Physiological basis
The first-year university program includes studying the structure of the heart and its coronary vessels. But most often, textbook authors limit themselves to describing only large vessels. Clinicians use a completely different, but also international, nomenclature. Coronary angiography and stent implantation require a more detailed description of the heart vessels, which has found application in international practice.
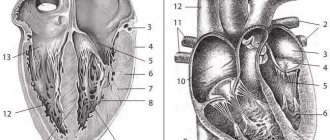
From the anatomy course, everyone learned that two arteries depart from the aorta that supply blood to the heart itself: the left and right coronary arteries. The thickenings at the root of the aorta, from which these arteries emerge, are called the left and right coronary sinuses, respectively.
The following parts of the left coronary artery (LCA, left coronary artery) are distinguished: the main trunk , which is divided into the anterior interventricular branch (ramus interventricularis anterior, RIVA or left anterior descending, LAD), as well as the circumflex artery (left circumflex coronary artery, LCx) .
The main trunk of this artery rarely exceeds 1 cm in length, and is then divided into its two terminal branches. The anterior interventricular branch is located on the anterior surface of the heart up to its apex. Along its length, the anterior ventricular branches (diagonal branches, RD/R.Diag) and anterior septal branches depart from this artery. In coronary angiography, for the purpose of topical indication of the location of the lesion, it is proposed to divide the coronary bed into segments.
The proximal segment of the LAD begins with its branch from the trunk and continues to the point where the first septal or first RD departs from it, the middle part - to the branch of the second septal branch or the second RD, the distal part - to the apex of the heart / after the departure of the second RD.
- The circumflex artery is always located on the posterior surface of the heart. In its proximal part, a branch of the obtuse edge (obtuse marginal artery, obtuse marginal branch, OMB) departs from it. Depending on the location of this branch, the proximal and distal parts of the circumflex branch are distinguished. Very rarely, another branch departs from the main trunk between the anterior interventricular branch and the circumflex branch in the middle, originating directly from the common trunk - the intermediate artery (RIM, ramus intermedius).
The three parts of the right coronary artery (RCA) are distinguished: - proximal (from the mouth to its first turn, usually located horizontally),
- middle (from the first to the second turn) and
- distal (after its second turn until the artery divides into branches at the “cross” of the heart (crux cordis) - the intersection of the posterior interventricular and atrioventricular grooves of the heart).
Sometimes, immediately after the mouth itself, a small branch departs from the vessel - the branch of the conus arteriosus (ramus coni arteriosi, CB), as well as many small branches to the right atrium.
The most important of these branches is the artery of the sinoatrial node (SA node artery, SNA). It is often located under the right ear of the heart. In rare cases, the branch of the conus arteriosus has its own orifice. This option should always be considered, since coronary angiography may mistake this artery for the main trunk of the right coronary artery. By blocking the entrance to this artery with a catheter, it is possible to cause local ischemia and, as a consequence, rhythm disturbances up to the flutter of the heart chambers. In the anterior part of the coronary sulcus, in the region of the acute edge of the heart, a branch of the acute edge (acute marginal artery, AMB), usually from one to three, departs from the right coronary artery, usually from one to three, which in most cases reaches the apex of the heart.
So, let's list all the abbreviations again:
Left coronary artery - left coronary artery (LCA): - Anterior interventricular branch (LAD), or anterior descending artery - left anterior descending artery (LAD); otherwise - ramus interventricularis anterior (RIVA/RIA); — Diagonal arteries (branches) — YES; ramus diagonalis (RD/Diag); - Circumflex branch (OB) of the left coronary artery, circumflex artery - left circumflex coronary artery (LCx)); - Branch of the obtuse edge, obtuse marginal artery, obtuse marginal branch, (OMB); - Septal interventricular branches, ramus septalis (RSA); — Intermediate artery, ramus intermedius (RIM).
