General practitioner
Shekinah
Natalya Nikolaevna
15 years of experience
General practitioner
Make an appointment
While still at school, children learn about white blood cells and the importance of the many functions they perform in the body. However, an excess of even such useful enzymes in the blood can create health problems. What kind of disease is this in adults - leukocytosis?
Leukocytosis is a process of changes in the composition of the blood, which results in an increase in the number of leukocytes. For adults, the norm for leukocytes is considered to be 9000 in 1 μl of peripheral blood. Exceeding these values may indicate a problem. The changes that occur in the composition of the blood are the body’s protection against certain influencing factors. For specialists, an increase in the number of leukocytes becomes one of the important signs when diagnosing a number of pathologies.
Main causes of leukocytosis
There are many factors that can influence changes in blood composition. The following are various causes of leukocytosis in the blood in adults.
Often the disease is provoked by infections. One of the main functions of leukocytes is to maintain anti-infective immunity. Therefore, the appearance of foreign pathogens in the body leads to an increase in the number of white blood cells in the blood. Different types of pathogenic microorganisms provoke different types of leukocytosis.
With the bacterial type, the number of neutrophils and monocytes increases. Their action in fighting infections can be compared to an “oxygen explosion” that literally destroys hostile pathogens.
Viral infections provoke an increase in lymphocytes. This type of leukocyte produces specific antibodies to trigger the apoptosis mechanism in viral cells.
Helminthic infestations – the level of eosinophils changes. They contain a cationic protein that can act on helminths that have infected the body and negatively affect the metabolic processes within them.
The causes of leukocytosis can be systemic diseases:
- diffuse connective tissue diseases (for example, dermatomyositis or systemic lupus erythematosus);
- joint diseases (rheumatoid arthritis, etc.);
- systemic vasculitis (giant cell arteritis, nonspecific aortoarteritis).
The exact mechanism of leukocytosis in systemic diseases has not been established. Presumably, the production of leukocytes is provoked by cytokines and mediators that are formed during the process of rheumatic inflammation.
Allergies become the main cause of the development of eosinophilic leukocytosis.
Blood diseases - pathologies such as leukemia, polycythemia, lymphomas, cause the development of hyperleukocytosis. It develops against the background of oncological transformations occurring in bone marrow stem cells. As a rule, the result is severe acute leukocytosis.
Other causes of leukocytosis:
- endocrine type disorders;
- lesions that cause large-scale tissue destruction (for example, extensive burns);
- various types of toxic effects on the bone marrow;
- malignant neoplasms;
- primary immunodeficiency;
- diseases of the lungs and respiratory tract;
- diseases of dermatological type, etc.
Revealing
The syndrome may not have pronounced symptoms. If this form is mild, they will not exist at all. If the number of white blood cells decreases significantly, infectious pathologies will begin to develop.
One of the symptoms of the syndrome is a feverish state. This is due to infectious effects, the body’s reaction to chemotherapy drugs taken, or a tumor.
Among the symptoms of the syndrome:
- Feeling weak;
- State of dizziness;
- The mucous membranes bleed;
- Hemorrhages appear on the skin, some others.
Serious infectious consequences include sepsis and septic shock.
A low white blood cell count is detected by a blood test.
Pulmonary hemorrhage
Complications
Since this disease is not independent, it also cannot be a predictor of any complications or consequences. All consequences that occur in the patient (including death) are directly related to the disease against which leukocytosis developed. Therefore, a serious excess of any type of leukocytes in the blood is a reason to conduct an in-depth examination to find out the true cause. Such a need may arise even if a person feels absolutely healthy.
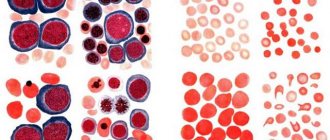
Structure
The structure of leukocytes of different types is different, and they look different. What they all have in common is the presence of a core and the absence of their own color. The cytoplasm can be granular or homogeneous.
Neutrophils
Neutrophils are polymorphonuclear leukocytes. They are round in shape and have a diameter of about 12 microns. There are two types of granules in the cytoplasm: primary (azurophilic) and secondary (specific). Specific small, lighter and make up about 85% of all granules, contain bactericidal substances, the protein lactofferin. Ausorophilic ones are larger, they contain about 15%, they contain enzymes, myeloperoxidase. In a special dye, the granules are colored lilac, and the cytoplasm is colored pink. The granularity is fine, consists of glycogen, lipids, amino acids, RNA, enzymes, due to which the breakdown and synthesis of substances occurs. In young forms, the nucleus is bean-shaped, in rod-nuclear forms it is in the form of a stick or a horseshoe. In mature cells - segmented - it has constrictions and looks divided into segments, which can be from 3 to 5. The nucleus, which can have processes (appendages), contains a lot of chromatin.
