- What is atherosclerosis of the lower extremity vessels?
- Symptoms of the disease
- Risk factors
- Stages of development of atherosclerosis of the lower extremities
- Diagnostics
- Treatment
- Conservative treatment
- Surgical techniques
- Possible consequences and prevention
- Popular questions
Obliterating atherosclerosis (OA) of the arteries of the lower extremities
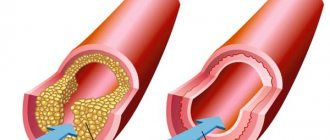
is a chronic vascular disease, which is based on lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of arterial walls and a decrease in the vascular lumen. As a result, ischemia develops - insufficient oxygen supply to cells and tissues.
Most often the popliteal, femoral and tibial arteries are involved in the pathological process.
OA of the arteries of the lower extremities is in first place among diseases of the peripheral arteries of atherosclerotic origin. According to literature data, obliterating arterial diseases account for about 16% of all vascular diseases Source: Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. .
Symptoms of atherosclerosis of leg vessels
The development of the disease occurs gradually and in the first stages there may be nothing to show for it. Subsequently, the patient develops pain in the lower extremities, especially with prolonged walking, and a feeling of numbness in the feet. A decrease in temperature is felt on the legs, pallor and cyanosis are visible, and cramps occur. Over time, a person develops intermittent claudication and trophic changes occur in the form of delamination of nails and the formation of ulcers on the fingers and heels.
- with atherosclerosis, the patient may feel and observe the following:
- muscle pain in the legs, in the later stages even the feet hurt, and the pain cannot be relieved with painkillers;
- limited mobility of the affected leg;
- pain along the affected artery - first during physical activity, then at rest;
- intermittent claudication - after walking some distance, a person is forced to stand up and give his legs a rest, and then he moves on until the next attack of weakness;
- tingling, numbness in the affected area;
- thickening of nails;
- loss or slow growth of hair on the legs;
- paleness when raising the legs and sharp redness when lowering them;
- rapid freezing of feet;
- sores on the skin;
- purple fingers;
- absence of pulsation in the affected artery;
- areas of darkening on the skin are signs of the onset of gangrene in advanced stages;
- coldness of the skin of the leg;
- reduction in the mass and volume of the muscles of the thighs and legs.
At the beginning of the disease, as a rule, one limb suffers, then the process becomes symmetrical - this is a signal that the arteries are affected on both sides. An objective examination reveals the absence of pulsation in the popliteal fossa, thigh and ankle.
Causes of the disease
The main reason for the development of this pathology is a violation of lipid metabolism in the body, which can be provoked by the following factors:
- Hypertonic disease;
- Obesity;
- Addiction to alcohol, smoking;
- High blood cholesterol levels;
- Constant stress;
- Genetic predisposition;
- Previous infectious diseases;
- Pathological processes in the endocrine glands.
Any of these reasons does not mean that atherosclerosis will necessarily develop in you, however, the listed factors, especially in combination, increase the risk of atherosclerosis several times.
Risk factors
The development of OA is based on the following most significant risk factors, the degree of influence of which can be different Sources: 1. Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. 2. Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. 3. Fattakhov V.V. Obliterating atherosclerosis of the lower extremities in the practice of a polyclinic surgeon / V.V. Fattakhov // Practical medicine. - 2010. - No. 2 (41). — P. 126-130. :
- male gender (men get sick 10 times more often);
- age (over 40 years);
- poor nutrition;
- overweight (obesity);
- smoking tobacco;
- hypokinesia (insufficient motor activity);
- hypofunction of the thyroid and gonads;
- heredity;
- some concomitant diseases (diabetes mellitus, coronary heart disease, heart rhythm disorders, lipid and carbohydrate metabolism, hypertension);
- exposure to adverse environmental factors.
City Hospital reports!
Obliterating atherosclerosis, causes
Obliterating atherosclerosis is the appearance of cholesterol plaques in the thickness of the walls of the arteries, leading to narrowing and blockage (obliteration) of the artery and disruption of the blood supply to the organ or tissue that the altered artery supplies.
Atherosclerotic plaques can occur in any arteries of the human body, including those found in the arteries of the lower extremities. This leads to the development of a disease - obliterating atherosclerosis of the lower extremities.
The occurrence of atherosclerotic plaques occurs due to many reasons. The role of metabolic disorders in this process, in particular disorders of fat metabolism in the body, is important. Genetic predisposition to this disease also plays a role, as well as such important factors as smoking, diabetes, poor diet, sedentary lifestyle, obesity, high blood cholesterol, and arterial hypertension. Among patients with obliterating atherosclerosis of the lower extremities, men significantly predominate.
According to the Ministry of Health of the Russian Federation, 5-15% of the population suffers from chronic obliterating diseases of the lower extremities.
The main age of patients with obliterating atherosclerosis of the lower extremities is 60-69 years in men, 70-79 years in women, but atherosclerosis has recently become rapidly “younger”.
