Anatomy of the cardiovascular system
1. Right coronary artery 2. Anterior descending artery 3. Appendage 4. Superior vena cava 5. Inferior vena cava 6. Aorta 7. Pulmonary artery 8. Branches of the aorta 9. Right atrium 10. Right ventricle 11. Left atrium 12. Left ventricle 13. Trabeculae 14. Chordae 15. Tricuspid valve 16. Mitral valve 17. Pulmonary valve
In order to talk about diseases of the cardiovascular system, it is necessary to understand its structure. The circulatory system is divided into arterial and venous. Through the arterial system, blood flows from the heart, through the venous system it flows to the heart. There are large and small circles of blood circulation.
The great circle includes the aorta (ascending and descending, aortic arch, thoracic and abdominal sections), through which blood flows from the left side of the heart. From the aorta, blood enters the carotid arteries that supply blood to the brain, subclavian arteries, blood supply to the arms, renal arteries, arteries of the stomach, intestines, liver, spleen, pancreas, pelvic organs, iliac and femoral arteries, and blood supply to the legs. Blood flows from the internal organs through veins that drain into the superior vena cava (collects blood from the upper half of the body) and the inferior vena cava (collects blood from the lower half of the body). The vena cava drains into the right heart.
The pulmonary circulation includes the pulmonary artery (through which, however, venous blood flows). Through the pulmonary artery, blood enters the lungs, where it is enriched with oxygen and becomes arterial. Through the pulmonary veins (four), arterial blood enters the left heart.
The heart pumps blood - a hollow muscular organ consisting of four sections. These are the right atrium and right ventricle, which make up the right heart, and the left atrium and left ventricle, which make up the left heart. Oxygen-rich blood coming from the lungs through the pulmonary veins enters the left atrium, from there into the left ventricle and then into the aorta. Venous blood enters the right atrium through the superior and inferior vena cava, from there into the right ventricle and further through the pulmonary artery into the lungs, where it is enriched with oxygen and again enters the left atrium.
There are pericardium, myocardium and endocardium. The heart is located in the cardiac sac - the pericardium. Cardiac muscle - the myocardium consists of several layers of muscle fibers; there are more of them in the ventricles than in the atria. These fibers, contracting, push blood from the atria into the ventricles and from the ventricles into the vessels. The internal cavities of the heart and valves are lined by the endocardium.
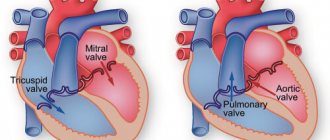
Valve apparatus of the heart
Between the left atrium and the left ventricle there is a mitral (bicuspid) valve, and between the right atrium and the right ventricle there is a tricuspid (three-leaf) valve. The aortic valve is located between the left ventricle and the aorta, the pulmonary valve is between the pulmonary artery and the right ventricle.
Work of the heart
From the left and right atria, blood flows into the left and right ventricles, while the mitral and tricuspid valves are open, the aortic and pulmonary valves are closed. This phase in the work of the heart is called diastole. Then the mitral and tricuspid valves close, the ventricles contract and through the opened aortic and pulmonary valves, blood rushes into the aorta and pulmonary artery, respectively. This phase is called systole, systole is shorter than diastole.
Conduction system of the heart
We can say that the heart works autonomously - it itself generates an electrical impulse that spreads through the heart muscle, causing it to contract. The pulse must be generated at a certain frequency - normally about 50-80 pulses per minute. In the conduction system of the heart, the sinus node is distinguished (located in the right atrium), from which nerve fibers go to the atrioventricular (atrioventricular) node (located in the interventricular septum - the wall between the right and left ventricles). From the atrioventricular node, nerve fibers run in large bundles (right and left bundle branches), dividing into smaller bundles in the walls of the ventricles (Purkinje fibers). An electrical impulse is generated in the sinus node and spreads through the conduction system throughout the myocardium (heart muscle).