Right coronary artery - right coronary artery (RCA): - Branch of the acute edge, acute marginal artery, (AMB); - Artery of the sinoatrial node - ramus nodi sinuatrialis (SA node artery, SNASA/RNS); — Posterior interventricular branch (ZMZHV), or posterior descending artery (PDA); otherwise - ramus interventricularis posterior (RIVP/RIP).
And once again for repetition (an important task for diagnosing the localization of ischemia during myocardial infarction): LAD/RIVA, LCx supplies blood to the left chamber from the front and side, and RCA from the back. The left atrium is supplied by LCx, RCA. The partition is RSA from LAD. Right camera at the back - RCA, at the front - RCA, LAD. Right atrium - RCA.
It should also be recalled about the dominance of the blood supply to the myocardium. In the so-called right heart, which occurs in 70% of people, the posterior descending artery (PDA) arises from the right coronary artery. In left-sided hearts (10% of people), the circumflex artery (LCx) reaches the level of the posterior interventricular groove and forms the posterior descending artery (PDA). In the even rarer, so-called mixed codominant type (20% of people), there are two posterior ventricular branches (RIVP/RIP) arising from the right coronary and circumflex arteries.
To understand the principle of operation of the ECG, it is necessary to repeat the structure of the conduction system of the heart. The sinoatrial node is located in the wall of the right atrium, its impulses travel to the atrioventricular node (also located in the wall of the right atrium). Next, the impulse propagates along the fibers of the His bundle, which is divided in the interventricular septum into two legs - right and left (sometimes called the legs of Tavara). The signal reaches the endocardium via Purkinje fibers. Sometimes there are additional pathways for the transmission of excitation, as, for example, through Kent fibers. Such pathways are often located between the atria and ventricles and bypass the atrioventricular node. Because of this, the myocardial muscles often contract prematurely, which becomes noticeable on the ECG, and such patients are predisposed to tachycardia (WPW syndrome).
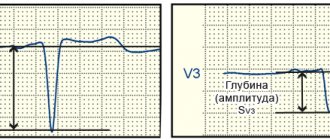
An electrocardiogram is nothing more than a recording of the propagated electrical potentials of the heart, recorded by electrodes on the limbs and chest wall. The ECG includes three standard Einthoven leads (I, II, III), and three enhanced Goldberg leads (aVR, aVL, aVF). Attaching six more chest electrodes according to Wilson (V1-V6) allows you to record the spread of excitation along the heart wall in a horizontal projection. Depending on the changes in these leads, even at the prehospital stage, using an ECG, it is possible to suggest the localization of the infarction and a possible “problem” artery.
For example, with a heart attack of the right side of the heart (the back wall), the right ventricle is often particularly severely affected. Most often this occurs due to a blood clot in the RCA. The right side of the heart is unable to contract properly, resulting in decreased preload of the left chamber of the heart because it reduces the volume of blood transported to the left atrium. The heart tries to compensate for the reduced cardiac output by increasing the contraction rate. With a heart attack of the left side of the heart, the main complication is cardiogenic shock.
Especially for our subscribers, we have made a table that shows ECG changes depending on the location of possible damage to the coronary arteries.
It is also worth repeating the classification of acute coronary syndromes:
Unstable angina without troponin elevation. This form is classified according to Braunwald into 3 classes depending on the severity of clinical signs: I - recent chest pain (less than 2 months, more than 3 times a day); II - pain behind the sternum at rest (at least once in the past month, but not within the last 48 hours); III - chest pain at rest (at least once in the last 48 hours).
Unstable angina is classified into 3 groups according to the causes of occurrence: A - secondary unstable angina (myocardial infarction, anemia, fever, hypotension, tachyarrhythmia, thyrotoxicosis, respiratory failure); B - primary unstable angina; C - unstable angina after a heart attack (at least 2 weeks after a heart attack).
Myocardial infarction without ST segment elevation (NSTEMI) with an increase in the concentration of cardiac troponin in the blood. ST segment elevation myocardial infarction (STEMI) with increased cardiac troponin concentrations in the blood.