Symptoms of obliterating atherosclerosis of the arteries of the lower extremities
The most common symptom of atherosclerotic lesions of the arteries of the lower extremities is intermittent claudication. Patients note pain, cramps, numbness that occurs when walking and goes away at rest, in the muscles of the thigh, gluteal region (high intermittent claudication), and lower leg (low intermittent claudication). This is a sign that at rest the muscles of the lower limb are sufficiently supplied with blood, and during physical activity the narrowed artery cannot deliver enough blood, and oxygen starvation occurs.
With further narrowing of the artery, up to its complete blockage (occlusion), pain begins to appear even with less load (a clear criterion is the distance traveled after which pain appears), then they continue to bother you even at complete rest. In this case, a lower position of the leg helps relieve pain. Pain at rest indicates a complete blockage of the artery; in this case, the blood supply is provided by collaterals - small arteries running in parallel, bypassing the blocked (occluded) artery.
With further aggravation of the condition, non-healing ulcers begin to appear on the skin, they gradually increase in size and deepen until they die completely - gangrene. Gangrene usually begins with the toes; in the absence of adequate treatment, the height of the spread of gangrene is determined by the level and degree of changes in the arteries.
One of the simplest and most objective studies of the extent of arterial damage is ultrasound duplex scanning of the arteries. Using an ultrasound sensor, you can see both the narrowed areas and the degree of their narrowing. When, due to the deterioration of the patient’s condition, it becomes clear that surgery is no longer possible, angiography is performed - an X-ray examination of the vessels through a puncture, using a catheter and a contrast agent.
Treatment of obliterating atherosclerosis of the lower extremities
Treatment tactics for each patient are developed individually and depend on the level, extent and extent of arterial damage, and the presence of concomitant diseases. However, there are general patterns that correspond to the severity of symptoms:
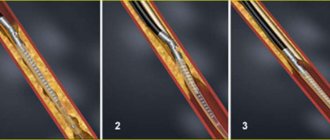
Intermittent claudication suggests the presence of a narrowed section of the artery. In most situations, endovascular treatment is effective: dilatation or stenting of a narrowed arterial vessel.
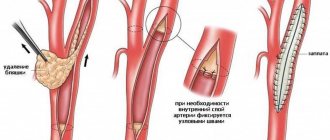
For pain at rest, it is assumed that there is a completely blocked section of the artery with blood supply to the leg through collaterals. In this case, endovascular treatment is used if it is possible to pass a catheter through the blocked area - which is often only possible with small blockages (occlusions). For long occlusions, surgical treatment methods are more applicable: open removal of atherosclerotic plaques (endarterectomy), or replacement of the affected area with a vein or tissue prosthesis (bypass surgery). In case of multiple lesions, combined operations are often used - bypassing the occluded section of the artery and dilatation (or stenting) of the narrowed one.
The presence of ulcers or gangrene is a sign of extensive arterial occlusions, multi-level lesions of arteries with weak collateral blood flow. Surgical treatment options in this case are reduced. Endovascular treatment can be used in combination with open surgery. If it is impossible to perform arterial reconstruction, or if it is ineffective, amputation of the affected limb is performed.
Important! The smaller the atherosclerotic damage to the artery, the simpler, more successful and cheaper the treatment. Therefore, the most favorable stage for treatment of obliterating atherosclerosis of the lower extremities is the stage of intermittent claudication.
If the described symptoms occur, urgent consultation with a vascular or endovascular surgeon is necessary. By postponing the start of treatment “until better times,” you contribute to the progression of the disease and increase the likelihood of amputation in the near future.
Endovascular treatment of obliterating atherosclerosis of the arteries of the lower extremities
In the cath lab, under completely sterile conditions, the endovascular surgeon punctures the femoral or other artery and inserts a catheter into the artery. The catheter is brought to the affected arterial area, a contrast study is performed - angiography, which makes it possible to clarify the extent and degree of narrowing (occlusion). A conductor is passed through the affected area - a metal string with a soft tip. A catheter balloon is installed along the guide into the affected area - a catheter with a plastic balloon inflated under high pressure to a strictly defined diameter. Then the balloon is inflated (dilated) at the site of narrowing. In this case, atherosclerotic plaques are pressed into the artery wall and smoothed out evenly, the lumen of the vessel increases. Control angiography is performed. If restoration of arterial patency is satisfactory, the procedure is completed. If a narrowed or closed area remains (elastic narrowing, external compression, bending), a stent is installed at the site of the lesion - a mesh metal structure, expanded by a balloon and reinforcing the lumen of the artery from the inside, preventing it from collapsing. After the patency of the artery is restored, the endovascular instruments are removed from the artery, the puncture site is pressed with a hand for 5-10 minutes (until bleeding from the puncture site stops), then a pressure bandage is applied and bed rest is prescribed until the next morning. Anticoagulants (heparin, fraxiparin, clexane) can be prescribed for several days, after which the patient continues to take the long-term antiplatelet agent prescribed for this disease (thrombo-ASA, aspirin-cardio, cardiomagnyl, cardio-ASA).
results
Immediately after restoration of arterial patency, the volumetric velocity of blood flow in the arteries of the limb increases, and the pulse is restored in the underlying arterial segments. If a limb has been left for a long time under conditions of insufficient blood supply, restoration of blood flow can lead to the so-called hyperperfusion/reperfusion syndrome. Unusually high blood flow causes redness of the limb, swelling, and sometimes pain. This condition goes away after a few days, after the limb “gets used” to the new conditions of blood supply.