Blood supply to the heart
Like all organs, the heart must receive oxygen. Oxygen is delivered through arteries called coronary arteries. The coronary arteries (right and left) arise from the very beginning of the ascending aorta (at the origin of the aorta from the left ventricle). The trunk of the left coronary artery is divided into the descending artery (also known as the anterior interventricular) and the circumflex artery. These arteries give off branches - the artery of the obtuse edge, diagonal, etc. Sometimes the so-called median artery branches off from the trunk. The branches of the left coronary artery supply blood to the anterior wall of the left ventricle, most of the interventricular septum, the lateral wall of the left ventricle, and the left atrium. The right coronary artery supplies part of the right ventricle and the posterior wall of the left ventricle.
Now that you have become an expert in the anatomy of the cardiovascular system, let’s move on to its diseases.
Thromboembolism is blockage of blood vessels by blood clots. The most dangerous is thromboembolism of the pulmonary artery and its branches.
Peripheral arterial diseases:
- Arterial stenosis and occlusion
- Arterial aneurysms
- Raynaud's disease (syndrome)
- Peripheral venous diseases
- Peripheral vein thrombosis
- Phlebitis
- Varicose veins
Materials from the site www.cardioweb.ru
National Society for the Study of Atherosclerosis
In order to talk about diseases of the cardiovascular system, it is necessary to understand its structure. The circulatory system is divided into arterial and venous. Through the arterial system, blood flows from the heart, through the venous system it flows to the heart. There are large and small circles of blood circulation. The great circle includes the aorta (ascending and descending, aortic arch, thoracic and abdominal sections), through which blood flows from the left side of the heart. From the aorta, blood enters the carotid arteries that supply blood to the brain, subclavian arteries, blood supply to the arms, renal arteries, arteries of the stomach, intestines, liver, spleen, pancreas, pelvic organs, iliac and femoral arteries, and blood supply to the legs. Blood flows from the internal organs through veins that drain into the superior vena cava (collects blood from the upper half of the body) and the inferior vena cava (collects blood from the lower half of the body). The vena cava drains into the right heart. The pulmonary circulation includes the pulmonary artery (through which, however, venous blood flows). Through the pulmonary artery, blood enters the lungs, where it is enriched with oxygen and becomes arterial. Through the pulmonary veins (four), arterial blood enters the left heart.
The heart pumps blood - a hollow muscular organ consisting of four sections. These are the right atrium and right ventricle, which make up the right heart, and the left atrium and left ventricle, which make up the left heart. Oxygen-rich blood coming from the lungs through the pulmonary veins enters the left atrium, from there into the left ventricle and then into the aorta. Venous blood enters the right atrium through the superior and inferior vena cava, from there into the right ventricle and further through the pulmonary artery into the lungs, where it is enriched with oxygen and again enters the left atrium.
There are pericardium, myocardium and endocardium. The heart is located in the cardiac sac - the pericardium. Cardiac muscle - the myocardium consists of several layers of muscle fibers; there are more of them in the ventricles than in the atria. These fibers, contracting, push blood from the atria into the ventricles and from the ventricles into the vessels. The internal cavities of the heart and valves are lined by the endocardium.
- Right coronary artery
- Anterior descending artery
- Ear
- Superior vena cava
- Inferior vena cava
- Aorta
- Pulmonary artery
- Branches of the aorta
- Right atrium
- Right ventricle
- Left atrium
- Left ventricle
- Trabeculae
- Chords
- Tricuspid valve
- Mitral valve
- Pulmonary valve
Valve apparatus of the heart
Between the left atrium and the left ventricle there is a mitral (bicuspid) valve, and between the right atrium and the right ventricle there is a tricuspid (three-leaf) valve. The aortic valve is located between the left ventricle and the aorta, the pulmonary valve is between the pulmonary artery and the right ventricle.
Work of the heart
From the left and right atria, blood flows into the left and right ventricles, while the mitral and tricuspid valves are open, the aortic and pulmonary valves are closed. This phase in the work of the heart is called diastole. Then the mitral and tricuspid valves close, the ventricles contract and through the opened aortic and pulmonary valves, blood rushes into the aorta and pulmonary artery, respectively. This phase is called systole, systole is shorter than diastole.
