As you know, pregnancy is a risk factor for the development of varicose veins: often, it is during the period of bearing a baby that “snakes” of dilated veins or spider veins appear on the legs. However, it is problematic for expectant mothers to treat this disease - they can only take measures to prevent the progression of the disease. But after childbirth, it’s time to give the disease a worthy rebuff, because now a woman has the opportunity to use the entire arsenal of therapeutic agents for this.
The word "varicose veins" comes from the Latin word "varix" - bloating. Varicose veins are a chronic disease accompanied by various disturbances in the outflow of blood in the veins associated with pathological changes in the venous valves, which often causes changes in the entire vascular system.
The problem of varicose veins has been known since the times of Hippocrates and Avicenna, who devoted entire sections of their works to the description and treatment of vein diseases. In Russia, more than 35 million people suffer from varicose veins, while women are exposed to a much larger number of risk factors compared to men. The problem of varicose veins is especially relevant for women during pregnancy and in the early postpartum period, especially if the disease arose before pregnancy.
How do varicose veins occur?
In order to deal with the problem of varicose veins, it is necessary to understand how the venous system of the legs is structured and how the outflow of venous blood occurs.
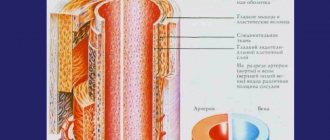
The venous system of the lower extremities consists of superficial and deep. Superficial veins are located directly under the skin, deep veins are located in the muscle layer of the leg and thigh. The connection between these two systems is provided by communicating (perforating) veins. In each vein there are valves that ensure blood flow in only one direction - from the periphery to the center.
The flow of venous blood to the heart is ensured by the contraction of the heart muscle, leg and thigh muscles (muscle pump). Another necessary factor is the full functioning of the venous valves, which, similar to heart valves, allow blood to flow in only one direction. When the muscles of the leg and thigh contract, the deep veins of the limb are compressed, and blood from them flows into the veins of the leg and thigh, as well as into the veins of the pelvis. Unmodified vein valves prevent blood from entering the superficial venous system. If the deep vein valves work normally, when the muscles relax, there is no return of blood from the pelvic veins.
An increase in pressure in the veins of the pelvis due to the growth and development of the fetus leads to the gradual destruction of the valves of the veins, as a result of which, during muscle contractions, blood under high pressure flows from the deep venous system to the superficial one. Increased pressure in the superficial veins leads to their expansion. This condition is called varicose veins. A separate group of manifestations of this disease includes the so-called spider veins, which arise due to the expansion of venous capillaries of the skin and subcutaneous tissue. They can be congenital or acquired, appearing anywhere on the human skin. But if they appear on the skin of the legs and are actively increasing, then they should be regarded as a symptom of incipient varicose veins.
Diagnostics
First of all, the doctor conducts an examination with palpation - already at this stage the disease can be detected. Additionally, the following studies can be carried out:
- Ultrasound examination of veins in combination with duplex or triplex scanning based on Doppler sonography. The procedure allows the doctor to examine the veins and valves in detail and determine the stage of the disease.
- Contrast X-ray venography. It consists of introducing a contrast agent into the body and monitoring the entire vascular network using x-rays.
- Functional tests to identify varicose veins, with which you can determine the volume of affected veins and the feasibility of surgical treatment.
These types of diagnostics allow you to obtain comprehensive information about the condition of the veins and the degree of development of the disease, thanks to which the doctor can make an accurate diagnosis and prescribe effective treatment.
Symptoms of varicose veins
Manifestations of varicose veins depend on the stage of the disease. At the beginning of the disease, when irreversible changes in the vessels and capillaries have not yet occurred, the only symptom may be “worms” of dilated veins in the legs. As the disease progresses, fatigue, a feeling of heaviness in the legs, bloating, cramps in the calf muscles (especially in the evening, and sometimes at night), numbness, and a tingling sensation appear. Swelling usually occurs in the evening, especially after prolonged standing or sitting, and disappears completely after a night's rest. Over time, as varicose veins progress and the valves of the veins are destroyed, trophic disorders appear (they are associated with a deterioration in the supply of oxygen and other substances to the tissues) - most often they occur on the inner surface of the lower third of the leg. These are induration (hardening, thickening of the skin), pigmentation, dermatitis (the appearance of areas of inflammation on the skin), then a trophic ulcer, which is difficult to treat.
