Definition:
Myocardial revascularization is the restoration of the patency of the arteries of the heart (coronary arteries) through surgery.
Such operations include:
- Percutaneous coronary intervention (stenting, angioplasty). The main idea of these operations is to restore and maintain blood flow in the vessels. A stent is passed and placed into the heart arteries by first dilating the artery with a balloon. A stent is a thin metal wire tube. By expanding the artery and thereby increasing its diameter, the stent further preserves the lumen of the artery. This is a more gentle operation than coronary artery bypass grafting. It is performed under local anesthesia, without anesthesia.
- The coronary artery bypass surgery involves sewing additional vessels (shunts) to the ascending aorta, which will supply blood to the area of the heart suffering from a lack of blood and oxygen. Arteries located in the chest, veins in the legs and some other vessels are used as additional vessels. The operation is performed on a stopped heart, and the patient is connected to a heart-lung machine.
- An additional way to improve blood supply to the heart is laser revascularization of the myocardium. The operation consists of “burning” the myocardium (heart muscle) with a special laser in order to form small holes in it, which helps to increase blood supply to this area of the heart.
Bibliography
1. Schub C. Stable angina pectoris, 3: medical treatment. Mayo din Proc. 1990:65:256-273. 2. Stone PH, Gibson RS. Glasser SP, et al. ASIS Study Group. Comparison ot'propranolol, diltiazem, and nifedipine in the treatment of ambulatory ischemia in patients with stable angina: differential effects on ambulatory ischemia, exercise performance, and anginal symptoms. Circulation. 1990:82:1962-1972. 3. RITA-2 Trial Participants. Coronary angioplasty versus medical therapy for angina: the Second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997:350:461-468. 4. Chaitman BR. Rosen AD. Williams D.O. et al. Myocardial infarction and cardiac mortality in the Bypass Angioplasty Revascularization Investigation (BARI) randomized trial. Circulation. 1997:96:2162-2170″ 5. Alien KB, Dowling RD, Fudge TL, et al. Comparison of transmyocardial revascularization with medical therapy in patients with refractory angina. N En^l .1 Mcd. 1999:341:1029-1036. 6. Frazier OH. March R.J. Horvath K.A. Transmyocardial revascularization with carbon dioxide laser in patients with end-stage coronary artery disease. N Enyl J Med. 1999:341:1021-1028. 7. Whitlow PL, Knopf WD. O'Neill WW. Kaul U. Londero H, Shawl F. Six month follow-up of percutaneous transmyocardial revascularization in patients with refractory angina [abstract]. J Am Coil Cardiol. 1999;33(suppl):29A. 8. Benetti F, Mariani MA. Sani G. et al. Video-assisted minimally invasive coronary operations without cardiopulmonary bypass: a multicenter study../ Thorac Surg. 1996:112:1478-1484. 9. Boonstra PW, Grandjean JG, Mariani MA. Improved method for direct coronary grafting without CPB via anterolateral small thoracotomy. Ann Thorac Surg. 1997:63:567-569. 10. Holubkov R, Zenali M, Akin JJ. Erb L, Courcoulas A. MIDCAB characteristics and results: the CardioThoracic Systems (CTS) registry. EiirJCardiothoracSurs. 1998:14(suppl 1):S25-S30. 11. Mariani MA. Boonstra PW, Grandjean JG, et al. Minimally invasive coronary artery bypass grafting versus coronary angioplasty for isolated type C stenosis of the left anterior descending artery. J Thorac Cardiovasc Surf;.1997:114:434-439. 12. Alderman EL. Levy JH. Rich JB, et al. Analyzes of coronary graft patency after aprotinin use: results from the International Multi-center Aprotinin Graft Patency Experience (IMAGE) trial. J Thorac Cardiovasc Surf;. 1998; 116:716-730. 13. Chauhan A. Mullins PA. Thuraisingham SI, Taylor G, Fetch MC, Schofield PM. Effect of transcutaneous electrical nerve stimulation on coronary blood flow. Circulation. 1994;89:694-702. 