Types of myocardial blood circulation
Based on the blood supply to the posterior wall of the heart, balanced, left and right types of blood circulation are distinguished. Determination of the predominant type depends on whether one of the arteries reaches the avascular area, which was formed as a result of the intersection of two grooves - the coronary and interventricular. One of the arteries reaching this area gives off a branch that passes to the apex of the organ.
Consequently, the predominant right type of blood circulation of the organ is provided by the right artery, which has a structure in the form of a large trunk, while the circumflex artery to this area is poorly developed.
The predominance of the left type, accordingly, implies the predominant development of the left artery, which goes around the root of the heart and provides blood supply to the organ. In this case, the diameter of the right artery is quite small, and the vessel itself reaches only the middle of the right ventricle.
The balanced type involves uniform blood flow to the above-mentioned area of the heart through both arteries.
PBCA and stenting
Sones, back in 1959, described a method that allows one to assess the condition of individual coronary vessels. Judkins modified the described method in 1967. It is this method of studying the coronary vessels that is still used today. The first transluminal balloon coronary angioplasty (TBCA) was performed on September 16, 1977 in Zurich in Switzerland. Since then, the number of ACS patients undergoing TBCA has increased from 10 to 65%. According to the latest data, recently published in The Lancet, deaths due to cardiovascular disease in 2010 fell by a quarter compared with 1950, when 400 out of 100,000 cases were fatal. The first patient was a 38-year-old male smoker who presented with LAD stenosis. After the operation, the man lived another 37 years.
With PBCA, a balloon catheter is inserted using a guidewire up to the site of stenosis. The balloon inflates and thereby “flats” atherosclerotic plaques, stretching the vascular wall. Minor intimal injuries during balloon inflation often have no consequences, but sometimes it is in these places that tissue proliferation later begins, which in 30–40% of cases leads to restenosis and relapses over the next three months. The frequency of emergency operations to create bypasses is less than 0.5%. By implanting a stent, the vascular wall is stabilized. There was also a primary stenting technique - implantation of a stent without previous dilatation of the vessels with a balloon, but now it is used extremely rarely and only in the initial stages of narrowing the lumen of the vessel. Studies in recent years have shown that with significant narrowing of the lumen of the vessel, such patients experienced myocardial ischemia in the first hours after angioplasty, which required immediate re-surgical intervention or re-dilatation. This complication occurs due to plaque detachment from the endothelium. Exposure of the surface of smooth muscle cells leads to thrombosis due to the release of collagen molecules and tissue factors that trigger the blood clotting cascade. To avoid the development of blood clots and restenosis, angioplasty is now most often combined with the implantation of stents at the site of stenosis.
The first stent implantation was performed by Sigwart in 1987. Then the stents were mounted directly on the balloon by the doctor himself. Now the entire structure is included, which has reduced the risk of stent loss in the bloodstream if it is not sufficiently fixed.
New types of cylinders themselves have also appeared. Some of them have cutting teeth on their surface that are located parallel to the axis of the vessel, as well as cylinders made of nitinol and nylon that are helical or parallel to the axis of the vessel. These designs make it possible to create an ideal site for implantation of a future stent. At first, during the research process, scientists did not notice a difference between such cylinders and standard ones, but recently it turned out that such notched cylinders coated with drugs show better results.
There are two types of metallic stents : self-expanding and balloon-mounted. Studies show that the use of the first type of stents more often causes the development of neointimal hyperplasia. Therefore, the second type of stent is now often used. Typically, they consist of a metal tube in which holes are created using various techniques. After dilating the vessel with a balloon catheter, a network is created in its lumen, enveloping its walls from the inside. The prototype of this type of stent was the Palmaz-Schatz stent, which is no longer used.
A 1994 study showed no difference between implantation of such a stent and conventional angioplasty. The development of this direction has made it possible to develop new types of stents. Most often they consist of several modules connected by connectors. Initially, they were made from steel, but now platinum, cobalt, nitinol (nickel-titanium), and also only titanium are used as materials for the manufacture of stents. Because of this, they have become significantly smaller and lighter. RCTs have shown the advantages of stents with thick frames over those with thin frames. It is assumed that they injure the vessels less, thus preventing re-endothelialization.