Eosinophils
These granulocytes reach a diameter of 12 microns and have a monomorphic coarse granularity. The cytoplasm contains oval and spherical granules. The granularity is stained pink with acidic dyes, the cytoplasm becomes blue. There are two types of granules: primary (azurophilic) and secondary, or specific, filling almost the entire cytoplasm. The center of the granules contains a crystalloid, which contains the main protein, enzymes, peroxidase, histaminase, eosinophil cationic protein, phospholipase, zinc, collagenase, cathepsin. The eosinophil nucleus consists of two segments.
Basophils
This type of leukocyte with polymorphic granularity has dimensions from 8 to 10 microns. Granules of different sizes are stained with a basic dye in a dark blue-violet color, the cytoplasm is stained pink. The grain contains glycogen, RNA, histamine, heparin, and enzymes. The cytoplasm contains organelles: ribosomes, endoplasmic reticulum, glycogen, mitochondria, Golgi apparatus. The core most often consists of two segments.
Lymphocytes
By size they can be divided into three types: large (from 15 to 18 microns), medium (about 13 microns), small (6-9 microns). The latter are in the blood most of all. Lymphocytes are oval or round in shape. The nucleus is large, occupies almost the entire cell and is painted blue. A small amount of cytoplasm contains RNA, glycogen, enzymes, nucleic acids, and adenosine triphosphate.
Monocytes
These are the largest white cells, which can reach a diameter of 20 microns or more. The cytoplasm contains vacuoles, lysosomes, polyribosomes, ribosomes, mitochondria, and the Golgi apparatus. The nucleus of monocytes is large, irregular, bean-shaped or oval, may have bulges and indentations, and is colored reddish-violet. The cytoplasm acquires a gray-blue or gray-blue color under the influence of the dye. It contains enzymes, saccharides, and RNA.
Classification of leukocytosis
A shift in leukocytosis does not always indicate a disease. According to biological characteristics, two types are distinguished:
- physiological leukocytosis;
- pathological increase in leukocytosis.
The physiological type is the norm of leukocytosis. It occurs in absolutely everyone and does not pose any danger. In certain circumstances, even a healthy person has moments in everyday life when an increase in white blood cells occurs. Factors influencing this physiological process may be different. For example, there is the concept of food reactive leukocytosis. As a rule, it occurs 2-3 hours after eating. Another common factor is playing sports or other intense physical activity. As a result of muscle work, the level of leukocytes temporarily increases. The physiological type of leukocytosis in women during pregnancy is a completely normal phenomenon during the second trimester of pregnancy.
Pathological leukocytosis in the blood develops against the background of diseases, therefore, correction of the level of leukocytes is carried out by treating the disease against which it developed.
The following types of leukocytosis are distinguished.
Depending on the degree of increase in the level of leukocytes:
- moderate leukocytosis - an increase in the level from normal to 15,000;
- high leukocytosis – level range from 15,000 to 50,000;
- hyperleukocytosis - the concentration level exceeds 50,000. This degree of the disease is characterized by the presence of a large number of unformed white cells;
By type of leukocytes that exceeded the norm:
- neutrophilic or neutrophilia. The excess of neutrophils is more than 75%. Changes can be provoked by suppurative processes, as well as various bacterial infections;
- lymphocytic or lymphocytosis. The level of lymphocytes exceeds 38% in adults (for children under 7 years of age, this figure is 55%). The cause may be lymphoproliferative diseases, as well as viral infections;
- monocytic or monocytosis. The level of monocytes exceeds 10%. Common causes include septic endocarditis, granulomatous processes, protozoal infections;
- eosinophilic or eosinophilia. Exceeding the norm is more than 5%. The cause may be allergic reactions, a number of lung diseases, helminthic infestations, etc.;
- basophilic or basophilia. Basophil level more than 1%. This shift in leukocytosis is very rare. Among the causes, experts identify nonspecific ulcerative colitis, polycythemia vera, and allergies.
