Translation into English of the names and abbreviations of the arteries of the heart
Serzhenko Nadezhda Medical translation agency "Medtran"
Translation of coronary angiography results raises many questions even for an experienced medical translator. The topic is quite difficult for a number of reasons:
- Complex anatomy of the coronary arteries
- A huge variety of anatomical options
- Abundance of terms and abbreviations
- Lack of a unified nomenclature
- Almost every artery has several synonymous names in both Russian and English
A standard situation for a medical translator is that it is necessary to translate an extract from the patient’s medical history, which contains a description of the results of coronary angiography, or, among other medical documents, there is a protocol for angiography of the coronary arteries. If the translator does not have experience in such translations, then two paragraphs of such text may take several hours.
Many translation problems arise due to synonyms (different variants of the names of the same artery). In order to correctly translate the variant name of an artery encountered in a medical history (which does not always have an unambiguous analogue in English), it is often necessary to search and compare the description of the anatomical structure in Russian with the description in English to make sure that the selected English term corresponds to the Russian name for the artery.
To avoid distortion of meaning when translating the names of anatomical formations and angiographic terms into English, we strongly recommend using analogues that are as close as possible to the Russian original. Despite the fact that the same artery may have several names in both Russian and English, the use of synonyms should be kept to a minimum, because this makes verification difficult and is a potential source of error. The translation of a medical text must convey the content of the source text as closely as possible, and the translator does not have the right to interpret the available information at his own discretion. However, for correct translation it is necessary to understand the basics of angiography and know the anatomy of the coronary arteries.
The terms and explanations below are intended to facilitate the work of the translator and help avoid errors when translating angiocoronary angiograms.
The aortic sinuses
The aortic sinuses, or sinuses of Valsalva, are the pockets between the semilunar valves of the aorta and its wall. The names of the sinuses correspond to the names of the coronary arteries branching from them: the right coronary artery departs from the right coronary sinus, the left coronary artery departs from the left coronary sinus, and the posterior sinus of Valsalva is called non-coronary (non-coronary sinus), since the coronary arteries do not depart from it. The aortic sinuses facing the pulmonary artery are called “facing aortic sinuses”.
The aortic valve has three leaflets, each having a cusp or cup-like configuration. These are known as the left coronary cusp, the right coronary cusp and the posterior non-coronary cusp. Just above the aortic valves there are anatomic dilations of the ascending aorta, also known as the sinus of Valsalva. The left aortic sinus gives rise to the left coronary artery. The right aortic sinus which lies anteriorly, gives rise to the right coronary artery. The non-coronary sinus is positioned on the right side.
The aortic sinuses that are adjacent to the pulmonary valve (facing the pulmonary valve) are described as the 'facing' aortic sinuses.
Right aortic sinus (1st facial sinus, right sinus of Valsalva). Right coronary sinus, right anterior sinus, right sinus of Valsalva, right-facing sinus (anat.: anterior aortic sinus).
The right coronary artery arises from the right aortic sinus.
Left aortic sinus (2nd facial sinus, left sinus of Valsalva). Left coronary sinus, left anterior sinus, left sinus of Valsalva, left-facing sinus (anat.: left posterior aortic sinus).
The left aortic sinus is the origin of the left coronary artery.
Non-coronary aortic sinus (non-facial aortic sinus, posterior sinus of Valsalva). Non-coronary aortic sinus, posterior sinus of Valsalva, non-facing aortic sinus (anat.: right posterior aortic sinus, sinus aortae posterior dexter).
Non-facing aortic sinus is that aortic sinus that does not face the pulmonary artery. The first one from it, when oriented counterclockwise, is called the “1st facial sinus”, and the next one is the “2nd facial sinus” (Terminology developed by a group of researchers from Leiden University (A. Gittenberger: de Groot et al., 1983)).
Non-coronary aortic sinus is an aortic sinus from which the coronary arteries do not arise. Typically (in most people), the posterior (non-facial) aortic sinus is also non-coronary. However, there are many variations in the anatomical structure of the coronary arteries, both normal and pathological, so it is important to understand the difference between the terms “facial” and “coronary” (see comments on the figure).