Conduction system of the heart
We can say that the heart works autonomously - it itself generates an electrical impulse that spreads through the heart muscle, causing it to contract. The pulse must be generated at a certain frequency - normally about 50-80 pulses per minute. In the conduction system of the heart, the sinus node is distinguished (located in the right atrium), from which nerve fibers go to the atrioventricular (atrioventricular) node (located in the interventricular septum - the wall between the right and left ventricles). From the atrioventricular node, nerve fibers run in large bundles (right and left bundle branches), dividing into smaller bundles in the walls of the ventricles (Purkinje fibers). An electrical impulse is generated in the sinus node and spreads through the conduction system throughout the myocardium (heart muscle).
Blood supply to the heart.
Like all organs, the heart must receive oxygen. Oxygen is delivered through arteries called coronary arteries. The coronary arteries (right and left) arise from the very beginning of the ascending aorta (at the origin of the aorta from the left ventricle). The trunk of the left coronary artery is divided into the descending artery (also known as the anterior interventricular) and the circumflex artery. These arteries give off branches - the artery of the obtuse edge, diagonal, etc. Sometimes the so-called median artery branches off from the trunk. The branches of the left coronary artery supply blood to the anterior wall of the left ventricle, most of the interventricular septum, the lateral wall of the left ventricle, and the left atrium. The right coronary artery supplies part of the right ventricle and the posterior wall of the left ventricle.
Now that you have become an expert in the anatomy of the cardiovascular system, let’s move on to its diseases.
Coronary heart disease (CHD)
The basis of coronary heart disease is an insufficient supply of oxygen to the heart muscle. That is, there is a discrepancy between demand and delivery. The most common cause of IHD is atherosclerosis of the coronary arteries. An atherosclerotic plaque forms inside the coronary artery, which closes its lumen. With increased stress (physical, psychological stress), the heart requires more oxygen, but its delivery is limited due to partial stenosis (blockage) of the coronary artery. Therefore, the main symptom of angina pectoris is retrosternal (squeezing, pressing) pain during physical activity. The duration of pain is from seconds to minutes (no more than 30 minutes). The pain is usually relieved with nitrates (nitroglycerin). To make a diagnosis of angina, an ECG, stress tests, ECHO CG, 24-hour ECG monitoring, myocardial perfusion scintigraphy, and coronary ventriculography are performed. Angina is divided into stable (angina pectoris, angina at rest) and unstable (progressive, first occurring). A special form of angina is vasospastic (Prince-Menthol), which occurs due to spasm of the coronary arteries. There are three main ways to treat angina - medications (nitrates, b-blockers, angiotensin converting enzyme inhibitors, etc.), balloon angioplasty and coronary artery bypass surgery.
Myocardial infarction
- necrosis (death) of a section of the heart muscle. The causes of myocardial infarction are the same as angina pectoris. The main symptom is prolonged chest pain (more than 30 minutes), which is not relieved by nitrates. The diagnosis of myocardial infarction is made based on the clinical picture, characteristic ECG changes and elevated blood enzyme levels. Treatment is medication (aimed at relieving pain, reducing blood oxygen demand, dilating the coronary arteries); in some cases, within a few hours of the development of a heart attack, it is possible to dissolve a blood clot by administering special drugs (streptokinase, urokinase, etc.). Emergency balloon angioplasty is sometimes performed.
As a result of a myocardial infarction, or due to other diseases (myocarditis), the muscle tissue of the heart is replaced by connective tissue, that is, a scar is formed. Scar changes in the myocardium are called cardiosclerosis .
Disorders of cardiac rhythm and conduction.