Side effects, complications, relapses
In the presence of arterial lesions of both lower extremities, restoration of blood flow in one of them can lead to depletion of blood flow in the other. As a result, after surgery, intermittent claudication may appear on a limb that was previously considered healthy (which is a manifestation of the presence of previously undiagnosed obliterating atherosclerosis in it). Therefore, it is important to initially examine both limbs, even if painful symptoms are present on only one side.
The most common complication during endovascular interventions is puncture site hematoma. This complication does not require additional hospitalization; in the vast majority of cases it is treated conservatively.
Complications at the site of arterial damage (arterial thrombosis, partial or complete rupture of the artery) are relatively rare, their frequency depends on the experience of the surgeon, the quality of equipment, instruments and the severity of arterial damage. For example, the presence of calcification (long-existing arterial plaques accumulate calcium) increases the likelihood of rupture of the arterial wall when it dilates. In most cases, such complications can be eliminated endovascularly, or, if necessary, with open surgery.
Re-emergence or worsening of symptoms of arterial insufficiency can be caused by repeated narrowing of the dilated arterial segment or growth of the intima (inner lining of the artery) at the site of the stent. In this case, repeated endovascular interventions are performed, and if they are ineffective, surgical treatment is performed. However, most often, repeated narrowing of the arteries of the lower extremities is associated with the progression of atherosclerosis.
Continued growth of atherosclerotic plaques may create the need for repeated endovascular or surgical interventions. Therefore, it is especially important for patients with obliterating atherosclerosis to correct risk factors for the progression of atherosclerosis: strive to normalize blood pressure and blood cholesterol levels, quit smoking, follow a certain diet, change the mode of physical activity - that is, completely, sometimes radically change their lifestyle. All this is necessary in order to stabilize and slow down the further development of atherosclerosis. Only in this case, the results of any treatment for arterial insufficiency of the lower extremities will be long-term.
Clinical cases
Clinical case No. 1
A patient complained of intermittent claudication and pain in both legs occurred at a walking distance of 50 m.
The angiogram shows pronounced stenoses of the common iliac arteries on both sides (Fig. 1).
Balloon-expandable stents were installed into the areas of stenosis under local anesthesia through radial access (puncture on the forearm) (Fig. 2 and 3).
rice. 1 pic. 2 fig. 3
Stenoses were completely eliminated (Fig. 4).
Pain in the legs with minimal exertion no longer bothers the patient.
The pain-free walking distance has increased significantly.
rice. 4
Clinical case No. 2
A patient with diabetes mellitus complained of a non-healing trophic ulcer on the foot, in the bed of the removed 3rd toe (the toe was removed at the place of residence due to its gangrene), incipient gangrene of the 1st and 2nd toes of the right foot.
The angiogram shows occlusion of one of the tibial arteries at the level of the right ankle joint, its subocclusion in the lower third of the leg; the blood supply to the foot is provided by a single artery (Fig. 5).
rice. 5 (before intervention) Fig. 6 fig. 7
rice. 8 fig. 9
Balloon angioplasty of the arteries on the leg and foot was performed (Fig. 6, 7, 8, 9).
The main blood supply to the foot has been completely restored (Fig. 10 - angiogram of the right foot and lower third of the leg). Good conditions have been created for the healing of fingers and trophic ulcers. See photos of the foot before, one month, 3 months after angioplasty (the initially long-term non-healing bed after removal of the gangrenous toe quickly healed after angioplasty; the incipient gangrene of the 1st and 2nd toes was stopped - the toes were completely healed).
rice. 10
Photo of the foot before angioplasty Photo of the foot 1 month after angioplasty
Photo of the foot 3 months after angioplasty
Clinical case No. 3
The patient was admitted with critical ischemia of the only left lower limb due to acute thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color). In 2010 he had already been admitted with a similar condition of the right lower limb, when, despite the full scope of treatment, including a thrombectomy (removal of blood clots) performed by a vascular surgeon called from the republican hospital, gangrene of the limb eventually began to develop, and it had to be amputated.
In the present situation, clinical thrombosis of the arteries of the limb occurred 2 weeks ago, but the patient presented only 2 weeks later as a result of progressive deterioration of the limb.
The angiogram shows thrombotic occlusion of the arteries of the limb below the level of the inguinal fold (Fig. - top row). The patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through radial access (wrist puncture) and lowered into the left lower limb to the level of thrombosis. The thrombolytic drug was administered for 1 day. Despite the 2-week period of thrombosis, the blood clots were completely dissolved, and the main blood supply to the limb was completely restored (Fig. - bottom row). The patient's complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 4
Similar example. The patient was admitted with critical ischemia of the left lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marble-colored).