There are also stents with a special coating that creates a blood-impermeable barrier. These substances include polytetrafluoroethylene and polyethylene. They were first used for the emergency closure of small perforations of the coronary arteries, but are now used in the prevention of coronary aneurysms and arteriovenous fistulas.
Drug-eluting-stents (DES) are coated with special substances that inhibit the proliferation of endothelial cells, thus preventing vessel restenosis, which most often develops within 4-8 months after implantation.
Ferromagnetic stents that are tightly installed in the vascular bed are not a contraindication for MRI.
There are special stents for positioning them in the mouths and branches of blood vessels. Like any foreign object in the bloodstream, stents are an additional factor in thrombus formation. Therefore, after the procedure itself, the patient is always prescribed DAAT or TAT.
Coronary angiography
Coronary angiography (coronary angiography) is x-ray visualization of the coronary vessels after the injection of a radiopaque contrast agent. The X-ray image is simultaneously recorded on 35 mm film or digital media for subsequent analysis. At the moment, coronary angiography is the “gold standard” for determining the presence or absence of stenoses in coronary disease. The purpose of coronary angiography is to determine the coronary anatomy and the degree of narrowing of the lumen of the coronary arteries. Information obtained during the procedure includes determination of the location, extent, diameter and contours of the coronary arteries, the presence and degree of coronary obstruction, characterization of the nature of the obstruction (including the presence of atherosclerotic plaque, thrombus, dissection, spasm or myocardial bridge). The data obtained determine the further tactics of treating the patient: coronary bypass surgery, intervention, drug therapy. To conduct high-quality angiography, selective catheterization of the right and left coronary arteries is necessary, for which a large variety of diagnostic catheters of various modifications have been created. The examination is carried out under local anesthesia and NLA through arterial access. The following arterial approaches are generally accepted: femoral arteries, brachial arteries, radial arteries. Transradial access has recently gained a strong position and has become widely used due to its low morbidity and convenience. After puncture of the artery, diagnostic catheters are inserted through the introducer, followed by selective catheterization of the coronary vessels. The contrast agent is administered in doses using an automatic injector. Filming is performed in standard projections, the catheters and intravener are removed, and a compression bandage is applied.
Brachytherapy
This method is based on radioactive irradiation of the coronary arteries during relapses after implantation of stents. Beta radiation is used for this, since it can penetrate only a few millimeters into the thickness of the tissue. In this method, a catheter is inserted into the site of the stenosis that was previously dilated with a balloon. Using this catheter, the area is irradiated with a calculated dose for a certain amount of time (3-5 minutes). Vascular brachytherapy has been used since 1996. In February 2005, the company developing devices for brachytherapy of coronary vessels (Beta-Cath-System) ceased to exist.
Rotablationplasty
This method has been used since 1989. A diamond bur is introduced into the vessel, capable of rotating at a frequency of 190,000 rpm. in a minute. It is used to remove tissue at the site of restenosis. The size of the crushed particles in this way is 5–10 micrometers (the length of a red blood cell is 7.5 micrometers). The resulting channel is very small in diameter, but sufficient for performing PTCA. As a rule, the method is used in case of formation of calcifications at the site of restenosis. The diameter of the bur head varies from 1.25 to 2.5 mm. Because the rotablation bur cable does not penetrate the stenosis site well, the success rate of the operation is 80–95%. Complications include vascular spasms, which occur more often (5%) than with PTCA.
Basic angiographic projections
When carrying out the procedure, the goal is to obtain the most complete information about the anatomy of the coronary arteries, their morphological characteristics, the presence of changes in the vessels with an accurate determination of the location and nature of the lesions. To achieve this goal, coronary angiography of the right and left coronary arteries is performed in standard projections. (They are described below). If it is necessary to conduct a more detailed study, shooting is carried out in special projections. This or that projection is optimal for analyzing a certain section of the coronary bed and allows the most accurate identification of morphological features and the presence of pathology of a given segment. Below are the main angiographic projections indicating the arteries for which these projections are optimal for visualization. For the left coronary artery, the following standard projections exist. 1. Right anterior oblique with caudal angulation. RAO 30, caudal 25. OV, VTK,
2. Right anterior oblique projection with cranial angulation. RAO 30, cranial 20 LAD, its septal and diagonal branches
3. Left anterior oblique with cranial angulation. LAO 60, cranial 20. The mouth and distal portion of the LCA trunk, the middle and distal segment of the LAD, septal and diagonal branches, the proximal segment of the OB, the VTK.