Classification
Change in sinus node automaticity:
- sinus bradycardia (slow heart rate),
- sinus tachycardia (accelerated rhythm),
- sinus arrhythmia (irregular rhythm)
Escape rhythms Atrioventricular dissociation Atrial tachycardias Atrioventricular reciprocal tachycardias Ventricular tachycardia Ventricular fibrillation Ventricular preexcitation Sinus node weakness Blocks:
- Sinoatrial
- Atrioventricular
- Bundle branch blocks
Atrial fibrillation and flutter Parasystole
Since it is quite difficult to explain to a non-specialist the essence of these violations, we will decipher only the basic concepts. Extrasystole is an extraordinary contraction of the heart. A distinction is made between atrial extrasystoles (“incorrect” impulse occurs in the atria) and ventricular extrasystoles (“incorrect” impulse occurs in the ventricles). The patient perceives extrasystoles as pauses in the work of the heart. In healthy people, a small amount of extrasitol is recorded per day. Atrial fibrillation (atrial fibrillation) is frequent, chaotic, irregular contraction of the atria and irregular ventricular rhythm. The main causes of atrial fibrillation are damage to the mitral valve, thyrotoxicosis (pathology of the thyroid gland), and cardiosclerosis.
To treat rhythm disturbances, there are several groups of antiarrhythmic drugs; in some cases, pathological foci or nerve pathways are destroyed.
Conduction disorders - delay in the conduction of impulses through the conduction system of the heart - blockade, or vice versa, accelerated conduction of the impulse along additional conduction pathways. Conduction delay is a block; there are sinoauricular, atrioventricular, and bundle branch blocks. Accelerated conduction - WPW (Wolf-Parkinson-White) syndrome is more common.
Hypertonic disease.
The main manifestation of hypertension (HD) is increased blood pressure (BP). This is often manifested by headaches, tinnitus, and flickering of “spots” before the eyes. Hypertension is divided into two large groups - essential (primary) and symptomatic (secondary) hypertension. Essential hypertension is a disease at the level of the whole organism. With secondary hypertension, there is damage to one or another organ, which leads to an increase in blood pressure. Secondary hypertension is divided into renal (glomerulonephritis, pyelonephritis, renovascular hypertension, etc.), endocrine (pheochromocytoma, paraganglioma, Cohn syndrome, Itsenko-Cushing syndrome), vascular (coarthation of the aorta), hypertension with damage to the central nervous system.
When blood pressure increases, changes occur in various organs. The organs most susceptible to the effects of high blood pressure are called target organs. These are the brain, heart, blood vessels, retina, kidneys.
When treating symptomatic hypertension, it is important to eliminate the cause of the increase in blood pressure. The main antihypertensive drugs are b-blockers, angiotensin converting enzyme inhibitors (ACEIs), calcium antagonists, and diuretics.
Heart defects
Heart defects are divided into congenital and acquired. There are quite a large number of names that are congenital; we will not list them all; we will pay attention to the most common ones. These are patent oval window (ventricular septal defect), atrial septal defect, tetralogy and Fallot's triad. Treatment is surgical. Mitral valve prolapse is insufficiency of the mitral valve caused by the “bending” of its valves into the cavity of the left atrium during contraction (systole) of the left ventricle. The reason is connective tissue disorders.
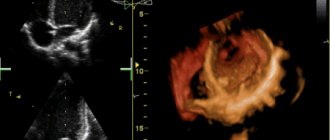
Acquired defects include stenosis (incomplete opening) or insufficiency (incomplete closure) of the heart valves. Stenosis or insufficiency of the mitral and tricuspid valves are more common. The cause of the lesion is rheumatism, endocarditis, atherosclerosis, etc. Treatment is surgical, in the acute phase - antibiotic therapy, hormones, cytostatics, etc.
Primary damage to the heart muscle
Myocarditis Endocarditis Pericarditis Cardiomyopathies
- Dilatational
- Hypertrophic
- Restrictive
Myocarditis is an inflammation of the heart muscle, it can be bacterial, viral, or allergic. This is a rather “complex” disease, since an autoimmune reaction is triggered - antibodies are produced to one’s own muscle. Treatment: antibiotics, hormonal drugs, hydroxyquinolines. Endocarditis is inflammation of the endocardium, often bacterial. Ultimately leads to damage to the heart valves. Treatment: antibiotics, hormones.
Dilated cardiomyopathy is a lesion of the heart muscle, which causes expansion of the heart (enlargement of cavities) and thinning of its walls. The heart's ability to pump blood decreases. The reason is not fully understood. The main manifestation is the occurrence of circulatory failure - shortness of breath, swelling, enlarged liver, attacks of suffocation. Weakness, cardiac arrhythmias, and thromboembolism are common.
