Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
The main cause of cerebrovascular accidents is atherosclerosis of the carotid arteries. Atherosclerotic plaques cause narrowing of the carotid arteries, which is an obstacle to normal blood circulation in the brain. Gradually, a complete blockage of the carotid artery develops, which is called occlusion. Impaired patency of the carotid artery is the main cause of ischemic stroke in the modern world. The risk of developing a stroke if the carotid artery is narrowed symptomatically by 70% or more is about 15% per year.
Many people die or become disabled from stroke every year, although modern vascular surgery can prevent it in most patients. Only regular diagnosis and trust in doctors will significantly reduce the risk of stroke. It is much easier to treat atherosclerosis of the carotid artery than ischemic stroke and its consequences.
Causes and risk factors
The carotid arteries are paired large arterial vessels that supply blood to the brain in those sections where the centers of thinking, speech, personality, sensory and motor function are located. The carotid arteries run through the neck and enter the brain through openings in the skull.
When fatty substances and cholesterol accumulate, an atherosclerotic plaque is formed, which narrows the carotid arteries. This reduces blood flow to the brain and increases the risk of ischemic stroke. A stroke occurs when blood flow does not reach any part of the brain. During a stroke, some brain functions are suddenly lost. If the lack of blood flow lasts more than three to six hours, then these disorders become irreversible.
Why does a stroke develop when the carotid artery narrows?
- Significant narrowing of the carotid artery reduces blood circulation in the brain, and with a sudden drop in pressure (suddenly getting out of bed, flying, overheating in the sun or major surgery), the blood flow suddenly stops, which leads to the death of nerve cells.
- Tearing off a piece of atherosclerotic plaque with its transfer by the bloodstream into small arteries of the brain, which leads to their blockage.
- Acute thrombosis (formation of a blood clot) due to narrowing of the carotid artery with complete cessation of blood flow in certain areas of the brain.
Diagnostic methods
After collecting anamnesis, identifying risk factors and characteristic symptoms, the doctor may conduct an additional examination, including:
- A physical examination,
during which the doctor, using a phonendoscope, can detect a noise above the carotid artery in the neck, which indicates a narrowing of the artery. The doctor may also conduct a neurological examination to assess your physical and mental status, such as strength in your limbs and ability to remember spoken language. - Ultrasonography.
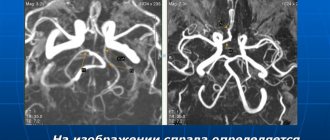
The most common non-invasive research method to assess the condition of the carotid arteries is Doppler ultrasound. This is a variant of conventional ultrasound examination that evaluates blood flow speed, pressure and can detect narrowing of the lumen of the arteries due to changes in these indicators. - Computed angiography.
This procedure is performed using a contrast agent to highlight the arterial vessels. The drug is administered intravenously. When it reaches your carotid arteries, a series of X-ray images are taken of the neck and brain area in different views. - Magnetic resonance imaging.
Similar to CT scanning, this method can visualize brain tissue and detect early brain lesions or other pathology. - Angiography.
It is a more “sensitive” invasive research method. However, it is now used less and less due to the existing risk of stroke during the procedure. During the study, X-ray images of the arterial vessels supplying the brain are taken, with preliminary intra-arterial administration of a contrast agent.
Risk factors for carotid atherosclerosis
Risk factors for carotid artery disease are similar to those for other types of cardiovascular disease. They include:
- Age
- Smoking
- Hypertension (high blood pressure) is the most important risk factor for stroke
- High cholesterol
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of atherosclerosis
Men under 75 years of age have a greater risk of developing carotid artery stenosis than women in the same age group. In the group over 75 years of age, women have a greater risk of stroke. In patients suffering from coronary artery disease, narrowing of the carotid artery is often detected.
Treatment
The goal of treatment of atherosclerotic lesions of the carotid arteries is to prevent the development of stroke. The choice of treatment method depends on the degree of narrowing of the artery lumen.
Slightly and moderately expressed narrowing.
In the presence of moderate narrowing of the carotid arteries, the following recommendations may be sufficient to prevent stroke:
- Lifestyle changes. Healthy lifestyle changes can help reduce damage to the carotid artery wall and slow the progression of atherosclerosis. Such changes include quitting smoking, losing weight, eating a healthy diet, reducing salt intake and regular exercise.
- Treatment of concomitant chronic diseases. At the same time, it is necessary to treat such concomitant diseases as arterial hypertension, obesity and diabetes mellitus.
- Prescribing medications. Your doctor may prescribe you to take aspirin or other antiplatelet medications daily to reduce the risk of blood clots. Therapy aimed at correcting blood pressure (ACE inhibitors, beta blockers) and correcting the lipid profile – taking statins – may also be recommended.