A diagram explaining the definition of terms.
a: the nonfacial sinus of the aorta (H) is darkened, 1 and 2 - the 1st and 2nd facial sinuses (light), from which the coronary arteries arise;
b: in the case of the origin of the coronary arteries from one facial sinus of the aorta, the second (shaded) may turn out to be non-coronary. Thus, the terms “facial” and “coronal”, “non-facial” and “non-coronal” are not synonymous. Source: Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries. M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003.
Coronary arteries (coronary arteries)
The term “coronal” comes from the Greek “wreath, crown,” and “coronary” comes from the Latin “crown.” Both terms refer to the arteries of the heart and are absolute synonyms.
Right coronary artery and its branches
RCA - right coronary artery (RCA - right coronary artery).
Right coronary artery (RCA), right main coronary artery. The right coronary artery arises from the right aortic (1st facial) sinus, most often in the form of a trunk running posteriorly along the right atrioventricular groove, encircling the tricuspid valve, and heading towards the cross of the heart. The RCA typically arises from the right sinus of Valsalva (RSV) of the ascending aorta, passes anteriorly and to the right between the right auricle and the pulmonary artery and then descends vertically in the right atrioventricular sulcus. When the RCA reaches the acute margin of the heart, it turns to continue posteriorly in the sulcus onto the diaphragmatic surface and base of the heart.
Single-plane anatomical diagram of the structure of the coronary arterial tree and the cardiac complex. A - left coronary artery (LCA) system, B: right coronary artery (RCA) system.
1 - first facial sinus of the aorta, 2 - second facial sinus of the aorta.
A - aorta, LA - pulmonary artery, ASA - right atrial appendage, LAA - left atrial appendage, LAD - anterior interventricular branch, OB - circumflex branch, DV - diagonal branch, VTK - obtuse edge branch, ASU - sinus node artery, CA - conal artery, BOK - branch of the acute edge, a.AVU - artery of the atrioventricular node, ZAMV - posterior interventricular branch. Source: Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries.
M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003. CA – conal artery (branch of the conus arteriosus). Conus branch, infundibular branch, conus arteriosus branch.
The conus artery is the first major branch of the right coronary artery, but it can arise as an independent orifice from the 1st facial sinus of the aorta. The conus artery supplies the conus arteriosus and the anterior wall of the right ventricle and may participate in the blood supply to the anterior interventricular septum.
The artery has a variable distribution, but usually supplies a region of the anterior interventricular septum and the cone of the main pulmonary artery (hence its name). Although an acute occlusion of the tiny artery has been shown to result in ST elevation, another more important role it serves in pathophysiology is that of a route of collateral circulation. The conus artery has been shown to collateralise with the more distal acute marginal branch in RCA stenosis/obstruction, and collateralise with the left anterior descending artery (LAD) in LAD stenosis/obstruction, providing a potentially vital collateral pathway.
ASU – artery of the sinus node (branch of the sinus node, artery of the sinoatrial node (a.SNA), branch of the sinoatrial node). Sinoatrial nodal artery (SANa), sinus node artery, sinoatrial nodal branch, SA nodal artery, right SA node branch.
The sinus node artery is the main artery providing blood supply to the sinoatrial node, and its damage leads to irreversible disturbances in heart rhythm. The ASU is also involved in the blood supply to most of the interatrial septum and the anterior wall of the right atrium.
The artery of the sinus node, as a rule, arises from the dominant artery (see types of blood supply to the heart). With the right type of blood supply to the heart (in approximately 60% of cases), the ASU is the second branch of the right coronary artery and departs from the RCA opposite the origin of the conus artery, but can also arise from the 1st facial sinus independently. With the left type of blood supply to the heart, the artery of the sinus node arises from the circumflex branch of the left artery.
The sinoatrial nodal artery (SANa) supplies blood to the sinoatrial node (SAN), Bachmann's bundle, crista terminalis, and the left and right atrial free walls. The SANA most frequently originates from either the right coronary artery (RCA) or the left circumflex branch (LCX) of the left coronary artery (LCA).
Kugel's artery (great auricular artery). Kugel's artery, atrial anastomotic branch, Kugel's anastomotic branch (Lat.: arteria auricularis magna, arteria anastomotica auricularis magna, ramus atrialis anastomoticus).
Kugel's artery is an anastomosing between the systems of the right and left coronary arteries. In 66% of cases, it is a branch of the LCA or the SPU artery arising from it, in 26% - a branch of both coronary arteries or the SPU artery, arising from them simultaneously, and in 8% of cases - a branch of smaller branches arising from the right and left coronary arteries arteries to the atria.