14. DeJongste MJ, Hautvast RW, Hillege HL, Lie KI. Working Group on Neurocardiology. Efficacy of spinal cord stimulation as adjuvant therapy for intractable angina pectoris: a prospective, randomized clinical study. J Am Colt Cardiol. 1994;23:1592-1597. 15. Yeung AC, Hayase M, Fitzgerald P, et al. Percutaneous in-situ coronary artery bypass (PICAB): current development status and preliminary results of a novel myocardial revascularization technique [abstract]., I Am Coil Cardiol. 1999:33(suppl):47A. 16. Carter AJ. Kornowski R. Lamson T, et al. Percutaneous in-situ coronary venous arterial bypass: initial results of retrograde myocardial perfusion in a porcine model [abstract]. J Am Coil Cardiol. 1999;33(suppl):49A. 17. Symes JF. Losordo DW, Vale PR, et al. Gene therapy with vascular endothelial growth factor for inoperable coronary artery disease. Ann Thorac Sui-s. 1999:68:830-836. 18. Arora RR, Chou TM. Jain D. et al. The Multicenter Study of Enhanced External Counterpulsation (MUST-EECP):effect of EECP on exercise-induced myocardial ischemia and anginal epi.sodes.7Aw Coil Cardiol. 1999:33:1833-1840. 19. Lawson WE. Hui J.C. Soroff HS, et al. Efficacy of enhanced external counterpulsation in the treatment of angina pectoris. Am J Cardiol. 1992:70:859-862. 20. Lawson WE, Hui JCK, Zheng ZS, et al. Three-year sustained benefit from enhanced external counterpulsation in chronic angina pectoris. Am J Cardiol. 1995:75:840-841. 21. Zheng ZS. Li TM, Kambic H, et al. Sequential external counterpulsation (SECP) in China. Trans Am Soc Artif Intern Organs. 1983:29:599-603. 22. Karim S, Sani A, Karo-Karo S. et al. Enhanced external counterpulsation in the treatment and rehabilitation of coronary patients in Indonesia. Asian Cardiovasc Thorac Ann. 1995;3: 26-28. 23. Kantrowitz A, Kantrowitz A. Experimental augmentation of coronary flow by retardation of the arterial pressure pulse. Surgery. 1953:34:678-687. 24. Moulopoulos SD, Topaz S, Kolff WJ. Diastolic balloon pumping (with carbon dioxide) in the aorta—a mechanical assistance to the failing circulation. Am Heart.I. 1962:63:669-675. 25. Jacobey JA. Taylor WJ, Smith GT. Gorlin R. Harken DE. A new therapeutic approach to acute coronary occlusion. II: opening dormant coronary collateral channels by counterpulsation. Am J Cardiol. 1963:11:218-227. 26. Masuda D, Nohara R, Hirai T, et al. The new therapeutic approach with the enhanced external counterpulsation in patients with chronic stable angina: evaluation of myocardial flow and flow reserve by N-13 ammonia PET [abstract]. Circulation. 1999; 100(suppl):l-732. 27. Sessa WC. Pritchard K, Seyedi N, Wang J, Hintze TH. Chronic exercise in dogs increases coronary vascular nitric oxide production and endothelial cell nitric oxide synthase gene expression. Circ Res. 1994:74:349-353. 28. Garlichs CD. Zhang H. Werner D, John A, Tragner P. Daniel WG. Reduction of serum endothelin-1 levels by pneumatic external counterpulsation [abstract]. Can J Cardiol. 1998; 14(suppl): 87F. 29. Zarins CK. Zatina MA. Giddens D.P. Ku DN. Glagov S. Shear stress regulation of artery lumen diameter in experimental atherogenesis. J Vase Surg. 1987:5:413-420. 30. Tseng H, Peterson TE, Berk BC. Fluid shear stress stimulates mitogen-activated protein kinase in endothelial cells. Circ Res. 1995;77:869-878.
Indications for revascularization
Restoring the blood supply to the heart surgically is performed if there is no effect (or insufficient effect) from taking drug therapy. The choice of myocardial revascularization technique is a complex, integrated approach based on an assessment of the patient’s condition, the characteristics of coronary artery lesions, concomitant diseases, the complexity of the postoperative period, etc.
To determine the indications for a particular treatment method, it is recommended to undergo a full cardiac examination. We use modern equipment techniques, which allows us to minimize the risk of complications after operations.