Complaints and symptoms
Atherosclerosis of the carotid arteries can be asymptomatic or cause complaints associated with impaired cerebral blood flow. Most often, patients may complain of temporary impairment of brain function (transient ischemic attack) or persistent loss of brain function (ischemic stroke).
Transient ischemic attack (TIA)
A TIA occurs when blood flow to the brain is briefly interrupted. This is the initial phase of acute cerebrovascular accident, which is reversible. It has the same symptoms as a stroke, but these symptoms go away within minutes or hours.
A TIA requires emergency medical attention because it is impossible to predict whether it will progress to a stroke. Immediate treatment can save lives and increase the chances of a full recovery.
Modern research has shown that patients who have had a TIA are 10 times more likely to suffer a major stroke than a person who has not had a TIA.
Ischemic stroke has the following symptoms:
- Sudden loss of vision, blurred vision, difficulty in one or both eyes.
- Weakness, tingling, or numbness on one side of the face, one side of the body, or one arm or leg.
- Sudden difficulty walking, loss of balance, lack of coordination.
- Sudden dizziness.
- Difficulty speaking (aphasia).
- Sudden severe headache.
- Sudden memory problems
- Difficulty swallowing (dysphagia)
Ischemic stroke and transient ischemic attack begin in the same way, so any ischemic stroke can be called an ischemic attack if the symptoms completely resolve within 24 hours of the onset of the disease. The presence of a time interval between the onset of stroke symptoms and the death of parts of the brain allows for urgent surgery to restore cerebral blood flow.
Complications
Atherosclerotic plaque
The most dangerous complication of atherosclerotic lesions of the carotid arteries is stroke. There are various mechanisms that increase the risk of stroke:
- Decreased blood flow.
The carotid arteries may become so narrowed by atherosclerotic lesions that they are unable to provide adequate blood supply to the brain. - Rupture of an atherosclerotic plaque.
Particles of atherosclerotic plaque can break off and travel with the bloodstream into smaller vessels of the brain, blocking the lumen of these arteries and blocking the blood supply to the area of the brain that is fed by this vessel. - Blood clot formation.
The surface of some atherosclerotic plaques may rupture to form an uneven, ulcerated surface. When this happens, the body's response is to attract platelets to the site of the break and form a blood clot (thrombus). Large blood clots can partially or completely block the lumen of an artery, thereby impeding blood flow and causing a stroke.
The consequences of a stroke can be the formation of a focus of brain damage and dysfunction of organs, in particular paralysis of the limbs. In severe cases, a stroke can be fatal.
Stroke or transient ischemic attack are often the first manifestations of atherosclerotic lesions of the carotid arteries and are considered medical emergencies. If you or your loved ones have symptoms of impaired blood supply to the brain, you should urgently seek medical help. Do not try to get to the hospital on your own.
Signs of concern:
- sudden feeling of numbness or weakness in the face or limbs, usually on one side;
- impaired speech or understanding;
- sudden loss of vision in one or both eyes;
- dizziness or loss of balance;
- sudden causeless severe headache;
Course of the disease
Once atherosclerotic plaques appear, they will no longer be able to resolve, but only gradually progress. The rate of growth of an athersclerotic plaque depends on many risk factors, including cholesterol levels. All people over 50 years of age are recommended to undergo an annual ultrasound of the carotid arteries in order to exclude the development of atherosclerotic plaques and the risk of ischemic stroke.
With the development of complications of atherosclerosis of the carotid arteries, discirculatory encephalopathy quickly progresses. Frequent TIAs, and even more so ischemic stroke, contribute to the death of part of the brain tissue and disruption of brain function. Patients with atherosclerosis of the carotid arteries often develop vascular dementia (dementia).
After restoration of the patency of the carotid artery, the phenomena of cerebrovascular insufficiency are stopped, and the likelihood of repeated cerebrovascular accidents is significantly reduced.
Atherosclerosis with thrombosis of the anterior cerebral artery
Atherosclerotic deposits in the lower segment of the anterior cerebral artery rarely give pronounced clinical symptoms of neurological deficit, since blockage of the lumen (occlusion) is compensated by collateral blood flow through the anterior communicating artery. The likelihood of a transient ischemic attack (TIA, microstroke) and stroke increases if the path of collateral blood flow is characterized by a congenital fusion (atresia) or if there are atherosclerotic changes in a higher section of the anterior cerebral artery.