Clinically, thrombosis of the arteries of the limb also occurred 2 weeks ago, but the patient came only 2 weeks later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows occlusion of the arteries of the limb below the level of the knee joint ( Fig. - top row ). Over the course of 1 day, the patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through an access on the wrist and lowered into the left lower limb to the level of thrombosis. This method of treatment made it possible to completely dissolve blood clots, despite the 2-week period of thrombosis, the main blood supply to the limb was completely restored ( Fig. - bottom row ). As a result, the patient's complaints resolved completely. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 5
The patient was admitted with critical ischemia of the right lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color).
In the present situation, clinical thrombosis of the arteries of the limb occurred 3 days ago, but the patient came only 3 days later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows a short occlusion of the femoral artery above the level of the knee joint, occlusion of all arteries of the limb below the level of the knee joint ( Fig. - top row of photos ). The patient underwent selective thrombolysis through a catheter inserted under local anesthesia through radial access and reduced to the level of thrombosis in the right lower limb. The thrombolytic drug was administered for 1 day. Despite the 3-day period of thrombosis, the blood clots were dissolved, the main blood supply to the limb was restored, with the exception of the local area below the knee ( Fig. - second row of photos ). Balloon angioplasty of this area was performed, after which the main blood supply to the limb was completely restored (Fig. - third row of photos) . The patient’s complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 6
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee at a walking distance of 100 m. The angiogram shows a short occlusion of the right femoral artery at the level above the knee joint. Balloon angioplasty of the occlusion area was performed with good angiographic and clinical results. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty).
Clinical case No. 7
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee, and a progressive decrease in the pain-free walking distance. In the past, the patient underwent femoral-popliteal bypass surgery using his own vein. The angiogram shows critical stenosis of the shunt at the level above the knee joint. Balloon angioplasty of the area of critical stenosis was performed with a good angiographic and clinical result. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty). Angioplasty in this situation extended the life of the venous shunt and made it possible to avoid repeated open vascular surgery.
Clinical case No. 8
A patient complains of pain in the muscles of the right leg below the knee. The angiogram shows chronic occlusion (blockage) of the popliteal artery. Recanalization and balloon angioplasty of the occlusion area were performed. However, the result of angioplasty was regarded as insufficient and the intervention was supplemented with stenting with good angiographic and clinical results. The rest pain disappeared. Also, after the intervention there was no intermittent claudication. Photo below: the progress of the surgical intervention (the first row of photos is the area of occlusion before and after angioplasty, the flexion test shows the absence of compression of the stent when bending the knee joint; the following photos show blood flow below the knee joint before and after intervention).
Endovascular treatment of obliterating atherosclerosis. conclusions
Steady progress in manufacturing technologies for endovascular instruments, the emergence of new devices, improvement of catheterization techniques and the emergence of new treatment methods in recent years have led to a significant expansion of indications for endovascular reconstructive operations on the arteries of the lower extremities, improved treatment results and reduced the number of complications and relapses.
The experience accumulated by specialists allows us to recommend endovascular methods for the treatment of obliterating atherosclerosis to everyone who is faced with the problem of choosing a method of treating this disease.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC:
Tel.
Email mail
Ivanov Andrey Gennadievich (head of the department of x-ray surgical methods of diagnosis and treatment, doctor of the highest category in the specialty “endovascular diagnostics and treatment”)
Stages of development of atherosclerosis of the lower extremities
The most detailed is the modified classification of chronic arterial insufficiency of the lower extremities (CANF), which takes into account in detail the phenomena of critical limb ischemia, which is necessary when determining treatment tactics.
| Stage 1 | Muscle pain only during heavy physical activity (when walking over a distance of more than 1 km). Initial signs of stenosis appear - the skin turns pale, there is a feeling of goosebumps, it seems that the legs are always cold, fatigue quickly sets in when walking, excessive sweating is observed |
| Stage 2A | Feeling of fatigue and stiffness in the calf muscles, intermittent claudication after 200-1000 m |
| Stage 2B | Intermittent claudication in less than 200 m |
| Stage 3A | Intermittent claudication after a few steps or pain at rest when it is possible to keep the lower limb in a horizontal position for more than 2 hours |
| Stage 3B | Pain at rest, ischemic edema, inability to keep the lower limb in a horizontal position for 2 hours |
| Stage 4A | Gangrene of the fingers or part of the foot with the prospect of maintaining the supporting function of the limb |
| Stage 4B | Extensive necrotic changes in the limb without the possibility of maintaining its supporting function |
Diagnostics
There is a standard diagnostic program for this disease:
- Ultrasound of vessels of the lower extremities (duplex and Doppler scanning);
- coagulogram (determination of the blood coagulation system);
- determination of cholesterol and LDL levels in the blood;
- leg arteriography;
- establishment of pulsation in peripheral arteries;
- MR, MSCT angiography.
If prescribed by a doctor, MRI and CT scans with contrast and rheovasography can be performed.
To make a timely diagnosis of atherosclerosis of the vessels of the lower extremities, consultation with a vascular surgeon or phlebologist and a number of diagnostic measures are necessary.