ADVa. – adventitial artery.
The third branch of the PCA. The adventitial artery can be a branch of the conus artery or arise independently from the aorta. It goes up and to the right and lies on the anterior wall of the aorta (above the sinotubular junction), heading to the left and disappearing into the fatty sheath surrounding the great vessels.
AOK - artery of the acute edge (right marginal artery, right marginal branch, branch of the acute edge). Acute marginal artery, right marginal branch, right marginal artery.
The acute margin artery is one of the largest branches of the RCA. It descends from the RCA along the sharp right edge of the heart and forms powerful anastomoses with the LAD. Participates in nutrition of the anterior and posterior surfaces of the acute edge of the heart.
a.PVH - artery of the atrioventricular node (artery of the atrioventricular node). AV node artery, AV nodal artery (branch), AVN artery.
The artery (branch) of the atrioventricular node arises from the RCA in the area of the cross of the heart.
Posterior interventricular branch, posterior interventricular artery, posterior descending artery. Posterior descending artery (PDA), posterior interventricular artery (PIA).
The posterior interventricular branch can be a direct continuation of the RCA, but is more often a branch of it. It passes in the posterior interventricular groove, where it gives off posterior septal branches, which anastomose with the septal branches of the LAD and supply the terminal sections of the conduction system of the heart. With the left type of blood supply to the heart, the LAD receives blood from the left coronary artery, departing from the circumflex branch or LAD.
Posterior septal branches, inferior septal (septal) branches. Posterior septal perforators, posterior septal (perforating) branches.
The posterior (“lower”) septal branches arise from the LAD in the posterior interventricular groove, which anastomose with the “anterior” septal (septal) branches of the LAD and supply the terminal sections of the conduction system of the heart.
Posterolateral branch of the left ventricle (posterolateral left ventricular branch). Right posterolateral artery, posterolateral artery (PLA), posterior left ventricular (PLV) artery.
In approximately 20% of cases, the RCA forms the posterolateral branch of the left ventricle.
Left coronary artery and its branches
LCA – left coronary artery (LCA – left coronary artery, OS LCA – main trunk of the left coronary artery, trunk of the left coronary artery, main trunk of the left coronary artery).
Left coronary artery (LCA), left main coronary artery (LMCA), main stem of the left coronary artery, left main stem. As a rule, the left coronary artery arises with one trunk from the left (2nd facial) sinus of the aorta. The left artery trunk is usually short and rarely exceeds 1.0 cm, bends around the pulmonary trunk from behind, and at the level of the nonfacial sinus of the pulmonary artery is divided into branches, usually two: LAD and OB. In 40-45% of cases, the LCA, even before dividing into the LAD and OB, can give off the artery that supplies the sinus node. This artery can also arise from the OB of the LCA. The LMCA typically originates from the left sinus of Valsalva (LSV), passes between the right ventricle outflow tract and the left auricle and quickly bifurcates into the LAD and the LCX arteries. Its normal length varies from 2 mm to 4 cm.
Trunk of the left coronary artery - division into LAD and OB
Source: Coronary anatomy and anomalies.
Robin Smithuis and Tineke Willems. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. LAD – anterior interventricular branch (anterior descending artery, left anterior descending artery, left anterior interventricular artery). Left anterior descending artery (LAD), anterior interventricular artery (AIA), anterior descending coronary artery.
The anterior interventricular branch arises from the left artery trunk and follows down along the anterior interventricular septum. In 80% of cases, it reaches the apex and, going around it, moves to the back surface of the heart.
Right ventricular branch
The right ventricular branch is a non-permanent branch of the LAD and arises from the LAD on the anterior surface of the heart.
Septal branches of the LAD (septal branches of the LAD, “anterior” septal branches). Septal perforators, the septal branches (arteries), the septal perforator branches, perforator branches.
The septal branches of the LAD vary greatly in size, number, and distribution. The large first septal branch of the LAD (also known as the anterior septal branch, anterior septal artery, 1st SV) supplies the anterior part of the interventricular septum and participates in the blood supply to the conduction system of the heart. The remaining septal branches of the LAD (“anterior”) are usually smaller in size. They communicate with similar septal branches of the cervical vein (“lower” septal branches).