Forecast
Carotid atherosclerosis carries a significant risk of ischemic stroke. With asymptomatic narrowing of the internal carotid artery of more than 70%, the risk of ischemic stroke exceeds 5% per year. If the patient has had episodes of cerebrovascular accidents, then this risk is already 25% per year.
The risk of ischemic stroke in asymptomatic atherosclerotic plaques with a narrowing of less than 70% does not exceed that in patients without atherosclerosis.
After adequate restoration of blood circulation in the carotid arteries, the risk of ischemic stroke is reduced by more than 3 times.
Atherosclerosis with thrombosis of the middle cerebral artery
Atherosclerosis with thrombosis of the trunk of the middle cerebral artery can cause symptoms of cerebral ischemia both due to a narrowing of the lumen of the artery, and as a result of blockage of the initial segments of one or more arteries of the lenticular nucleus and striatum, supplying blood to the deep white matter and subcortical nodes. Clinically manifested atherosclerotic plaque is rarely located below the first division (bifurcation) of the middle cerebral artery. Since the circle of Willis is located below the beginning of the middle cerebral artery, collateral blood supply in the middle cerebral artery basin should be carried out through small superficial cortical vessels of the adjacent blood supply zones and anastomoses from the anterior and posterior cerebral arteries.
The cause of ischemic stroke in the middle cerebral artery is atherosclerotic thrombosis.
Available data indicate that before the development of cerebral infarction (stroke), narrowing of the lumen of the vessel is usually “prevented” by transient ischemic attacks (TIA, microstrokes) in the middle cerebral artery basin. Their symptoms are similar to those of transient ischemic attacks (TIA, micro-stroke), associated with deterioration of blood circulation as a result of severe stenosis of the internal carotid artery. In contrast to the internal carotid artery, the trunk of the middle cerebral artery and one or more of its major branches are usually occluded by an embolus (arterioarterial, cardiac, or unknown source).
What is the carotid artery, its functions
There are two carotid arteries in the human body. These are the largest vessels that supply the human brain, visual organs and most of the head with oxygen and nutrients. If blood flow to them is disrupted, a person is more likely to experience a major stroke . The disease has a high mortality rate and even after recovery can cause a number of additional health problems. However, this is only one of the many consequences of dysfunction of these arteries.
Hello student
In addition to the branches listed below, from both common carotid arteries, small branches depart in an irregular manner to the trachea, esophagus, deep cervical lymph nodes and to the ventral musculature of the neck.
Caudal thyroid artery, a. thyreoidea caudalis, is always weaker than the cranial thyroid artery and can often be completely absent, especially in the cat. It starts from the initial section of the common carotid artery. The arteries run cranially on both sides of the trachea, giving off thin branches to the trachea and esophagus, and caudal to the thyroid gland anastomose with the dorsal branches of the cranial thyroid arteries.
Large cranial thyroid artery, a. thyreoidea cranialis is the main vessel supplying blood to the thyroid gland. It starts from the common carotid artery caudal to the larynx and covers the thyroid gland from the cranial end with dorsal and ventral branches, ramus dorsalis and ramus ventralis. In addition to them, the sternocleidomastoid branch, ramus sternocleidomastoideus, servicing the cranial parts of the sternomastoid and cleidomastoid muscles, the pharyngeal branch, ramus pharyngeus, for the caudal constrictors of the pharynx and the laryngeal branch, ramus laryngeus, vascularizing the larynx, depart from the cranial thyroid artery.
In a cat, the diameter of the common carotid artery in the area from the beginning of the cranial thyroid artery to the origin of the occipital artery is noticeably increased and forms the sinus of the carotid artery, sinus caroticus. In a dog, this expansion is always located at the initial part of the internal carotid artery, but as an exception, it can also spread to the adjacent section of the common carotid artery. Baroreceptors are localized in the wall of the carotid artery sinus, excitation impulses from which are transmitted through the corresponding branch of the glossopharyngeal nerve to the medulla oblongata. The carotid ball, glomus caroticum, located here is an organ that performs the function of a chemoreceptor.
Internal carotid artery, a. carotis interna, in a dog it goes to the base of the skull and through the carotid canal enters the cranial cavity, supplying blood to the brain. Blood for the blood supply to the brain in a cat comes rostrally on each side from the branches of the miraculous network of the maxillary artery and from the anastomotic branches of the ascending pharyngeal arteries, as well as caudally from the main arteries, which receive large quantities of blood from the vertebral arteries.