Due to the systemic nature of the atherosclerotic process, patients with OA of the lower extremities often experience combined damage to various arterial basins, therefore, in such patients, an integral part of instrumental diagnosis is the study of extracranial and coronary arteries. Identification of pathology in them may require a change in treatment tactics or the order of surgical interventions Source: Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. .
Diagnostic measures
The presence of a specific pathology, as well as its exact cause, can only be determined during a face-to-face consultation with a specialist. During it, the doctor will ask several general questions regarding lifestyle and chronic diseases, study the medical history in detail, conduct some functional tests, and clarify the presence of similar pathologies in close relatives. As part of the examination, the doctor will ask you about the frequency and intensity of your symptoms, monitor your clinical picture, and identify the suspected etiology of the disease.
If suspicions are partially confirmed, you will be prescribed simple tests:
Rheovasography (RVG) is a non-invasive functional method for assessing pulse blood supply to the extremities, as well as the tone, elasticity and patency of peripheral vessels using a specific device;
Measurement of the brachial-ankle index - a one-time determination of the level of blood pressure in the area of the shoulders and ankles (normally it is the same);
Biochemical blood test (cholesterol content), and other tests to detect cardiac dysfunction.
For a more in-depth study of the course of the disease, the following measures are taken:
1. Duplex scanning of arteries and veins;
2. Angiography using a contrast agent;
3. Magnetic resonance angiography;
4. Multislice computed tomography of the lower extremities;
5. Functional tests.
Treatment of atherosclerosis of the vessels of the lower extremities
The approach to treatment is determined depending on the stage of the disease and is primarily about choosing the right regimen. It is necessary to adhere to a diet limiting fried and fatty foods, eliminating smoking and alcohol, as well as combating excess weight. The patient should follow a walking and physical activity regimen, choose comfortable and spacious shoes, and treat even the smallest injuries on the skin of the lower extremities. Treatment of concomitant chronic diseases is mandatory.
Medicinal methods include anticoagulants, antiplatelet drugs, agents that improve blood microcirculation, vasodilators, and physiotherapeutic procedures.
In severe cases, surgical treatment may be necessary.
General recommendations:
- normalize weight;
- follow a diet with low cholesterol;
- give up alcohol and smoking;
- wear shoes that fit;
- do not overcool your feet;
- even minor injuries should be carefully treated and treated;
- trim nails carefully without damaging soft tissues;
- engage in moderate physical activity - walking, swimming, cycling or exercising on an exercise bike.
Mechanism of arterial damage
All of these reasons disrupt fat metabolism, namely the accumulation of low-density lipoproteins and triglycerides. These substances are normally carriers of molecules, but during illness they change, binding to antibodies, becoming accumulations of unnecessary reserves in cells.
The process intensifies with diabetes, hypertension, decreased thyroid function, gout, during menopause, and under the influence of stressful situations.
The other side is impaired utilization of lipoproteins by the liver. This depends on the loss of sensitivity of hepatocyte cells to the changed complexes. Nerve endings (receptors) do not recognize them, so they are not accepted for processing.
Heredity is explained by mutation of genes that control the fat metabolism of cholesterol compounds.
Treating atherosclerosis
- Shishkin A.A.
- Volkov A.M.
- Kabirov A.V.
- Baranov V.S.
Shishkin Andrey Andreevich
Candidate of Medical Sciences. Surgeon, proctologist, phlebologist at SM-Clinic. Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
Read moreVolkov Anton Maksimovich
Phlebologist, surgeon at SM-Clinic. Performs operations with a modern proprietary method of treating varicose veins using a laser (modified endovenous laser coagulation. M-EVLC).
Surgical treatment of varicose veins of any complexity (phlebectomy, miniphlebectomy) More detailsKabirov Alexander Vitalievich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
More detailsBaranov Vladimir Sergeevich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Treats lower varicose veins using non-surgical and surgical methods (aesthetic sclerotherapy, ECHO sclerotherapy, stem sclerotherapy, phlebectomy, miniphlebectomy, EVLT).
More details
Medicines and their action
To relieve pain, use:
- painkillers;
- novocaine blockades (intraarterial, paravertebral at the level of 2–3 lumbar vertebrae).
Vasospasm is relieved with No-shpa, Halidor, Nicotinic acid, Hexonium.
To prevent thrombosis, Trental, Pentoxifyline, Agapurin, and the aspirin group are used.
In hospital settings, Trental is administered intravenously by drip, then tablets are prescribed in a maintenance dosage
Indirect anticoagulants (reduced blood clotting) are prescribed.
You can stimulate metabolism in tissues with vitamins, Solcoseryl, Parmidine, Prodectin.
The antioxidant effects of vitamins A, C, E, and Probuctol are used.
To restore protective forces, immunomodulatory drugs, ultraviolet irradiation of blood, and hemosorption are used.
Taking into account the autoimmune component in the pathology, desensitizing drugs are prescribed (Pipolfen, Diphenhydramine, Loratadine).
If the diet continues to maintain high levels of lipids in the blood, medications are prescribed to eliminate excess cholesterol.