Diagonal branch of the LAD (DV - diagonal branches, diagonal arteries). Diagonal arteries (DB - diagonal branches), the diagonals.
Diagonal branches arise from the LAD and follow along the anterolateral surface of the left ventricle. There are several of them, designated by numbers from top to bottom: 1st, 2nd, 3rd diagonal arteries (branches). They supply blood to the anterior part of the left ventricle. The first diagonal branch is usually one of those branches that feeds the apex.
Median artery (intermediate branch) Intermediate artery, intermediate branch, ramus intermedius (RI), median (intermedian) branch.
In approximately 20-40% of cases, the LMCA trunk is divided not into two, but into three branches: the “diagonal branch” departs from the LMCA trunk along with the OB and LAD, and in this case it is called the median artery. The median artery is the equivalent of the diagonal branch and supplies the free wall of the left ventricle.
The ramus intermedius (RI) is an artery arising between the left anterior descending artery (LAD) and the CX. Some call it a high diagonal (D) or a high obtuse marginal (OM) artery.
In this normal variant, the LMCA can trifurcate into a LAD, a LCX and a ramus intermedius. The ramus intermedius typically supplies the lateral and inferior walls, acting as a diagonal or obtuse marginal branch, while the arteries that usually supply this territory are small or absent.
Median artery
Source: Coronary anatomy and anomalies.
Robin Smithuis and Tineke Willems. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. OB – circumflex branch of the left coronary artery, circumflex artery. Left circumflex coronary artery (LCX), circumflex artery (CX, CA).
The circumflex branch is a large branch of the LMCA; in some cases it can branch off from the left aortic sinus independently. It follows along the left atrioventricular groove, goes around the mitral valve, the left (obtuse) edge of the heart, and passes to its diaphragmatic surface. Typically, the OB gives off the left fragment of the Kugel artery, and although more often it does not reach the sinus node, in 10-12% of cases the artery of the sinus node can be formed by this branch.
VTK - branch of the obtuse edge (left marginal (marginal) branch, artery of the obtuse edge). Obtuse marginal artery, the obtuse marginals, the obtuse marginal (OM) branch, the left marginal arteries.
The obtuse margin branch is the largest branch of the OB and can arise both from the beginning of the OB and at the level of the obtuse margin. This is a very important branch involved in feeding the free wall (its anterior and posterior surfaces) of the LV along its lateral edge. Very often, the OM system is generally represented by a large VTK and unexpressed OM. There can be several branches of the obtuse edge, then they are designated by numbers as they extend from left to right: 1st, 2nd, 3rd.
Left atrial branch.
The left atrial branch may arise from the OB. It nourishes the lateral and posterior surface of the left atrium.
Posterolateral branch (left ventricular branch). Posterolateral branch (PLB).
The posterolateral branch is most often the terminal branch of the OB, but the origin of this branch, as well as the LMVA and the artery of the atrioventricular node from the OB LCA, is determined by the dominance of the right or left coronary artery.
Anatomy
The right coronary artery begins in the anterior internal sinus of the aortic bulb. Departing from the anterior surface of the aorta, the PVA is located on the right side of the coronary sulcus, approaches the sharp edge of the heart, goes around it and goes to the intersection and then to the posterior interventricular sulcus. At the intersection of the posterior interventricular and coronary grooves (crossing), the PVA gives off the posterior interventricular branch, which goes to the distal part of the anterior interventricular branch, anastomosing with it. Rarely does PVA end at the sharp edge of the heart.
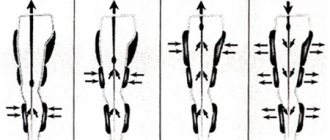
Types of blood supply to the heart Type of dominance (Coronary dominance)
The myocardial distribution of the coronary arteries is somewhat variable, but the right coronary artery (RCA) almost always supplies the right ventricle (RV), and the left coronary artery (LCA) supplies the anterior portion of the ventricular septum and anterior wall of the left ventricle (LV). The vessels that supply the remainder of the LV vary depending on the coronary dominance. Read More: https://www.ajronline.org/doi/10.2214/AJR.06.1295
The posterior descending artery (PDA) runs in the posterior interventricular groove and supplies the inferior wall and inferior third of the interventricular septum. The artery that supplies the PDA and a posterolateral branch determines the coronary dominance, so there can be three situations:
Right type of blood supply to the heart. Right dominant heart, RCA dominance, right-dominance, right dominant circulation.
