgical valve correction and replacement of right ventricular dysfunction;
- Pulmonary artery balloon angioplasty, with or without placement of an expandable metal stent, can be used to treat the disease.
Heart valve defects and their treatment
Heart valve therapy includes several methods: 1) drug treatment; 2) valve reconstruction surgery; 3) valve replacement surgery; and 4) transcatheter valve replacement. Although drug therapy cannot eliminate valve dysfunction, it can relieve symptoms in many cases. If valve reconstruction or replacement becomes necessary, your cardiologist, surgeon, or interventional cardiologist will tell you about possible treatment options. The choice between replacement or reconstruction depends on a number of factors, including which valve is affected, the severity of the disease, and the presence of stenosis or regurgitation.
Your Cardiology Team
If you are undergoing heart valve reconstruction or replacement surgery, you will be cared for by a team of medical specialists who are committed to ensuring your safety and comfort before, during and after surgery. The following information describes the different health care providers you may see during your treatment.
Your general practitioner (GP) may be the first to detect symptoms of heart valve disease or a condition that may cause the valve to become damaged or malfunction. The therapist may prescribe special tests to confirm the diagnosis or refer you to an appropriate specialist.
A cardiologist is a doctor who specializes in heart disease. A cardiologist does not perform heart surgery, but usually performs diagnostic tests to determine the cause of heart problems and prescribe treatments to correct heart problems. Your cardiologist may prescribe medications and/or refer you to a cardiovascular surgeon.
A cardiovascular surgeon is a doctor who specializes in heart surgery, including reconstruction or replacement of diseased heart valves. The surgeon is the key decision maker in deciding the timing and best strategy, including the surgical technique and the choice of medical device for your valve case.
An interventional cardiologist (interventional cardiologist) is a doctor who has received additional specialized training to perform catheter-based procedures to treat heart disease. The interventional cardiologist works with the surgeon to make the right decision regarding the need for transcatheter aortic valve replacement.
An anesthesiologist is a doctor trained to administer sedation or general anesthesia (sleep) during surgery.
Intensive Care Unit Doctors and Nurses - In the Intensive Care Unit, the patient is closely monitored and maintained after most types of surgery. Together with your surgeon and/or cardiologist, intensive care unit doctors and nurses care for you during this time.
Approaches to surgical treatment of heart valve defects
Most heart surgeries are performed through an incision along the entire length of the chest, or breastbone. This incision is called a median sternotomy. Typically the healing process goes quite well, requiring about 6 weeks for the bone to fully recover.
In some patients, heart valve surgery can be performed using small, or minimally invasive, incisions. Smaller incisions offer patients many benefits. Preoperative studies, including coronary angiography, echocardiography, and, in many cases, a chest CT scan (computed axial tomography), help determine which patients may benefit from minimally invasive surgery. Surgical approaches that involve small incisions also involve the use of a heart-lung machine, as do sternotomy surgeries.
Transcatheter aortic valve replacement (TAVR): a less invasive alternative to open heart surgery
If a patient has been diagnosed with severe aortic stenosis but open-heart surgery carries moderate or high risk, another option is available: transcatheter aortic valve replacement (TAVR). This procedure is also called transcatheter aortic valve implantation (TAVI). This is a minimally invasive surgery that does not require open heart surgery.
| The transcatheter aortic valve replacement procedure allows you to install a new valve into your diseased aortic valve. The new valve moves the flaps of your diseased valve to the side. The frame is implanted into the leaflets of your diseased valve to ensure proper placement. |
This minimally invasive procedure is different from open heart surgery. In transcatheter aortic valve replacement, instead of cutting into the chest and completely removing the diseased valve, the valve is replaced using a catheter.
Transcatheter aortic valve replacement can be performed in several ways, but the most commonly used is transfemoral (through an incision in the thigh). Only the cardiology team can determine the best method, taking into account the person's health and other factors.
Valve replacement surgery
If a cardiovascular surgeon decides to replace a patient's heart valve, the first step is to remove the diseased valve (removing the valve and calcium deposits) and the second is to implant a prosthetic heart valve in its place. Prosthetic valves, used to replace diseased natural valves, are made from a variety of materials and sizes.
There are two broad categories of prosthetic heart valves that are used to replace diseased valves:
- Biological prostheses are made primarily from animal tissue, namely bovine (cow) pericardium (the strong sac surrounding the heart), pig aortic valve, or human valves taken from a postmortem donor.
- Mechanical valves are made of a synthetic material, predominantly carbon.
Bioprosthetic valves
There is a wide variety of bioprosthetic valves:
- Heterograft (or xenograft) is valve or pericardial tissue of animal origin suitable for use in medicine (for example, cattle (cows) or pigs).
- Homograft (or allograft) are human valves obtained from a posthumous donor.
- Autograft/self tissue is a healthy valve that has been moved from one location in the human body to another to replace a damaged valve (applies only to the pulmonary valve, which is used to replace the aortic valve).