This is what a removed blood clot looks like along with cholesterol plaques during atherectomy surgery
Conservative treatment
The patient may be prescribed various medications:
- prevent the formation of blood clots, prevent stroke and heart attack;
- increasing physical activity, improving blood flow in the lower extremities;
- antiplatelet drugs that lower blood cholesterol levels;
- anticoagulants, which prevent blood clotting in blood vessels and prevent blood clots;
- antispasmodics to relieve pain and spasms;
- antimicrobial ointments that need to be used to treat trophic ulcers;
- medications that promote better tissue nutrition;
- vasodilators;
- vitamins.
Also, as part of conservative therapy, physiotherapy is performed - electrophoresis with novocaine, darsonvalization, hyperbaric oxygenation.
What do diseased leg arteries “look like” from the inside?
Plaques form more often in places of greatest blood flow pressure, in the area of vascular branches. From the inside, the artery wall is yellowish in color, dense, elasticity is lost, deformation and deposition of calcium salts are possible.
The femoral and popliteal arteries have five types of lesions according to location and extent:
- type 1 - limited areas of narrowing (occlusion) in individual segments;
- type 2 - widespread changes in the entire surface of only the external femoral vessel;
- type 3 - widespread occlusion of the external femoral and popliteal arteries, but preservation of patency at the site of the fork of the popliteal branch;
- type 4 - obliteration of the superficial femoral and popliteal arteries in combination with the level of the fork of the popliteal branch, but with preserved patency of the deep femoral artery;
- type 5 is the most severe lesion, since there is narrowing at the level of the superficial, deep femoral and popliteal arteries.
In combined lesions of the arterial vessels of the leg with the popliteal, 3 types are distinguished:
- type 1 - with complete obliteration of the popliteal segment and the initial parts of the tibial arteries, patency in the middle and lower part of the leg is preserved;
- type 2 - narrowing at the level of one or two arteries of the leg, but there is blood flow in the lower part of the popliteal and tibial arteries;
- type 3 - patency is preserved only at the level of small branches on the legs and feet.
Progressive atherosclerosis causes ulceration of the plaque with tissue breakdown. The detached masses migrate to more distant areas of the legs, cause thrombosis, and impair blood circulation.
Another outcome is the formation of an aneurysmal sac, thinning of the wall and internal bleeding from the damaged vessel.
Surgical techniques
Surgery is a last resort and is usually prescribed for severe ischemia and very severe complications. Nowadays, different types of surgical interventions are performed. Some involve a day hospital, some require a long-term hospital stay under observation. Patient rehabilitation plans and post-operative care vary. Our doctors advise patients in detail on all aspects related to surgical intervention and carefully monitor their health in the pre- and postoperative period.
Surgical treatment of atherosclerosis of the lower extremities:
- bypass surgery - an additional “bypass” path for blood flow is created around the area of narrowing of the artery;
- stenting - a special tubular spacer is placed in the affected vessel, which ensures the required diameter of the artery;
- balloon angioplasty - similar to stenting, only a balloon is inserted into the vessel cavity rather than a spacer, which expands its lumen;
- autodermoplasty - if trophic ulcers are poorly treated conservatively, they are operated on and covered with the patient’s own skin;
- endarterectomy - removal of the affected part of the artery in which the atherosclerotic plaque is located;
- prosthetics – replacement of the affected vessel with the patient’s own vein, taken from another place, or with a synthetic prosthesis;
- amputation - prescribed in severe cases when gangrene occurs, after which prosthetics are performed.
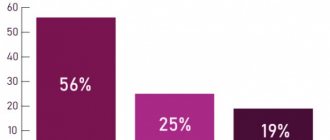
In 75-85% of cases, after surgery, blood circulation is completely restored for an average of 5-8 years.
Indications for surgery:
- an aneurysm that may rupture;
- chronic ischemia of critical stage;
- hemodynamically significant carotid artery stenosis or plaque accompanied by symptoms of cerebral ischemia;
- decompensation of blood circulation in the leg due to embolism, trauma, thrombosis.
Contraindications to surgical treatment:
- wet gangrene with sepsis;
- severe disruption of vital organs - renal and liver failure, circulatory disorders in the brain, myocardial infarction, heart failure, etc.
Diagnosis of occlusive lesions of the abdominal aorta
Diagnosis of occlusive lesions of the abdominal aorta. Angiographic semiotics of occlusive-stenotic lesions of the abdominal aorta is determined by the morphology and localization of the process in its wall. The most common acquired diseases of this localization are atherosclerosis and nonspecific aortoarteritis; congenital - hypoplasia and fibromuscular dysplasia. For atherosclerotic lesions of the abdominal aorta, localization distal to the renal arteries is typical. Atherosclerotic changes in the aortoiliac segment usually have a typical picture: plaques are most often located along the posterior wall of the aorta and iliac arteries. The bifurcation of the abdominal aorta is most often damaged. The iliac arteries are most often affected at the origin of the internal iliac artery. This must be kept in mind when planning the volume and extent of angiographic examination - from the interrenal abdominal aorta to the popliteal arteries - and when interpreting the angiographic picture.