Complications of varicose veins in pregnant women:
Nature made sure that during childbirth the mother did not lose a lot of blood. During pregnancy, under the influence of hormones, blood becomes thicker. Thick blood and venous congestion increase the risk of developing blood clots (thrombosis), resulting in the following complications:
- dermatitis, eczema of the skin over altered veins
- bleeding from dilated veins
- thrombophlebitis (inflammation of superficial veins with the formation of blood clots); manifested by redness, soreness and thickening along the vein, increased temperature
- deep vein thrombosis of the lower extremities; characterized by severe pain, severe swelling and enlargement of the affected limb, increased temperature
- BODY (pulmonary embolism) – a blood clot from varicose veins enters the branches of the pulmonary artery. It appears depending on the degree of damage. In severe cases: chest pain, increased pulse, drop in blood pressure, increased breathing, sudden loss of consciousness. The skin of the face takes on a bluish tint, and the veins in the neck swell. In mild cases: pain when breathing, cough, possible rise in temperature.
According to statistical data, thrombosis and BODY in pregnant women is observed 5-6 times more often than in non-pregnant women, and after childbirth 3-6 times more often than before childbirth. The risk is especially high after major blood loss during childbirth and caesarean section.
Possible complications of varicose veins
The greatest danger is not varicose veins itself, but its complications, which include:
- thrombophlebitis - inflammation of the veins;
- trophic ulcers resulting from a sharp deterioration in blood supply to the skin;
- thromboembolism - the formation of blood clots in veins of different diameters, blockage of the lumen of the veins, including large pulmonary veins.
As mentioned above, these complications most often occur in people with increased intra-abdominal pressure, which includes pregnant women. However, it must be remembered that an increase in intra-abdominal pressure in pregnant women is a temporary phenomenon and it occurs gradually.
Why do varicose veins develop after pregnancy or during pregnancy?
The body of a pregnant woman undergoes various fairly pronounced changes regarding the endocrine and reproductive systems, as well as the anatomical structure and position of the abdominal and pelvic organs, associated with their displacement of the increasing size of the uterus. Hormonal changes in a woman’s body affect not only the reproductive system, but also the functional state of the vein walls with their weakening. Also, the enlarged uterus compresses large venous vessels through which blood flows from the legs. This leads to stagnation of blood and increased pressure inside the veins, which accelerates the process of formation of pathological protrusions.
Prevention of varicose veins
In the absence of varicose veins before pregnancy and with correct behavior during pregnancy and after childbirth, the manifestations of the disease disappear. But, as we already know, it is easier to prevent a disease or identify it in the early stages (compensation stage) than to subsequently treat its advanced forms.
In order to suspect that you have varicose veins of the lower extremities, just look at your legs and listen to your feelings. In the stage of compensation for varicose veins, when the deep vein system is not affected, works as usual and there are manifestations only from the superficial veins, you can notice a slight expansion of the saphenous veins: they are soft, easily collapse, the skin over them is not changed. In the stage of decompensation (at this stage there are already changes in the valve apparatus and deep veins), a moderate or sharp expansion of the saphenous veins is determined; they are dense, sometimes painful, the skin over them acquires a pigmented tint (red, bluish or purple-brown).
If you have discovered at least one of the listed signs before pregnancy, you need to visit a phlebologist or vascular surgeon. And if this possibility does not exist, then contact the surgeon at the clinic at your place of residence.
Varicose veins can be prevented by knowing about the risk factors that contribute to its occurrence and development:
- hereditary predisposition;
- features of the anatomical structure and blood supply of the legs;
- the use of old-generation hormonal contraceptives (drugs with a high content of hormones that predispose to varicose veins are not currently sold);
- hard physical labor;
- prolonged stay in a sitting or upright position;
- decreased physical activity during pregnancy;
- chronic intestinal diseases, constipation;
- chronic lung diseases with prolonged debilitating cough.
Thus, among the risk factors there are those that we cannot influence (for example, heredity), but there are also those that we can completely eliminate.
For example, you should not stand or sit in one position for a long time. There is no need to stand in front of a bathtub or basin, washing your baby’s diapers and undershirts: this process can be completely entrusted to a washing machine.