4. Left anterior oblique with caudal angulation (spider). LAO 60, caudal 25. LCA trunk and proximal segments of the LAD and OB.
5. To determine the anatomical relationships, a left lateral projection is performed. For the right coronary artery, surveys are performed in the following standard projections. 1. Left oblique projection without angulation. LAO 60, stright. Proximal and middle segment of the RCA, VOC.
2. Left oblique with cranial angulation. LAO 60, cranial 25. The middle segment of the RCA and the posterior descending artery.
3. Right oblique without angulation. RAO 30, stright. Middle segment of the RCA, branch of the conus arteriosus, posterior descending artery.
Professor, Doctor of Medicine. Sciences Yu.P. Ostrovsky
Intravascular ultrasound
Another tool for the cardiologist is the intravascular ultrasound (IVUS) method. An ultrasonic probe is inserted into the vessel. The procedure for manipulation is similar to that for PTCA: after positioning the guidewire, the probe is passed to the site of stenosis. Ultrasound allows you to view 1 mm of tissue at a distance from the emitter. A total of 64 of these crystals (piezoelectric elements) are used at the top of the catheter. Using this method, it is possible to determine the composition of plaques and their fibrin, lipid and calcium components. Most often, ultrasound is used when the angiographic picture is ambiguous, using it as an additional examination method.
We were all tormented in physiology with graphs of pressure in blood vessels. Few people in junior courses would have thought that these data were actually used in diagnostics. With each coronary angiography, the pressure in the coronary arteries and its changes depending on the presence of stenotic areas are examined. To do this, a detector with a diameter of 0.014 inches is brought to the area under study. This catheter is advanced to the very end of the coronary artery. Then they pull him back. This way the pressure is recorded throughout the artery. On the monitor, doctors observe changes in pressure; in the place of its greatest difference, the most stenotic area most often turns out to be. A gradual change in pressure is evidence of diffuse vascular disease. It is important to calibrate the detector prior to testing. After the application of adenosine, hyperemia is observed, that is, an increase in blood circulation, which simulates a state of stress. After this, the pressure throughout the vessel is measured again, which makes it possible to determine whether the places of stenosis are important and whether they cause pain in the patient during physical activity. The adenosine test is not safe: it is possible to develop heart rhythm disturbances, but due to the short half-life of adenosine, only for a short time.
How does IHD manifest itself?
Coronary heart disease develops against the background of damage to the internal walls of blood vessels, which provokes a decrease in their lumen and deterioration of blood circulation in the heart muscle. Insufficient supply of oxygen and nutrients leads to myocardial ischemia with the subsequent development of acute or chronic processes, most often in the form of a heart attack and angina attacks.
To provide timely medical care, it is important to recognize the early symptoms of an impending vascular accident and call an ambulance.
Clinical manifestations of myocardial infarction:
- the main symptom is severe pain in the chest, which can be reduced only after taking narcotic analgesics;
- in patients with diabetes mellitus there may be no pain;
- in some cases, patients feel discomfort in the chest area, accompanied by pain in the abdomen and shoulder blade;
- sticky sweat appears;
- some patients develop symptoms of heart failure (the frequency and depth of breathing is impaired, which complicates respiratory function, coughing attacks occur that do not bring relief);
- heart rate is disturbed.
Symptomatic complex of angina attacks:
- a feeling of discomfort or painful sensations of a pressing nature appears in the chest area;
- pain occurs after physical exertion, nervous strain, stressful situations and after eating;
- pain radiates to the left shoulder area, between the shoulder blades and neck;
- the duration of attacks does not exceed 15 minutes;
- the sensation of pain and discomfort is easily eliminated after taking nitroglycerin.