Most hearts (approximately 70% of cases) are right dominant where the posterior descending artery (PDA) and the posterolateral branch are supplied by the right coronary artery (RCA). In this instance, the RCA supplies the inferoseptal and inferior segments of the left ventricle.
Left type of blood supply to the heart. Left dominant heart, LCA dominance, left dominant circulation.
In 10% of cases the PDA is supplied by the LAD or LCx.
Mixed type of blood supply to the heart. Codominant heart, codominance.
In 20% of cases a single or duplicated PDA and posterolateral branches are supplied by branches of both the RCA and LAD/LCx.
Dominant right coronary artery and its branches.
Right type of blood supply to the heart. Schematic structure of the right coronary artery (antero-posterior projection). AV = atrioventricular, PDA = posterior descending artery, RCA = right coronary artery, RV = right ventricular, SA = sinoatrial.
Dominant left coronary artery and its branches.
Schematic structure of the left coronary artery with the left type of blood supply to the heart (left anterior oblique projection).
AVGA = atrioventricular groove artery, PDA = posterior descending artery. Source: Sunil Kini, Kostaki G. Bis, and Leroy Weaver. Normal and Variant Coronary Arterial and Venous Anatomy on High-Resolution CT Angiography. American Journal of Roentgenology 2007 188:6, 1665-1674.
Literature and Internet resources:
- Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries. M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003. + 297 pp., illustration.
- Nerantzis, C. E., Marianou, S. K., Koulouris, S. N., Agapitos, E. B., Papaioannou, J. A., & Vlahos, L. J. (2004). Kugel's artery: an anatomical and angiographic study using a new technique. Texas Heart Institute journal, 31(3), 267–270.
- Vikse, J., Henry, B. M., Roy, J., Ramakrishnan, P. K., Hsieh, W. C., Walocha, J. A., & Tomaszewski, K. A. (2016). Anatomical Variations in the Sinoatrial Nodal Artery: A Meta-Analysis and Clinical Considerations. PloS one, 11(2), e0148331. doi:10.1371/journal.pone.0148331.
- Rahalkar, A. M., & Rahalkar, M. D. (2009). Pictorial essay: Coronary artery variants and anomalies. The Indian journal of radiology & imaging, 19(1), 49–53. doi:10.4103/0971-3026.45345.
- Villa, A. D., Sammut, E., Nair, A., Rajani, R., Bonamini, R., & Chiribiri, A. (2016). Coronary artery anomalies overview: The normal and the abnormal. World journal of radiology, 8(6), 537–555. doi:10.4329/wjr.v8.i6.537.
- Sunil Kini, Kostaki G. Bis, and Leroy Weaver. Normal and Variant Coronary Arterial and Venous Anatomy on High-Resolution CT Angiography. American Journal of Roentgenology 2007 188:6, 1665-1674
- Siew Yen Ho. Structure and anatomy of the aortic root. European Journal of Echocardiography, Volume 10, Issue 1, January 2009, Pages i3–i10.
- radiopaedia.org
- Robin Smithuis and Tineke Willems. Coronary anatomy and anomalies. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. www.radiologyassistant.nl
Copyright © 2008-2019 Medtran.ru. All rights reserved.
Coronary angiography
Physiological basis
The first-year university program includes studying the structure of the heart and its coronary vessels. But most often, textbook authors limit themselves to describing only large vessels. Clinicians use a completely different, but also international, nomenclature. Coronary angiography and stent implantation require a more detailed description of the heart vessels, which has found application in international practice.
From the anatomy course, everyone learned that two arteries depart from the aorta that supply blood to the heart itself: the left and right coronary arteries. The thickenings at the root of the aorta, from which these arteries emerge, are called the left and right coronary sinuses, respectively.
The following parts of the left coronary artery (LCA, left coronary artery) are distinguished: main trunk , which is divided into the anterior interventricular branch (ramus interventricularis anterior, RIVA or left anterior descending, LAD), as well as the circumflex artery (left circumflex coronary artery, LCx). The main trunk of this artery rarely exceeds 1 cm in length, and is then divided into its two terminal branches. The anterior interventricular branch is located on the anterior surface of the heart up to its apex. Along its length, the anterior ventricular branches (diagonal branches, RD/R.Diag) and anterior septal branches depart from this artery. In coronary angiography, for the purpose of topical indication of the location of the lesion, it is proposed to divide the coronary bed into segments. The proximal segment of the LAD begins with its branch from the trunk and continues to the point where the first septal or first RD departs from it, the middle part - to the branch of the second septal branch or the second RD, the distal part - to the apex of the heart / after the departure of the second RD.