The development of atherosclerotic lesions of the aortic wall and its branches is characterized by several stages. The earliest signs are elongation and curvature of the abdominal aorta and iliac arteries, often with an S-shaped curvature of the latter. Other early signs of atherosclerosis are a decrease in the degree of contrast along the edges of blood vessels and the appearance of small marginal “filling defects.” Further progression of the atherosclerotic process leads to the appearance of large marginal and; the contours of the aorta and iliac vessels become uneven, broken, and scalloped. With advanced atherosclerosis, a break in the shadow of the vessel is detected - occlusion, which can be limited (segmental) and widespread. Occlusion is characterized by the presence of a stump of the affected vessel, the shape of which can be very diverse. Occlusion of the abdominal aorta is characterized by a cylindrical and conical stump; for occlusion of the common iliac artery - a conical stump and a stump in the form of an oblique cut; with occlusion of the external iliac artery, only a conical stump is found. An important sign that this break in the shadow of a contrasting vessel is a true stump is the presence of dilated collateral vessels extending from sections of the arterial trunk located above the break area. Isolated occlusions of arterial vessels are quite rare. More often there are combined lesions of the aorta, iliac and femoral arteries and their branches. An important indirect sign of atherosclerotic lesions of the aorta and its branches is calcification of the vessel walls.
However, there is no direct parallelism between the degree and prevalence of calcification of the vascular walls and the narrowing or occlusion of their lumen. When analyzing angiograms, one should distinguish between stenotic lesions of the abdominal aorta and unilateral stenosis or occlusion of the iliac arteries and lesions of the bifurcation of the abdominal aorta and both iliac arteries - Leriche syndrome. In this case, assessment of collateral circulation pathways is very important. With high occlusions of the abdominal aorta (above the level of the inferior mesenteric artery), the pelvic arteries are contrasted by a roundabout blood supply through a system of visceral collaterals: the superior mesenteric artery and its connection with the branches of the inferior mesenteric artery (interarterial arch of Riolan), which in turn are connected with a.hypogastrica. The branches of the latter anastomose with the branches of the femoral artery and the deep artery of the femur. With low occlusion of the aorta (below the inferior mesenteric artery), both visceral and parietal collaterals participate in the circuitous blood supply. The main pathways are the branches of the inferior mesenteric artery and their connections with the arterial plexus around the rectum, as well as the lumbar arteries and their connections with a.hypogastrica. In the description of occlusive-stenotic lesions of the pelvic arteries, it is necessary to indicate the degree of damage to the common iliac arteries, separately the degree of damage to the internal iliac arteries and the condition of the distal vascular bed (external iliac, femoral, popliteal artery and vessels of the leg). With occlusion of the common iliac artery, the collaterals are close to those that form during occlusion of the abdominal aorta. However, here the parietal blood supply routes - the lumbar arteries and their anastomoses - are of greater importance; to a lesser extent - the system of the inferior mesenteric artery.
When the external iliac artery is blocked, the main collateral artery is the a.hypogastrica, the branches of which anastomose with the branches of the femoral artery and the deep femoral artery. When the femoral artery is occluded in its upper and middle thirds, it is very important to assess the patency of the deep femoral artery as the main collateral. It is generally accepted that if, according to angiographic data, the deep artery is patent to the second perforating branch, it is suitable for aortofemoral reconstruction. With segmental occlusion of the femoral artery in the area of the Gunter's canal, the main role of collaterals is played by the muscle branches extending from the artery above the site of occlusion. When the popliteal artery is blocked, anastomoses between the superior and inferior arteries of the knee joint are important. In general, it should be emphasized that even today, despite the successful development of the latest diagnostic methods for assessing the dynamics of blood supply in the main arteries of the extremities, only angiography allows for the most accurate and comprehensive assessment of the collateral bed that develops with occlusive lesions of the arteries of the pelvis and lower extremities.