If you have discovered some, even minor, signs of cardiovascular disease, do not put off visiting a doctor until later. If you need to see a cardiologist, you can do this online on our website.
Treatment and period after the course of EECP
EECP therapy did not start by chance. At the beginning of treatment, the patient required assistance in getting to her treatment session due to angina pectoris. During treatment, she noted a decrease in angina attacks, accompanied by an increase in physical activity (Table 3). At the end of the 7-week course of treatment, she experienced no restrictions in physical activity, including 60 minutes of cycling or treadmill training. She continued to take the same angina medications as before EECP.
Rice. 1. The mechanism of diastolic enhancement and afterload reduction during EECP use. ECG-dependent sequential diastolic activation of “milk” venous blood of the lower extremities and arterial blood from the periphery to the main vessels of the system was noted (stage 1-3). All cuffs are simultaneously deflated immediately before systole (step 4).
Subsequently, an improvement in myocardial perfusion was observed, as shown by scintigraphy data during the adenosine test; no signs of myocardial ischemia or myocardial infarction were detected (Fig. 2). 9 months after the end of the course of treatment, the patient remained active, angina attacks were less than once a month, and immediately stopped with rest or after the use of sublingual nitroglycerin.
Table 3. Clinical picture during treatment.
| Week 1 1 attack of angina at rest Physical activity limited to hotel room Week 3 1 attack of angina at rest Walking around hotel room Week 5 2 short attacks of mild angina Patient begins small exercise program Week 7 No angina Walking /ride a bike for 60 minutes a day |
Fig. 2 Comparison of resting and stress perfusion images obtained before (left) and after (right) EECP treatment. There is a decrease in myocardial ischemia caused by adenosine in the inferior wall (arrow), inferior septal segment (asterisk), and apical segment of the LV (plus sign) after treatment. The marks are on the image taken before treatment. Redist - redistribution.
conclusions
The widespread prevalence of coronary heart disease and the high risk of complications and death of patients contributes to the use of radical treatment methods. Methods of revascularization of coronary vessels make it possible to restore normal blood supply to the myocardium. The “gold standard” for providing care for acute coronary syndrome with ischemia of the heart muscle is placing a stent into the lumen of the affected area. All interventions are performed exclusively by cardiac surgeons, taking into account the patient’s indications and contraindications.
results
Immediate mortality (in hospital or in the first 30 days) after combined CABG and TMLR was 1.6% (1/60). The cause of death was multiple organ failure. According to our data, the mortality rate was lower compared to the data given in the literature (1.6% versus 6.3%).
Postoperative complications are presented in table. 2.
Table 2. Postoperative complications (in hospital or within 30 days)
3 (5%) patients experienced rhythm disturbances (atrial fibrillation), which were treated with medication. The postoperative period in these patients was uneventful, and they were discharged from the hospital on time.
All patients were extubated on the 1st day after surgery. The length of stay of patients in the intensive care unit was 2.2±0.7 bed days. The use of intra-aortic balloon counterpulsation was not required in any case. The total length of hospitalization was 11.1±2.9 bed days. Before discharge, LVEF increased from 48.8±4.97 to 54.9±4.08%.
Thus, analysis of the immediate postoperative period showed that TMLR is quite safe for the patient and does not require an expansion of the standard volume of intensive care in the intensive care unit.
Long-term follow-up
Clinical follow-up of patients in the long-term period was carried out 3, 6 and 12 months after surgery and then selectively up to 10 years after surgery (on average 7.5±0.9 years). At each interval, patients underwent clinical and instrumental examination. The clinical status of the patient was assessed based on the dynamics of angina FC and treadmill test. Transthoracic echocardiography was performed to monitor the effect on global and segmental myocardial contractility.
The dynamics of angina FC in patients after combined CABG and TMLR are presented in the figure.
Dynamics of the functional class of angina before and after surgery.
All patients were admitted to the clinic with an initially high angina FC. By the 12th month after surgery, a sharp decrease in angina FC was detected. This trend was followed up to 5 years, then a slight increase in angina FC was noted, which required an increase in nitrate intake.
All patients showed an increase in exercise tolerance after 12 months of observation.