Rice. 2. Schematic representation of the cranial thyroid artery in a dog, view from the lateral side (after Henninger, 1991)
1st place of origin a. thyreoidea cranialis; 2 ramus stemocleidomastoideus, 2 terminal branches; 3 ramus dorsalis with glandular branches; 4 ramus pharyngeus, 4′ ramus laryngeus; 5 a. thyreoidea caudalis with dorsal rami oesophagei and ventral rami tracheales; 6 ramus ventralis with glandular branches; 7 ramus cricothyreoideus, 7′ ramus laryngeus; 8 a. laryngea cranialis; 9 ramus pharyngeus; 10 ramus laryngeus; 11 a.m. carotis interna; 12 a.m. occipitalis; 13 a.m. carotis communis
External carotid artery, a. carotis externa, is a continuation of the common carotid artery in the cranial direction, and on the lateral side it is crossed by the hypoglossal nerve. It passes by bending slightly in an S-shape. Between the temporomandibular joint and the external auditory canal, the superficial temporal artery, a. temporalis superficialis, and medially from the temporomandibular joint the external carotid artery passes through the maxillary artery, a. maxillaris. The largest branches of the external carotid artery are: the occipital artery, a. occipitalis; cranial laryngeal artery, a. laryngea cranialis, ascending pharyngeal artery, a. pharyngea ascendens; lingual artery, a. lingualis; facial artery, a. facialis; caudal auricular artery, a. auricularis caudalis; artery of the parotid gland, a. parotidea
Occipital artery, a. occipitalisi, begins slightly cephalad to the origin of the internal carotid artery and in the dog is slightly thinner than the latter. It passes in the dorsal direction caudo-medially from the digastric muscle and laterally from the initial sections of the vagus and glossopharyngeal nerves, while being in close contact with the cranial end of the large medial retropharyngeal lymph node. In addition to branches into the surrounding muscles, the condylar artery departs from the occipital artery, a. condylaris, penetrating into the cranial cavity through the canal of the hypoglossal nerve. At the level of the mastoid process, the occipital artery in the dog gives off the small caudal meningeal artery, a. meningea caudalis, which enters the dura mater of the brain through the foramen supramastoideum. The terminal branches of the occipital artery anastomose with the terminal branches of the vertebral artery and, thus, participate in the vascularization of the central nervous system.
Small cranial laryngeal artery, a. laryngea cranialis, emerges from the ventral wall of the external carotid artery. It gives off the pharyngeal branch, ramus pharyngeus, to the caudal constrictors of the pharynx and the laryngeal branch, ramus laryngeus, which enters the larynx through the rostral thyroid notch and participates in the blood supply to the mucous membrane and internal muscles of the larynx.
Ascending pharyngeal artery, a. pharyngea ascendens, with its numerous branches covers the lateral and dorsal walls of the pharynx and reaches the base of the skull. In the dog, it forms an anastomosis medial from the auditory tube with the rostral loop of the internal carotid artery. In the cat, the ascending pharyngeal artery connects with the vestigial internal carotid artery before the latter enters the jugular foramen. Thus, this vessel is also involved in the blood supply to the brain.
Lingual artery, a. lingualis, arises from the ventral wall of the external carotid artery, passes along with the hypoglossal nerve parallel to the stylochoid in the ventral direction and bends rostrally in the region of the keratochioid. From this place it runs as the deep lingual artery, a. profunda linguae, towards the tip of the tongue, curving and forming loops between the genioglossus and hyoglossus muscles. Not far from the beginning, the ascending palatine artery departs from the lingual artery, a. palatina ascendens, which vascularizes the palatine tonsil from the caudolateral side and the palatine palatine with several branches. In addition to it, the sublingual intermaxillary branch, ramus mylohyoideus, departs from the lingual artery, which in cats periodically occurs only on one side.
Facial artery, a. facialis, begins at the level of the tympanic bulla and goes first medially from the styloglossus muscle. Next, it passes in the vascular notch between the ventral edge of the mandibular bone and the insertion of the digastric muscle in the lateral direction and reaches the facial surface of the head. Its terminal division into the inferior labial artery, a. labialis inferior, angular artery of the mouth, a. angularis oris, superior labial artery, a. labialis superior, and the angular artery of the eye, a. angularis oculi, occurs rostrally from the anterior edge of the masticatory muscle. In the area of the larynx, the facial artery gives off a glandular branch, ramus glandularis, to the mandibular salivary gland, the sublingual artery a. sublingualis, as well as several branches - their number may vary - into the surrounding muscles. On the facial surface, a branch of the large masticatory muscle, ramus massetericus, departs from the facial artery into the corresponding muscle; numerous anastomoses are formed with the transverse artery of the face, as well as with the masticatory artery, which arises from the deep temporal artery.
In a cat, a branch of the large masseter muscle extends into the larynx, and the glandular branch additionally supplies the sublingual salivary gland with blood.