Types of leukocytes
White cells are divided into two groups:
- Granular leukocytes - granulocytes. They contain large, irregularly shaped nuclei, consisting of segments, the more of which the older the granulocyte is. This group includes neutrophils, basophils and eosinophils, which are distinguished by their perception of dyes. Granulocytes are polymorphonuclear leukocytes. You can learn more about granulocytes from this article.
- Non-granular - agranulocytes. These include lymphocytes and monocytes, which contain one simple oval-shaped nucleus and do not have a characteristic granularity.
Symptoms and signs of leukocytosis
An increase in the level of leukocytes cannot be considered as an independent disease. It always develops against the background of another disease, and therefore does not have its own symptoms and clinical manifestations. Often, in the early stages, leukocytosis in men and women has no symptoms; a person may even think that he is completely healthy. However, there are a number of symptoms that you should pay attention to. Especially if a person cannot explain their nature, for example:
- elevated body temperature for a long time;
- frequent bruising and bleeding;
- general weakness, feeling of malaise;
- frequent dizziness or fainting;
- tingling and pain in the limbs;
- loss of appetite or weight loss for no apparent reason.
Are you experiencing symptoms of leukocytosis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
When to see a doctor
If you experience a general feeling of malaise or one of the symptoms described above for no apparent reason, you should consult a specialist. Such symptoms are characteristic of a large number of diseases and can also be a sign of leukocytosis. Therefore, you should contact a competent specialist for advice. JSC “Medicine” (clinic of Academician Roitberg) employs experienced specialists with extensive experience and high qualifications. The clinic is located in the center of Moscow: 2nd Tverskoy-Yamskaya lane, 10.
Diagnosis of leukocytosis
The diagnosis of leukocytosis is established based on the results of a clinical blood test. An appointment with a general practitioner takes place in two stages: taking an anamnesis and examining the patient. After analyzing the data obtained, the doctor prescribes additional studies to identify and confirm the disease that caused leukocytosis.
Let's consider the types of possible research.
- Detailed blood test and biochemical blood test. Leukocytosis is determined in the blood smear for the presence of toxic granularity of neutrophils, as well as atypical mononuclear cells.
- Detection of the pathogen using bacterial culture of blood, urine, and sputum. Identification of the pathogen will allow the exact cause to be determined and effective treatment to be prescribed.
- Allergy diagnostics. To confirm the allergic nature of leukocytosis, studies measure the level of immunoglobulin E using ELISA. Skin and provocative allergy tests may also be performed.
- Radiography. This method can be used to examine chest organs, joints, etc.
- Ultrasound. An effective diagnostic method for a large number of diseases. Ultrasound helps to identify, for example, an increase in the size of the kidneys, compaction of the pyelocaliceal system, it is also important for identifying vegetation on the valves, etc.
Research in our clinic is carried out using the most modern equipment, as quickly as possible.
Treatment of leukocytosis
Features and causes of appearance do not provide for symptomatic treatment of leukocytosis. Therapy is prescribed after the underlying disease has been established, the development and progression of which has provoked a jump in the level of leukocytes. Accordingly, treatment methods in each individual case will be very individual.
Antibiotics are used to treat infectious diseases. Steroid drugs can be used to eliminate inflammation. Reducing uric acid in the body with the help of special drugs helps prevent the destruction of body tissues, which can also cause leukocytosis, etc. When talking about the treatment of leukocytosis, we are talking about the disease that caused it.
At our multidisciplinary medical center, doctors prescribe safe and effective treatment using an individual approach and many years of experience.
Correction
Constitutional leukopenia does not require any intervention. If the development of this deviation is caused by a drug, its immediate discontinuation is necessary. With a pronounced decrease in leukocytes or agranulocytosis, they resort to the introduction of granulocyte colony-stimulating factor (G-CSF) or infusion of donor granulocytes. The main condition for successful therapy is treatment of the underlying pathology:
- Elimination of the pathogen.
Oseltamivir is used to treat influenza, and antiretroviral drugs (zidovudine, saquinavir) are used to combat HIV infection. For bacterial infections, antibiotics are prescribed. - Anti-inflammatory therapy.
To achieve remission of autoimmune diseases, glucocorticosteroids, immunosuppressants, and 5-aminosalicylic acid derivatives are used. - Chemotherapy.
If oncohematological pathology is confirmed, combinations of chemotherapeutic agents are prescribed - chlorambucil, vincristine, etoposide. - Bone marrow transplantation.
In case of ineffectiveness of chemotherapy for hematological malignancies, as well as in severe primary neutropenia, hematopoietic stem cell transplantation is performed.