As a rule, people with coronary circulatory insufficiency suffer from ascites, enlarged liver and paroxysmal cough. For timely diagnosis of coronary artery disease, a coronary examination of the heart vessels is performed - selective coronary angiography, which makes it possible to accurately identify the nature, degree and location of the narrowing. When the disease is advanced, post-infarction cardiosclerosis develops and is diagnosed as a complication after a heart attack or as an independent form of coronary artery disease. According to medical reviews, with the help of coronary angiography of the heart vessels in case of cardiosclerosis, it is possible to determine the location of stenoses or occlusions, vascular aneurysms, and identify possible arterial thrombosis; Such consequences of coronary vessel pathologies are often incompatible with life.
Another serious condition is sudden coronary (cardiac) death , characterized by sudden cardiac arrest. The exact causes of acute pathology have not been identified; according to some medical hypotheses, cardiac arrest is associated with electrical conduction disorders.
Coronary vasospasm and acetylcholine test
Spasms of the coronary arteries are often the cause of chest pain at night in patients without visible changes in the coronary vessels. Such patients are also prescribed coronary angiography and the above provocation test is performed to exclude psychogenic or non-cardiac causes of such symptoms. Now every person who has already passed physiology should have a thought: “Why acetylcholine?” If you don't find the answer, you may need to open the textbook again. The fact is that the endothelium of the heart produces NO when acetylcholine is applied, which leads to vasodilation. Acetylcholine has a vasoconstrictor effect on vascular smooth muscle cells as a result of their direct stimulation if the endothelium is damaged. In this way, healthy endothelium can be distinguished from damaged endothelium. Healthy vessels respond to acetylcholine by dilating, while damaged ones narrow. When vasoconstriction is more than 75% compared to the intracoronary application of nitroglycerin, we speak of coronary spasm.
Sources:
- M. Winkhardt. Das Herzkatheterlabor (Einführung in die Aufgabenbereiche des kardiologischen Assistenzpersonals). Steinkopff Verlag Darmstadt, 2005.
- Byrne RA et al. Coronary balloon angioplasty, stents, and scaffolds //The Lancet. – 2021. – T. 390. – No. 10096. – pp. 781-792.
Translation into English of the names and abbreviations of the arteries of the heart
Serzhenko Nadezhda Medical translation agency "Medtran"
Translation of coronary angiography results raises many questions even for an experienced medical translator. The topic is quite difficult for a number of reasons:
- Complex anatomy of the coronary arteries
- A huge variety of anatomical options
- Abundance of terms and abbreviations
- Lack of a unified nomenclature
- Almost every artery has several synonymous names in both Russian and English
A standard situation for a medical translator is that it is necessary to translate an extract from the patient’s medical history, which contains a description of the results of coronary angiography, or, among other medical documents, there is a protocol for angiography of the coronary arteries. If the translator does not have experience in such translations, then two paragraphs of such text may take several hours.
Many translation problems arise due to synonyms (different variants of the names of the same artery). In order to correctly translate the variant name of an artery encountered in a medical history (which does not always have an unambiguous analogue in English), it is often necessary to search and compare the description of the anatomical structure in Russian with the description in English to make sure that the selected English term corresponds to the Russian name for the artery.
To avoid distortion of meaning when translating the names of anatomical formations and angiographic terms into English, we strongly recommend using analogues that are as close as possible to the Russian original. Despite the fact that the same artery may have several names in both Russian and English, the use of synonyms should be kept to a minimum, because this makes verification difficult and is a potential source of error. The translation of a medical text must convey the content of the source text as closely as possible, and the translator does not have the right to interpret the available information at his own discretion. However, for correct translation it is necessary to understand the basics of angiography and know the anatomy of the coronary arteries.
The terms and explanations below are intended to facilitate the work of the translator and help avoid errors when translating angiocoronary angiograms.