Origin of the hypoglossal artery, a. sublingualis, from the facial artery, located approximately 5 mm ventral to the mandibular foramen. It passes dorsally from the digastric muscle and lateral from the styloglossus muscle towards the floor of the mouth. The submental artery departs from it, a. submentalis, located ventral to the maxillohyoid muscle. The cat does not have the submental artery. The hypoglossal artery is not connected to the mylohyoid muscle; the corresponding area is vascularized by branches directed dorsally.
Rice. 3. Arteries of the head, A dog, B cat. Left side view (after Nickel/Schwarz, 1963)
1 a. carotis communis; 2 a. carotis interna; 3 a. occipitalis; 3′ ramus occipitalis; 4 a. condylaris; 5 a. stylomastoidea; 6 a. meningea caudalis; 6′ a. meningea media; 7 a. pharyngea ascendens; 8 a. palatina ascendens; 9 a. laryngea cranialis; 10 a.m. carotis externa; 11a. lingualis; 12 a.m. profunda linguae; 13 a.m. sublingualis; 14 a.m. submentalis; 16 a.m. facialis; 17 a.m. labialis inferior; 18 a.m. angularis oris; 19 a.m. labialis superior; 20 a.m. angularis oculi; 21 a.m. auricularis caudalis; 22 a.m. auricularis lateralis; 23 ramus auricularis intermedius; 24 ramus auricularis medialis; 25 a.m. auricularis caudalis; 26 a. temporalis superficialis; 27 a. transversa faciei; 28 ramus massetericus; 30 a.m. auricularis rostralis; 31 a. palpebralis inferior lateralis; 32 a. palpebralis superior lateralis; 33 a. maxillaris; 33′ rete mirabile a. maxillaris (cat); 34 a. alveolaris inferior; 35 rami dentales from a. alveolaris inferior to dentes incisivi; 36 rami mentales; 37 a. temporalis profunda caudalis; 37′ a. temporalis profunda rostralis; 39 rami retis (cat); 40 a.m. buccalis; 41 a. ophthalmica externa; 42 a. ethmoidalis externa; 44 a. lacrimalis; 45 a. ophthalmica externa, branching in bulbus oculi; 46 a. malaris; 47 a. palpebralis inferior medialis; 48 a. palpebralis superior medialis; 49 a. lateralis nasi; 50 a. dorsalis nasi; 51 a. infraorbitalis; 52 ramus alveolaris from a. infraorbitalis to dentes incisivi; 53 a. sphenopalatina; 54 a. palatina major; 55 a. palatina minor
Rice. 4. Semi-schematic representation of the most important cerebral arteries in a dog (after Seiferle 1992)
1 a. carotis communis dextra; 2 a. carotis externa; 3 a. occipitalis; 4 sinus caroticus; 5 a. carotis interna dextra, 5′ S-shaped loop, 5” a carotis interna sinistra; 6 a. intercarotica caudalis; 7 a. ophthalmica, ramus anastomoticus externa; 8 a. carotis interna, intracranial area; 9 a. intercarotica rostralis; 10 a.m. cerebn rostralis; 11 a communicans rostralis; 12 aa. corporis callosi; 13 a.m. ethmoidalis interna; 14 a.m. ophthalmica interna; 15 a.m. cerebri media; 16 aa. communicantes caudales; 17 aa. cerebri caudales; 18 aa. cerebelli rostrales; 19 a.m. basilaris; 20 aa. labyrinthi; 21 ax cerebelli caudales; 22 a.m. spinalis ventralis
Caudal auricular artery, a. auricularis caudalis, is the largest vessel of the auricle. Its initial area is completely covered by the parotid salivary gland. The branching pattern of the artery shows strong individual differences. At a short distance from its origin on the external carotid artery, the caudal auricular artery gives off the thin stylomastial artery, a. stylomastoidea, which branches in the middle ear, a large sternocleidomastoid branch, ramus sternocleidomastoid t'lis, for blood supply to the occipital muscles, as well as branches to the mandibular and parotid salivary glands. The auricle itself is supplied with blood by passing along the outer surface of the lateral, middle and medial branches, ramus auricularis lateralis, ramus auricularis intermedius and ramus auricularis medialis. Of these vessels, the largest and longest is the middle branch. All branches anastomose with each other and through holes in the ear cartilage give off numerous short branches to the inner surface of the auricle. Thin deep auricular artery, o. auricularis profunda, which is another branch of the caudal auricular artery, enters the inner surface of the external auditory canal from the medio-rostral side. It ends with the occipital branch, ramus occipitalis, which branches in the temporal and occipital muscles.