The circumflex artery is always located on the posterior surface of the heart. In its proximal part, a branch of the obtuse edge (obtuse marginal artery, obtuse marginal branch, OMB) departs from it. Depending on the location of this branch, the proximal and distal parts of the circumflex branch are distinguished. Very rarely, another branch departs from the main trunk between the anterior interventricular branch and the circumflex branch in the middle, originating directly from the common trunk - the intermediate artery (RIM, ramus intermedius).
The following three parts of the right coronary artery (RCA) are distinguished: proximal (from the mouth to its first turn, usually located horizontally), middle (from the first to the second turn) and distal (after its second turn until the artery divides into branches at the “cross” of the heart (crux cordis) - the intersection of the posterior interventricular and atrioventricular grooves of the heart). Sometimes, immediately after the mouth itself, a small branch departs from the vessel - the branch of the conus arteriosus (ramus coni arteriosi, CB), as well as many small branches to the right atrium. The most important of these branches is the artery of the sinoatrial node (SA node artery, SNA). It is often located under the right ear of the heart. In rare cases, the branch of the conus arteriosus has its own orifice. This option should always be considered, since coronary angiography may mistake this artery for the main trunk of the right coronary artery. By blocking the entrance to this artery with a catheter, it is possible to cause local ischemia and, as a consequence, rhythm disturbances up to the flutter of the heart chambers. In the anterior part of the coronary sulcus, in the region of the acute edge of the heart, a branch of the acute edge (acute marginal artery, AMB), usually from one to three, departs from the right coronary artery, usually from one to three, which in most cases reaches the apex of the heart.
So, let's list all the abbreviations again:
Left coronary artery - left coronary artery (LCA): - Anterior interventricular branch (LAD), or anterior descending artery - left anterior descending artery (LAD); otherwise - ramus interventricularis anterior (RIVA/RIA); — Diagonal arteries (branches) — YES; ramus diagonalis (RD/Diag); - Circumflex branch (OB) of the left coronary artery, circumflex artery - left circumflex coronary artery (LCx)); - Branch of the obtuse edge, obtuse marginal artery, obtuse marginal branch, (OMB); - Septal interventricular branches, ramus septalis (RSA); — Intermediate artery, ramus intermedius (RIM).
Right coronary artery - right coronary artery (RCA): - Branch of the acute edge, acute marginal artery, (AMB); - Artery of the sinoatrial node - ramus nodi sinuatrialis (SA node artery, SNASA/RNS); — Posterior interventricular branch (ZMZHV), or posterior descending artery (PDA); otherwise - ramus interventricularis posterior (RIVP/RIP).
And once again for repetition (an important task for diagnosing the localization of ischemia during myocardial infarction): LAD/RIVA , LCx supplies the left chamber with blood from the front and side, and RCA from the back. The left atrium is supplied with blood by LCx, RCA . Partition - RSA from LAD . Right camera at the back - RCA , at the front - RCA, LAD . Right atrium - RCA .
It should also be recalled about the dominance of the blood supply to the myocardium. In the so-called right heart, which occurs in 70% of people, the posterior descending artery (PDA) arises from the right coronary artery. In left-sided hearts (10% of people), the circumflex artery (LCx) reaches the level of the posterior interventricular groove and forms the posterior descending artery (PDA). In the even rarer, so-called mixed codominant type (20% of people), there are two posterior ventricular branches (RIVP/RIP) arising from the right coronary and circumflex arteries.
To understand the principle of operation of the ECG, it is necessary to repeat the structure of the conduction system of the heart. The sinoatrial node is located in the wall of the right atrium, its impulses travel to the atrioventricular node (also located in the wall of the right atrium). Next, the impulse propagates along the fibers of the His bundle, which is divided in the interventricular septum into two legs - right and left (sometimes called the legs of Tavara). The signal reaches the endocardium via Purkinje fibers. Sometimes there are additional pathways for the transmission of excitation, as, for example, through Kent fibers. Such pathways are often located between the atria and ventricles and bypass the atrioventricular node. Because of this, the myocardial muscles often contract prematurely, which becomes noticeable on the ECG, and such patients are predisposed to tachycardia (WPW syndrome).