Walking with your child will serve as feasible physical activity and exercise. But at the same time, you don’t have to walk until exhaustion or, conversely, sit for hours with a book, comfortably sitting on a bench.
Since high heels are also a risk factor for the progression of varicose veins, you should, if possible, avoid them.
After childbirth, a woman may continue or develop the problem of constipation: its solution also applies to measures to prevent varicose veins.
Diagnosis of the disease
This pathology has characteristic manifestations, which are characterized by the appearance of small nodular protrusions, which have a different consistency and bluish coloration. Therefore, a preliminary diagnosis is possible after examination by a surgeon. The first surgical department of the hospital, if necessary, conducts additional laboratory, instrumental and functional studies (rheovasography, hemogram, ultrasound examination), with the help of which the degree of damage to the walls of the veins, the causes of the disease, as well as the stage of its course are determined. These studies can also be carried out if varicose veins appear after childbirth.
Diagnosis of varicose veins
Currently, there is a huge arsenal of methods for diagnosing varicose veins. They are available and do not cause any discomfort. The most common and reliable methods include:
- Doppler ultrasound is the simplest and safest method, when ultrasound is used to determine the speed of blood flow in the superficial and deep venous systems;
- angioscanning - the method is similar to Doppler ultrasound; it allows you to more accurately determine the degree of venous insufficiency in small-caliber vessels and capillaries;
- Contrast X-ray phlebography - allows you to identify at what level the damage to the valve apparatus of the superficial and deep veins occurred, by introducing contrast (a special drug) and its movement along the vascular bed.
The simplest and least time-consuming measures that can be taken after childbirth if you have varicose veins during pregnancy are:
- wearing elastic stockings or bandages during the day;
- compliance with the regime of physical activity and rest;
- complex of therapeutic gymnastics.
It is necessary to wear elastic knitwear throughout the entire period of pregnancy and about a month after childbirth, which will prevent disruption of the vein valves.
How are varicose veins treated after childbirth?
You should consult a doctor immediately after the appearance of varicose veins, swelling, and heaviness in the lower extremities. The doctor, a phlebologist, conducts clinical and ultrasound examinations of the lower extremities. In the process of ultrasound duplex scanning, the picture of pathologically altered venous blood flow is determined in detail.
Diagnosis of varicose veins after childbirth
The doctor formulates a treatment regimen, its stages and timing of optimal implementation. Most often, radical treatment of varicose veins after childbirth is recommended to begin after the end of the breastfeeding period. Until this point, it is recommended to limit yourself to wearing compression hosiery and a regime of certain restrictions. Baths, saunas, other thermal effects, as well as increased physical activity are contraindicated. Hiking, cycling, swimming are shown.
Causes of varicose veins
Experts identify several common causes of varicose veins:
- Hereditary predisposition is often transmitted through the female line - in 75% of cases in patients with varicose veins, relatives (grandmothers, mothers) encountered the same problem. At the same time, varicose veins of the legs in women are not inherited, but congenital pathologies of the structure of the veins are observed (weakness of the vascular walls, inferior valves, etc.).
- Often the cause of varicose veins in women is associated with an unbalanced rhythm of life. Constantly wearing high heels, sedentary work, lack of physical activity, or overloading the legs due to prolonged standing leads to a decrease in vascular tone and blood stagnation in the veins. To compensate for this imbalance, the veins dilate, while women still experience swelling and a feeling of heaviness.
- Hormonal imbalance can also contribute to the development of varicose veins in women. This may be due to hormonal fluctuations from one menstrual cycle to another, the use of oral contraception, etc.
- The appearance of varicose veins may be associated with pregnancy and labor. At this time, the constantly growing child compresses the veins of the pelvis, plus the amount of blood and hormones in the woman’s body increases. Under the influence of such factors, the ligaments of the women’s pelvis become more elastic, and the extensibility of the veins and their walls increases.
If a woman has problems with her veins before pregnancy, this can ultimately affect her course. Pregnant women with varicose veins are at risk of bleeding after childbirth, untimely discharge of amniotic fluid, and weak labor. Therefore, in case of any pathologies of the veins or in the presence of a hereditary predisposition during pregnancy, it is necessary to be observed by a phlebologist.