A xenograft is a biological valve made from animal tissue. Thus, pericardial valve leaflets are usually made from bovine pericardium (the sac surrounding the heart) and sutured to a flexible or semi-rigid frame. In addition, biological valve prostheses are made from porcine valves. The valve is made from a porcine aortic valve and is usually sutured to a flexible or semi-rigid frame to create a “scaffold” valve. Otherwise, the natural root of the porcine aorta remains unchanged and acts as a framework in a “frameless” valve. Each flap is surrounded by a fabric ring (cuff) for sewing. Sutures are placed through the cuff to attach the valve to the heart.
| Biological valve prostheses |
Mechanical valves
Mechanical valve blades are made of a special type of carbon. Such valves usually have two leaflets. The leaflets open and close during the cardiac cycle, allowing blood to flow in one direction.
Criteria and selection of heart valves
The choice between a mechanical and biological valve prosthesis depends on an individual assessment of the benefits and risks of each valve, as well as the lifestyle, age and health status of each patient.
Bioprostheses do not require long-term use of drugs that suppress the natural ability of blood to clot (anticoagulants). This is important for those who cannot take anticoagulants due to a history of major bleeding (eg, gastrointestinal or genitourinary) or an increased risk of traumatic injury and bleeding associated with activity, sports, or advanced age. Bioprostheses usually last at least 10 years, and in some cases more than 30 years. If a patient under the age of 60 years is implanted with a bioprosthetic valve, there is a high probability that at some point the need for a replacement valve will arise, whereas most patients aged 70 years and older do not require this.
Mechanical valves are subject to little wear. However, they require daily use of anticoagulants, which may require dietary or lifestyle changes.
Often the decision to choose a biological or mechanical valve prosthesis is related to the patient's age, with older patients predominantly receiving bioprostheses. However, there is no consensus regarding the exact age at which a bioprosthesis may be preferable to a mechanical valve.
Valve reconstruction surgeries
If possible, it is preferable to reconstruct the patient's valve rather than replace it with a prosthesis. Typically, during valve reconstruction surgery, the surgeon adjusts the tissue or underlying structures of the mitral or tricuspid valves.
Almost all valve reconstruction procedures involve the installation of a ring or half-ring for annuloplasty. This is a tissue-covered device that is implanted around the circumference, or opening, of the mitral or tricuspid valve. It provides support to the patient's own valve and allows the leaflets to close more tightly, potentially reducing leakage through the valve. There are many different annuloplasty products available. The surgeon will choose the one that best suits your heart valve.
| Annuloplasty rings |
In addition to annuloplasty, mitral valve reconstruction often requires correction of problems with the leaflets or chordae, which attach the valve leaflets to the heart. If the leaks are due to mitral valve prolapse, fixation of the leaflets and chordae (and implantation of a ring or half-ring for annuloplasty) restores normal valve function.
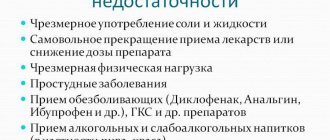
Caring for the patient after heart valve surgery
The normal recovery period after standard heart valve surgery is four to eight weeks. Recovery may be faster if a small incision was made, such as in minimally invasive and transcatheter surgeries. During this time, patients gradually gain strength and resume normal daily activities. Regular examination by a cardiologist is of great importance. Please contact your health care provider by phone or in person if you have any questions or concerns about your health, especially if you experience any unusual symptoms or changes in your general health.
Nutrition and exercise
Two additional important aspects of recovery and overall wellness are a healthy diet and regular exercise. If your doctor has recommended a special diet, it is important to follow it. Healthy eating is an integral part of a healthy life. During the recovery period, eating nutrient-dense meals will provide your body with energy and can help speed up the healing process.
To improve the overall health of the cardiovascular system, it is recommended to combine a balanced diet with your doctor's recommendations for physical activity and weight control. Maintaining a regular exercise program is an important part of maintaining a healthy lifestyle. With the guidance of your doctor, you should gradually increase your physical activity and activity level. Before starting a new sporting activity, consult your doctor.
Anticoagulants - It is important to follow your doctor's directions for taking medications, especially if an anticoagulant has been prescribed. Anticoagulants, or anti-clotting drugs, suppress the blood's natural ability to clot. If you are prescribed anticoagulants, you will need periodic blood tests to evaluate your blood's ability to clot. The result of such a study will help your doctor determine the required dosage of the anticoagulant. Finding the correct dosage of the drug may take some time, but consistency and cooperation with your doctor are important. Sometimes it is possible to conduct the test yourself at home; ask your doctor about this. Check with your doctor about interactions with other drugs you are taking and about dietary restrictions while taking anticoagulants. Learn about all the signs that may indicate your dosage is too high.