An electrocardiogram is nothing more than a recording of the propagated electrical potentials of the heart, recorded by electrodes on the limbs and chest wall. The ECG includes three standard Einthoven leads (I, II, III), and three enhanced Goldberg leads (aVR, aVL, aVF). Attaching six more chest electrodes according to Wilson (V1-V6) allows you to record the spread of excitation along the heart wall in a horizontal projection. Depending on the changes in these leads, even at the prehospital stage, using an ECG, it is possible to suggest the localization of the infarction and a possible “problem” artery.
For example, with a heart attack of the right side of the heart (the back wall), the right ventricle is often particularly severely affected. Most often this occurs due to a blood clot in the RCA. The right side of the heart is unable to contract properly, resulting in decreased preload of the left chamber of the heart because it reduces the volume of blood transported to the left atrium. The heart tries to compensate for the reduced cardiac output by increasing the contraction rate. With a heart attack of the left side of the heart, the main complication is cardiogenic shock.
Especially for our subscribers, we have made a table that shows ECG changes depending on the location of possible damage to the coronary arteries.
It is also worth repeating the classification of acute coronary syndromes:
- Unstable angina without troponin elevation . This form is classified according to Braunwald into 3 classes depending on the severity of clinical signs:
I - recent chest pain (less than 2 months, more than 3 times a day); II - pain behind the sternum at rest (at least once in the past month, but not within the last 48 hours); III - chest pain at rest (at least once in the last 48 hours). Unstable angina is classified into 3 groups according to the causes of occurrence: A - secondary unstable angina (myocardial infarction, anemia, fever, hypotension, tachyarrhythmia, thyrotoxicosis, respiratory failure); B - primary unstable angina; C - unstable angina after a heart attack (at least 2 weeks after a heart attack).
- Myocardial infarction without ST segment elevation (NSTEMI) with an increase in the concentration of cardiac troponin in the blood.
- ST segment elevation myocardial infarction
PBCA and stenting
Sones, back in 1959, described a method that allows one to assess the condition of individual coronary vessels. Judkins modified the described method in 1967. It is this method of studying the coronary vessels that is still used today. The first transluminal balloon coronary angioplasty (TBCA) was performed on September 16, 1977 in Zurich in Switzerland. Since then, the number of ACS patients undergoing TBCA has increased from 10 to 65%. According to the latest data, recently published in The Lancet, deaths due to cardiovascular disease in 2010 fell by a quarter compared with 1950, when 400 out of 100,000 cases were fatal. The first patient was a 38-year-old male smoker who presented with LAD stenosis. After the operation, the man lived another 37 years.
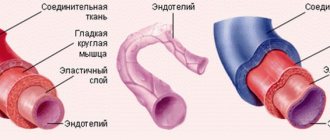
With PBCA, a balloon catheter is inserted using a guidewire up to the site of stenosis. The balloon inflates and thereby “flats” atherosclerotic plaques, stretching the vascular wall. Minor intimal injuries during balloon inflation often have no consequences, but sometimes it is in these places that tissue proliferation later begins, which in 30–40% of cases leads to restenosis and relapses over the next three months. The frequency of emergency operations to create bypasses is less than 0.5%. By implanting a stent, the vascular wall is stabilized. There was also a primary stenting technique - implantation of a stent without previous dilatation of the vessels with a balloon, but now it is used extremely rarely and only in the initial stages of narrowing the lumen of the vessel. Studies in recent years have shown that with significant narrowing of the lumen of the vessel, such patients experienced myocardial ischemia in the first hours after angioplasty, which required immediate re-surgical intervention or re-dilatation. This complication occurs due to plaque detachment from the endothelium. Exposure of the surface of smooth muscle cells leads to thrombosis due to the release of collagen molecules and tissue factors that trigger the blood clotting cascade. To avoid the development of blood clots and restenosis, angioplasty is now most often combined with the implantation of stents at the site of stenosis.
The first stent implantation was performed by Sigwart in 1987. Then the stents were mounted directly on the balloon by the doctor himself. Now the entire structure is included, which has reduced the risk of stent loss in the bloodstream if it is not sufficiently fixed.