Author:
Mironova Irina Sergeevna 5/5 (1 rating)
Honey. portal:
Causes Symptoms Complications Diagnostics Treatment Advantages of treatment at MGC Price of treatment Classification
Uveitis is a collective concept that covers inflammatory diseases of various parts of the choroid. The choroid (synonymous with the uveal tract) is represented by the anterior section (includes the iris and ciliary body) and the posterior section (the choroid itself - the choroid). Anatomically, these sections have separate blood supply and innervation, therefore the inflammatory process in the choroid is localized in most cases, although in some cases the entire uveal tract may be affected.
Classification
Uveitis is classified according to duration, predominant damage to one or another structure of the uveal tract, and also depending on the pathogen.
There are four types of uveitis depending on the location of the inflammation.
- Anterior uveitis is inflammation of the anterior part of the choroid, including iritis and iridocyclitis. This is the most common type of uveitis.
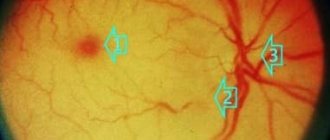
- Posterior uveitis (synonymous with choroiditis) is an inflammation of the posterior part of the choroid, in addition to the choroid itself, affecting the retina and optic nerve.
- Peripheral uveitis is a disease that affects the ciliary body, vitreous body, the choroid itself (choroid) and the retina.
- Panuveitis is a combined inflammation of all structures of the vascular tract.
Depending on the severity of the pathological development, uveitis can be acute or chronic.
Causes
Uveitis can be caused by factors and agents of different origins, which include:
- exogenous and endogenous infections;
- penetrating injuries and burns;
- infectious and allergic agents, immunodeficiencies and the autoimmune nature of the disease.
Main causes of uveitis
Most often, uveitis develops against the background of ankylosing spondylitis and Reiter's syndrome , toxoplasmosis (intrauterine infection), brucellosis , herpes simplex , influenza , meningitis , syphilis (in recent years - less and less), tuberculosis and sarcoidosis, and juvenile rheumatoid arthritis often causes bilateral chronic anterior uveitis, accompanied by the appearance of antinuclear antibodies and Russell bodies ( immunoglobulin in the iris).
In approximately 40% of patients, uveitis develops against the background of systemic diseases, and in 25%, the cause cannot be established, and therefore they speak of the idiopathic nature of the disease.
In recent years, scientists have been able to identify a genetic predisposition to uveitis. It is determined by the HLA genes -B27, -B5, -Bw22, -A29 and -D5. Anterior uveitis, associated with the presence of HLA-B27 in the bloodstream, develops 2.5 times more often in men than in women.
Symptoms
Depending on the location of the inflammatory process, the patient's complaints will be different.
With anterior uveitis, the leading symptoms will be redness of the mucous membrane of the eye, accompanied by lacrimation, photophobia, pain, a narrow pupil (miosis), blurred vision, and increased intraocular pressure.
Symptoms of posterior uveitis are usually mild and manifest themselves in the form of “floaters” before the eyes, the appearance of a veil, decreased vision, pain in the depths of the orbit and changes in the visual fields (if the optic nerve is involved in the pathological development).
With peripheral uveitis, the main manifestations will also be “floaters” in front of the eyes and blurred vision.
Patients with panuveitis may present with complaints characteristic of damage to one or another part of the uveal tract.
Consequences and complications
Severe trophic disorders, the action of toxins, epithelial lesions, pupillary fusion, congestion and exudation in the retina can lead to such serious consequences and complications as:
- clouding of the lens or in other words - cataract ;
- secondary glaucoma;
- atrophy of the eyeball;
- neuritis;
- exudative retinal detachment;
- band-shaped corneal degeneration.
Treatment of uveitis
The earlier the pathology is detected, and the more accurately the cause of the disease is established, the greater the chances of a positive outcome in the treatment of uveitis. The choice of treatment tactics depends on the characteristics of the disease in a particular patient. To stop the inflammatory process, local and general therapy is used (anti-inflammatory drugs, immunostimulants, pupil dilators, antibiotics, physiotherapy, etc.). A good effect for this disease is provided by the use of hirudotherapy (treatment with leeches), which is also used in our clinic. If intraocular pressure increases, antiglaucomatous drops are prescribed.
Diet for uveitis
Diet to boost immunity
- Efficacy: therapeutic effect after 3 weeks
- Terms: 1-3 months or more
- Cost of products: 1600-1800 rubles. in Week
If uveitis is non-traumatic in nature, then the severity of the course and the speed of development of pathogenesis directly depends on the state immunity . Therefore, to prevent uveitis, in addition to eye hygiene and regular examinations by an ophthalmologist, it is important to have a nutritious diet rich in vitamins (especially A and E) and foods that increase the body’s resistance. It is advisable to include in the diet:
- seafood, including cod and oysters;
- chicken eggs;
- nuts and seeds;
- carrots, apricots, citrus fruits and other orange fruits and vegetables;
- sprouted wheat, spinach and microgreens;
- Blueberries, which are also very good for vision, are rich in vitamin A and antioxidants .
Advantages of treatment at MGK
One of the most important factors for successful treatment of uveitis is early detection, the most accurate diagnosis and comprehensive treatment. By contacting the Moscow Eye Clinic, you can undergo a comprehensive and completely painless examination in a short period of time, comfortably. Based on the results of the examination, the doctor will select an individual treatment regimen.
Our clinic employs recognized domestic specialists who have extensive practical experience in successfully treating a wide variety of eye diseases. For those patients who require long-term treatment using injections, physiotherapeutic techniques, hirudotherapy, etc. A day hospital is available, which allows treatment under the supervision of experienced doctors. The clinic is open seven days a week, from 9 a.m. to 9 p.m.
Coloboma of the iris
| Typically, iris coloboma is located inferiorly at 06.00. clock, resembling a pear or a keyhole (see.
|
You can learn about plastic restoration of the pupil in our video
Install Flash Player to watch the movie.
Our licenses
Diagnostics
An eye examination performed by an ophthalmologist is painless and lasts a few minutes. Be sure to tell the doctor about the medications your child is taking.
Before examining the visual organ, the ophthalmologist applies drops to dilate the pupils. Dilation helps the doctor see the inside of the eyes.
To detect inflammation, the ophthalmologist uses a special microscope called a slit lamp. Shines a thin beam of light into one eye.
To detect changes in vision, a visual field examination and the following tests are performed:
- skin test;
- X-ray examination;
- optical coherence tomography.
If necessary, the child is referred to a rheumatologist. The doctor diagnoses autoimmune and inflammatory disorders associated with joints. These doctors know a lot about the immunosuppressive drugs that can be used to treat the disease and monitor potential side effects. The role of the rheumatologist is important in the care of patients with inflammatory eye diseases, so regular monitoring is necessary.
Prevention
Carefully following the doctor's recommendations and attending all scheduled appointments with the rheumatologist and ophthalmologist, your child's vision problems should be under control - the main preventive measures.
It is recommended to visit doctors regularly (every 3–6 months) to ensure that there are no changes in the condition of the optical system.
Prevention is as follows:
- proper hygiene;
- minimizing injury;
- strengthening the immune system with drugs and hardening;
- minimizing exposure to toxic substances.