In the long-term period, on average 7.5±0.9 years after surgical treatment, 2 patients required treatment for angina (percutaneous transluminal coronary angioplasty was performed), which is associated with the progression of the atherosclerotic process in the coronary vessels.
Survival rate after 7.5±0.9 years was 91.6% ( n
=55).
Discussion
Transmyocardial laser revascularization has received approval for the treatment of patients with grades III and IV angina at five cardiac surgery centers in the United States (St. Luke's Hospital in Milwaukee, New York-Presbyterian Columbia-Cornell University Hospital, Mayo Clinic, Duke University Hospital, Massachusetts General Hospital), where it was performed. Prospective randomized studies. St. Hospital was involved in the implementation of the first stage of the protocol. Luke's in Milwaukee. The patients underwent combined myocardial revascularization—CABG and laser recanalization using a holmium laser. The second phase of clinical trials involved the use of TMLR both as a stand-alone procedure and in combination with CABG. 4 other centers were involved in this work. After surgery, patients were assessed for the frequency and intensity of angina, episodes of unstable angina, myocardial infarction and other clinical indicators, such as stress tests, myocardial scintigraphy with thallium [10]. Taking into account the clinical success of both isolated TMLR and in combination with CABG, at the VII Annual Conference of Cardiothoracic Surgeons in Barcelona (1993), TMLR received final recognition as an alternative method of myocardial revascularization, the third after CABG and percutaneous transluminal coronary angioplasty. The US Society of Thoracic Surgeons (STS) and the Society of Minimally Invasive Surgeons (ISMICS) came to the conclusion that the evidence of the effect of combined operations indicates the validity of their use in this severe category of patients [11-13].
In 2000, the results of combined operations in 20 patients in whom TMLR was performed using a holmium laser were presented by G. Actis Dato et al. from the University of Cardiac Surgery in Turin (Italy) [14]. In 2004, J. Van der Sloot et al. published a randomized trial using the XeCl laser [15]. In 2010, S. Pratali et al. published long-term results (up to 12 years) of using a holmium laser [16]. All these works showed a temporary (up to 1 year) improvement in the condition of patients with subsequent return of angina.
In Russia, a number of studies were carried out at the Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev, Novosibirsk Research Institute of Circulatory Pathology named after. acad. E.N. Meshalkin [17] on the topic of surgical treatment of patients with coronary artery disease using CABG in combination with and without TMLR. The results of using a CO2 laser were evaluated. The data obtained in both studies are quite comparable with ours: angina FC in patients after CABG + TMLR significantly decreased by more than 2 classes in all studies. The need for nitrates has also decreased. In the long-term period, up to 10 years, a significant increase in LVEF and an improvement in the quality of life of patients was revealed.
In the world literature, sufficient attention has been paid to evaluating the results of combined CABG and TMLR, but the authors used different lasers: CO2 laser, Ho:YAG, XeCl. Also, in most reports, the assessment of results is based on a small number of observations. This applies to systematic reviews, randomized trials, meta-analyses, and large non-randomized single-center studies. Each of these works has certain disadvantages. For example, in the largest of them [16–18], the results of combined coronary artery bypass surgery with transmyocardial laser revascularization are compared with the data of isolated CABG in a group of patients with uncomplicated coronary artery disease without diffuse coronary artery disease, or the results are summarized in centers performing a small number of operations.
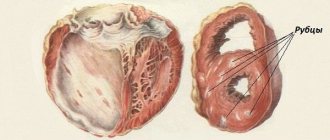
O. Howard et al., using a CO2 laser, observed a decrease in the size of myocardial infarction and an improvement in regional contractility after TMLR. They explain the benefits of TMLR, which have been verified histologically. Endocardium undergoing laser revascularization in dogs also demonstrated preservation of myocardial function during acute ischemia due to improved perfusion through the laser channels.
Long-term benefits on angina and exercise capacity are more difficult to assess after combined CABG and TMLR due to the strong beneficial effects of bypass surgery. In our study, in the long-term period, the patients' condition significantly improved, angina FC decreased by more than 2 classes in all patients, and exercise tolerance increased.
Yet the mechanism of TMLR remains controversial and may be multifactorial. There are currently no convincing theories. Functioning shunts make a certain contribution to improving the condition of patients. The clinical effectiveness of TMLR requires further research.