Hypertrophic cardiomyopathy is a thickening of the heart muscle, resulting in difficulty ejecting blood from the left ventricle. The reason is not fully understood. The main manifestation is rhythm and conduction disturbances, pain in the heart, weakness.
Restrictive cardiomyopathy is a reduction in the chambers of the heart.
Cor pulmonale is an overload of the heart that occurs due to increased resistance in the vessels of the lungs. The reason for this is primary pulmonary hypertension (primary damage to the blood vessels of the lungs), chronic pulmonary diseases (pneumosclerosis, emphysema, bronchiectasis, bronchitis, etc.) and anatomical changes in the chest. Thromboembolism is blockage of blood vessels by blood clots. The most dangerous is thromboembolism of the pulmonary artery and its branches.
Peripheral arterial diseases:
- Arterial stenosis and occlusion
- Arterial aneurysms
- Raynaud's disease (syndrome)
- Peripheral venous diseases
- Peripheral vein thrombosis
- Phlebitis
- Varicose veins
ANATOMICAL FEATURES OF BLOOD SUPPLY TO THE HUMAN HEART
Relevance: modern methods of surgical treatment of various heart diseases, the use of intravital coronary angiography require further study of the coronary arteries. Until now, there are disagreements regarding the typical features of the blood supply to the heart, the morphology and topography of anastomoses, as well as the paths of collateral blood flow [1.2,3,4,5]. Many opinions regarding the criteria for classifying the blood circulation of the heart into one of the types are associated with high variability in the structure of the coronary bed[6,7]. Hence the need arises to study the general patterns of blood supply to the heart.
Purpose of the study: to study the typical features of the blood supply to the heart.
Materials and methods of research: the study was carried out on 40 isolated heart specimens of adults of both sexes, admitted to the morgue of the Department of Normal Anatomy, as well as the Department of Clinical Anatomy and Operative Surgery of KazNMU named after. S.D. Asfendiyarov. Various research methods were used: 1-microanatomical preparation, 2-morphometry of the coronary vessels, 3-staining of the vessels, 4-photography, 5-statistical processing of the obtained material.
Results and discussions: three types of blood supply to the heart were identified: right-coronary, left-coronary and uniform. The right coronary type included those cases when the right coronary artery (RCA) branched in the right parts of the heart, was the source of the posterior descending artery and at the same time took part in the blood supply to the posterior wall of the left ventricle (the branching zone ranged from 1/3 to 2/3). The left coronal type of blood supply was characterized by the fact that in addition to the branch to the left ventricle, the left circumflex artery sent a posterior descending branch, the latter supplying blood to 1/3 of the posterior surface of the right ventricle. With a uniform type of blood supply to the heart, the source of the posterior interventricular branch was the right coronary artery, but unlike the right coronary type, the descending branch did not participate in the blood supply to the posterior wall of the left ventricle. As the materials of our study show, the right-coronal type is predominant (80.5% of cases), while the left-coronal and uniform types of blood supply occur (8% and 11.5%, respectively). According to our preparations, the same diameter of the mouths of both coronary arteries was found in 20.7% of cases. In 44.6% of cases, the mouth of the SVA exceeded the diameter of the LVA; less often, in 37.7 cases, the opposite relationship occurred. The SVA more often than 48% began below the LVA, less often in 28.9% both coronary arteries began at the same level. In 54.4% of cases, the orifice of the LVAD was displaced to the anterior section of the corresponding aortic valve, and the SVA was displaced to the posterior section of the aortic valve (56.3%). Almost equally rarely, the orifices of both coronary arteries (in 13.8% - right, 17.3% - left) corresponded in position to the middle of the aortic valve. The anatomical features of the blood supply to the human heart are determined by the nature of the distribution of the coronary arteries in the ventricular myocardium. Thus, the anterior descending branch of the LVA in 50.4% of cases passed to the posterior surface of the heart, and most