In case of nonspecific aortoarteritis, a two-plane angiographic examination of the abdominal aorta is mandatory. It allows you to detect the main differences between macromorphological lesions of the aorta and its branches from atherosclerotic lesions. Atherosclerosis is characterized by more frequent damage to the abdominal aorta and the presence of local contrast defects at the site of atherosclerotic plaques. In aortoarteritis, the narrowing of the aortic lumen is of greater extent, and the localization of the lesion differs from that in atherosclerosis. The “favorite” sites of damage in aortoarteritis are the thoracoabdominal aorta, carotid arteries and distal segments of the subclavian arteries. When aortoarteritis affects the abdominal aorta, the orifice of the celiac and superior mesenteric arteries are usually involved. In no other occlusive process are the collaterals (Riolan's arch) as developed as in aortoarteritis. With celiac artery stenosis, there is an excess of the diameter of the common hepatic artery over the splenic artery due to the redistribution of blood flow (normally, on the contrary, the diameter of the splenic artery is larger). With complete occlusion of the celiac artery, there is no direct contrast. The contrast fills it after the branches of the superior mesenteric artery through the pancreatic duodenal and gastroduodenal arteries. This can be detected with selective mesentericography. Stenosis of the superior mesenteric artery is detected only in the lateral projection, since the narrowing is usually located within the first two centimeters from the mouth. Damage to the superior mesenteric artery is characterized by dilatation of the inferior mesenteric artery and the arch of Riolan. In this case, a sequential assessment of all frames of a series of angiograms makes it possible to notice that the blood flow along the Riolan arch goes in the cranial direction, and first the inferior, then the superior mesenteric artery is contrasted. Less commonly, a celiac-mesenteric anastomosis is detected, along which the contrast moves in the caudal direction. This can be detected with selective celiacography. When the inferior mesenteric artery is occluded, its contrast occurs due to the Riolan arc, which functions in this case in the caudal direction. In addition, a rectal-mesenteric anastomosis may be detected. With combined lesions of the celiac and superior mesenteric arteries, all blood flow goes in the cranial direction through the inferior mesenteric artery and the arch of Riolan. A narrow long arc of Riolan is typical for atherosclerosis. Aortoarteritis, on the contrary, is characterized by a wide and short Riolan arc. Based on the structural features of the Riolan arch, one can often judge the etiology of the lesion.
Branches of the abdominal aorta
Possible risks associated with the disease
The disease is insidious in that it is impossible to predict its course and symptoms. Approximately 20% of patients over 65 years of age, having severe plaques, do not feel any discomfort. The seriousness of the progressive course of OA ANC is also due to the fact that after the appearance of the first symptoms, 10-40% of patients develop gangrene within 3-5 years, which leads to amputation of a limb or death Source: Kazantsev A.V. A new approach to surgical tactics for obliterating atherosclerosis of the arteries of the lower extremities / A.V. Kazantsev, E.A. Korymasov // Saratov Medical Scientific Journal. - 2010. - T. 6. - No. 4. - P. 850-856. .
Atherosclerosis can be complicated by arterial thrombosis. This complication, if not immediately sought by a doctor, leads to loss of a limb or embolism of other arteries. If the clot detaches and enters the coronary artery, a myocardial infarction may develop, and if it migrates to the carotid artery, a stroke may occur.
What is non-stenotic arterial atherosclerosis?
Non-stenotic arterial atherosclerosis is a disease in which cholesterol plaques form on the inner surface of the vessels, but the deposits practically do not slow down the blood flow. These plaques have an elongated shape and are localized along the surface of the arteries, which is the main distinguishing feature from the stenotic form of atherosclerosis, in which calcifications grow into the lumen of the vessels and significantly impede blood flow.
A cholesterol plaque is a deposit of lipid tissue that becomes harder over time due to the deposition of calcium on its surface. With non-stenotic atherosclerosis, the formation can block the lumen of the vessel by no more than half.
This pathology begins to develop at a fairly young age and is asymptomatic for a long time, and only with progression can it manifest itself as a pathology of an organ that lacks nutrients due to poor blood circulation. As a rule, this happens after 50 years.
Prevention methods
For prevention purposes, you need to start controlling the levels of lipids, sugar and cholesterol in the blood as early as possible. Even with a slight increase in numbers relative to the norm, you should consult a doctor. It is also recommended to regularly do ultrasound of the lower extremities - once every 1-2 years.
It is important to watch your diet, because the reason for the increase in “bad” cholesterol in the blood is the saturated fats that we consume in food. These are products of animal origin - fatty meat, lard, butter. There is a lot of cholesterol in eggs, or rather in the yolks. All these products should be consumed in the smallest possible quantities.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Appointment (examination, consultation) with a cardiovascular surgeon, primary, therapeutic and diagnostic, outpatient | 1 750 | — |
| Program “Risk of atherosclerosis and ischemic heart disease, predisposition to dyslipidemia” | 19 000 | — |
* You can read more about the conditions here - Treatment on credit or in installments.
Aneurysms
Aneurysms of peripheral arteries are characterized by the appearance of pathologically dilated areas of the arterial wall, resulting from its weakening. As a result, the artery wall bulges and this condition can be complicated by thromboembolism, strokes, or, if the arterial wall is significantly thinned, ruptures.
About 70% of such aneurysms occur in the popliteal arteries, and 20% in the iliofemoral segment. Sometimes they are combined with abdominal aortic aneurysms, which in 50% of cases are bilateral. Typically, aneurysms of peripheral arteries are provoked by atherosclerosis and infectious diseases (in such cases, the protrusion is most often localized in the femoral artery). Sometimes the root cause of their occurrence is entrapment of the popliteal artery or septic emboli, leading to the formation of a mycotic aneurysm.
Peripheral aneurysms are often asymptomatic. In some cases they are manifested by the following symptoms:
- pain when palpating;
- pallor and coldness of the affected limb;
- sensitivity disorders;
- absence of pulse in the affected area due to thromboembolism or rupture of a pathological protrusion;
- pain, fever, general malaise (if the aneurysms are infectious).
The risk of artery rupture in the area of the aneurysm is low - no more than 5% for popliteal bulges and 1 - 14% for iliofemoral aneurysms.