Other Medical Information —Before having any dental procedures, including dental procedures, endoscopy, or surgery, tell your doctor if you have a prosthetic heart valve. Patients with a prosthetic valve are more susceptible to infections, which can lead to heart damage in the future. Therefore, you may need to take antibiotics before and after some medical procedures to reduce the risk of infection.
Also, when traveling for more than a few days, try to keep your diet and exercise levels as close to your normal as possible. Be sure to discuss all medications you take (including over-the-counter medications) with your doctor, and do not change the dosage unless specifically instructed to do so.
Normal performance
To study the functioning of the CPA at the primary stage, a general clinical examination of the patient is used. Characteristic signs of violations:
- dyspnea;
- pulsation of the neck veins;
- pallor or cyanosis of the upper part of the body;
- during auscultation – additional noise at the point of valve projection.
Making a final diagnosis and choosing adequate treatment tactics depends on the results of instrumental methods that objectively assess the condition of this structure. The most common tests are electrocardiography (ECG) and echocardiography (echoCG).
ECG
There are no specific electrocardiographic signs of PC defects. Changes in the ECG occur when symptoms of heart failure due to a valve defect appear.
With regurgitation or stenosis of the pulmonary valve, hypertrophy of the right ventricle develops, which is established on the ECG in comparison with the state of the left sections.
Severe pancreatic hypertrophy (mass larger than left):
- the ventricular QRS complex is represented by qR or simply R in precordial lead V1;
- in V6 the QRS complex is deformed in rS, RS (occasionally – Rs);
- the degree of hypertrophy is reflected by the height of the R wave in V1 and the depth of S in V6 - the greater the difference between them, the more significant the increase in the myocardium;
- the ST segment in V1 is under the isoline, the T wave is negative;
- in V6 ST is located above the isoline, T-positive.
Moderate hypertrophy (the mass of the pancreas is less than the left one, but impulse conduction is slow):
- The QRS complex in V1 is observed as rsR or rSR;
- V6 deformation in qRS.
Moderate hypertrophy is represented by deformation of the QRS complex:
- in V1 – rS, RS, Rs;
- in V6 – qR;
- the amplitude of the R wave in V1 is increased;
- the S waves in V1 and R waves in V6 are reduced.
A shift of the electrical axis of the heart to the right is noted at each stage of hypertrophy.
ECHO
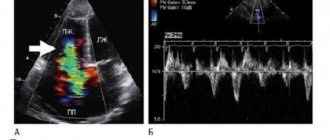
Ultrasound examination of the heart is considered the gold standard for diagnosing PC defects. The method allows you to study the anatomical features and functional state of the valves. To visualize internal hemodynamics, Doppler echocardiography is used.
The pulmonary valve on ECHO is depicted in the form of a three-lamellar formation, the elements of which bend into the lumen of the vessel during RV systole.
Standard PC indicators:
- structure – normoechoic, homogeneous;
- peak blood flow velocity – 0.5-1.0 m/s;
- average pressure gradient – up to 9 mm Hg. Art.;
- lumen diameter – 11-22 mm.
During ultrasound, the structure of the coronary artery and the presence of pathological formations are studied. The main changes for various defects are presented in the table.
| PA stenosis | Insufficiency (regurgitation) of the coronary arteries |
|
|
Pulmonary valve insufficiency
Pulmonary insufficiency occurs extremely rarely as a congenital anomaly. However, pathology often occurs as a complication after surgery or percutaneous angioplasty for pulmonary stenosis, as well as treatment for tetralogy of Fallot. Also, pulmonary valve insufficiency can develop as a result of a dilated pulmonary valve ring due to pulmonary hypertension or Marfan syndrome.
Significant pulmonary insufficiency can be caused by primary pulmonary hypertension, secondary pulmonary hypertension, infective endocarditis, rheumatic heart disease, carcinoid heart disease, Marfan syndrome and certain drugs, for example, methysergide, pergolide.
Pulmonary valve insufficiency is a serious pathology that is usually asymptomatic and is not accompanied by signs of right ventricular failure. With this pathology, a soft diastolic murmur is heard in the left upper region of the sternum and hypertrophy of the right ventricle is observed.
When diagnosing this pathology, the following studies are carried out:
- ECG;
- chest x-ray;
- color Doppler echocardiography;
- cardiac catheterization.
Treatment of pulmonary valve insufficiency
Pulmonary insufficiency usually does not require special treatment, but to monitor the pathology, it is necessary to conduct cardiograms every 1-3 years, depending on the severity and cause of the pathology. If symptoms or right ventricular dilatation are present, surgical pulmonary valve replacement is necessary. If severe right ventricular failure and pulmonary hypertension are detected, a heart transplant may be required.
Pulmonary insufficiency is usually well tolerated in childhood. Long-term studies have shown that pulmonary valve regurgitation can lead over time to progressive right ventricular dilatation, right ventricular dysfunction, exercise intolerance, gastric tachycardia, and, in extreme cases, sudden death.