often it branched in the area of the apex of the heart to a lesser extent - in the lower part of 1/3 of the longitudinal groove of the heart. The topography of the left circumflex artery depended on the areas of branching of the anterior descending branch and the SVA. Typically, the circumflex artery sent one branch to the anterior and posterior surfaces of the left ventricle. But, in 36.6% of cases, the anterior descending artery gave two branches to the left ventricle. There was no clear relationship between the type of blood supply to the heart and the number of branches of the predominant artery to the myocardium in our preparations. The type of blood supply to the heart also determines the structure of anastomoses, the number of which decreases with age, and their diameter increases. The anastomoses are most clearly noted in the right coronary type, when the branching zone of the right coronary artery on the posterior surface of the heart is ½ of the left ventricle. The type of blood supply to the heart determines the effect on the areas of vascular distribution. Thus, with an increase in the area of branching of the SVA on the posterior surface of the heart, there is an increase in the diameter and territory of distribution of the anterior descending branch on the anterior surface of the left ventricle and in the area of the interventricular septum. As a number of researchers note [9,10,11], due to these circumstances, occlusion of even large arterial branches can be asymptomatic. The prognosis of myocardial infarction depends on the structural features and topography of the coronary arteries of the heart, among other conditions.
Conclusions: the identification of right-coronal, left-coronal and uniform types of blood supply to the heart is based on the preferential development of one of the 2 arteries supplying the heart. This division is convenient from a clinical point of view when interpreting the results of coronary angiography, as well as determining indications for surgical treatment. Most studies on this topic are aimed at studying the criteria for whether the blood supply to the heart belongs to one type or another. As the results of a morphometric study show, the type of blood supply to the heart does not always mean the predominant development of one of the arteries. From the statistical data it is clear that the right-coronal type is predominant (80.5% of cases), from which we conclude that the left-coronal and uniform type include extreme variants in the structure of the coronary arteries. Thus, all transitional forms in the development of the coronary arteries are included in the group with the right type of blood supply. Therefore, we believe that the types of blood supply to the heart are reference points in the study of the coronary arteries, but cannot explain the variety of options for their development.
Bibliography
1. Babunashvilli A.M., Rabkin N.Kh., Ivanov V.A. Coronary angioplasty. M., DIA 1996, p. 352.
2. Belenkov Yu.I., Mareev Yu.V., Ageev F.T. Chronic heart failure. Selected lectures on cardiology. M. GEOTAR-MEDIA, 2006, p. 429.
3. Bockeria L.A., Alekyan B.G., Colombo A. Interventional methods for the treatment of coronary heart disease. M., 2002 from 417.
4. Bockeria L.A., Berishvilli I.I. Surgical anatomy of the heart in 3 volumes. - Scientific Center for Cardiovascular Surgery named after. A.N. Bakuleva. RAMS-2006-Vol.1. p296-297.
5. Bockeria L.A., Rabotnikov V.S., Buziashvilli Yu.I. Coronary heart disease in patients with low contractility of the left ventricular myocardium (diagnosis, treatment tactics). M: NTsSSKh them. A.N.Bakuleva RAMS 2001
6. Vakhromeeva M.N. Normal distribution and abnormalities of the coronary arteries in the human heart. Dissertation for Candidate of Medical Sciences M., 1992.
7. Luzha O. X-ray anatomy of the vascular system. Budapest 1973 - pp.29-33.
8. Sokolov Yu.N., Sokolov M.Yu., Kostenko L.N. Invasive cardiology and coronary disease. K. Mornon 2002 from 360.
9. Turegalieva A.G. - On the development of cardiac and cardiac surgical care in the Republic of Kazakhstan. Therapeutic Bulletin. 2010.-s. 4-5.
10. Berishvilly. Cjngenital anomalies of coronary arteries in children cardiac. Simposiam on the 60ths SSCVS international congress.-Moscow, 2011, lecture.-May, 22. 2011.
11. Levin DC Anatomic variations of the coronary arteries supplying the anterolateral aspect of the left ventricle.// Invest. Radiol.- 1982.-Vol. 17, -p.458.