Lipidogram
Interpretation of the results of the Lipidogram study
Interpretation of test results is for informational purposes only, is not a diagnosis and does not replace medical advice.
Reference values may differ from those indicated depending on the equipment used, the actual values will be indicated on the results form. Currently, the prognostic significance of the concentration of total cholesterol in the blood is undoubted in relation to the risk of mortality from major diseases associated with atherosclerosis (coronary artery disease and cerebral strokes). When the cholesterol level in the blood is below 5.2 mmol/l, the risk of developing atherosclerosis is the lowest. If the concentration of LDL cholesterol in the blood is below 2.59 mmol/l, atherosclerotic changes in the coronary arteries rarely occur.
An increase in LDL cholesterol above 2.59 mmol/l is observed when eating foods rich in animal fats and cholesterol. Physical inactivity, unbalanced nutrition, resulting excess body weight, smoking, arterial hypertension, diabetes mellitus are factors that increase the risk of coronary artery disease. The presence of at least two of the above factors accelerates the development of critical coronary atherosclerosis by approximately 10 years.
Reducing the concentration of total cholesterol in the blood and increasing HDL cholesterol reduces the progression of atherosclerosis. A 10% reduction in total cholesterol levels in the blood leads to a 20% reduction in mortality from heart disease. An increase in HDL cholesterol concentration by 0.03 mmol/l reduces the risk of coronary disease by 2-3% in men and women. In addition, regardless of the content of total cholesterol in the blood (including those exceeding 5.2 mmol/l), an inverse relationship remains between the content of HDL cholesterol and the incidence of cardiac pathology.
Concentrations of HDL cholesterol less than 1.3 mmol/l and triglycerides in the blood more than 2.3 mmol/l are independent prognostic indicators of the likelihood of death from coronary artery disease. Therefore, HDL cholesterol levels should be considered a more accurate predictor of mortality from coronary artery disease than total cholesterol concentrations.
Based on the above, the following aspects should be taken into account in clinical practice:
- Reducing the concentration of LDL cholesterol and increasing the concentration of HDL cholesterol helps reduce the risk of developing atherosclerosis.
- The level of testosterone in men and estrogen in women is directly related to lipid metabolism disorders.
- The concentration of Lp(a) in the blood serum reflects the activity of the atherosclerotic process.
- Low physical activity (physical inactivity), excess nutrition, and smoking have an adverse effect on lipid metabolism.
- Correction of lipid disorders should be aimed not only at reducing blood cholesterol levels, but also at normalizing the lipid profile.
- Exercise and weight loss reduce plasma LDL-cholesterol and triglyceride concentrations and increase plasma HDL-cholesterol concentrations.
- A healthy lifestyle will prevent the development of atherosclerosis, the foundations of which can form at a relatively young age.
Optimal lipid profile (lipid profile):
- Total cholesterol
- HDL cholesterol > 1.3 mmol/l.
- LDL cholesterol
- Triglycerides
- CA
- AIP
A study of lipid metabolism (lipidogram) should be carried out in individuals in the age range from 20 to 80, every 5 years. It must be remembered that the likelihood of developing IHD and cardiovascular diseases increases if the subjects have other risk factors (smoking, diabetes mellitus, arterial hypertension, family history of IHD in first-degree relatives that developed in men under the age of 55 years, in women under 65 years of age). Therefore, to successfully reduce mortality from cardiovascular diseases, this population must be tested for the presence of all these factors.
Lipidogram (total cholesterol, triglycerides, HDL, LDL, atherogenic index)
[P 3.2.4]
| Price | Add 480 rub. |
| Ready time | 3 hours from the moment the biomaterial arrives at the laboratory |
| Material for research | Blood |
| Special conditions | Strictly on an empty stomach! |
| analysis included in the following profiles |
|
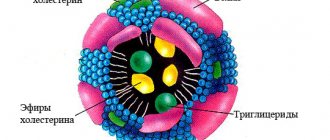
High-density lipoproteins (HDL) - belong to the group of “good” lipids and reduce the risk of developing atherosclerosis and cardiovascular disease. They remove cholesterol deposits from the walls of blood vessels, delivering them back to the liver for processing or excretion. Serves our body: to produce bile acid, which is necessary for the absorption of fats in the small intestine; it is the “raw material” of steroid hormones of the adrenal cortex (hydrocortisone and aldesterone), as well as female and male sex hormones (estrogens and androgens); for the formation of vitamin D, necessary for bone tissue, the nervous system, insulin production, maintaining muscle tone, mineral metabolism, immunity; for the normal activity of serotonin receptors in the brain. Serotonin is a substance responsible for a good mood. Low cholesterol levels cause depression and aggressive behavior.
Low-density lipoproteins (LDL) - belong to the group of “bad” lipids and increase the risk of developing atherosclerosis and cardiovascular disease. Low-density lipoproteins (LDL) - carry cholesterol to build the walls of blood vessels. But its excess tends to settle in them. Cholesterol plaques, growing, worsen the patency of blood vessels. And this reduces blood supply - nutrition of tissue organs. This disease is vascular atherosclerosis. The insidiousness of this disease lies in the fact that its symptoms - disturbances in the normal functioning of organs - appear only when the lumen of the vessel is closed by 75%. Hence such diseases of the circulatory system as: coronary heart disease, which can lead to myocardial infarction; thrombosis of arteries and veins; brain stroke; gangrene of the lower extremities.
Cholesterol is synthesized in the liver and is found in almost all cells of the body. Cholesterol enters the body from two sources: 70% of it is produced by the liver, and 30% comes from food.
Back to section
Blood test to assess lipid metabolism disorders, biochemical (with atherogenicity coefficient)
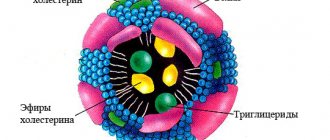
A lipidogram, or lipid profile, is a comprehensive study that determines the level of lipids (fats) in various blood fractions. Allows you to detect lipid (fat) metabolism disorders and assess the risk of developing cardiovascular diseases. Lipid metabolism disorders play an important role in the development of vascular atherosclerosis and diseases of the cardiovascular system. It has been scientifically proven that high levels of cholesterol in the blood (hypercholesterolemia) and local inflammatory changes in the vascular wall increase the risk of thickening and hardening of the arterial wall with subsequent disorders of local circulation. Atherosclerotic vascular damage, according to statistics, increases the likelihood of myocardial infarction, stroke, and kidney pathology. A lipidogram allows you to assess the atherogenicity (propensity to develop atherosclerosis) of blood plasma even with normal levels of total cholesterol. A lipid profile test measures triglycerides, total cholesterol (cholesterol), high-density lipids, low-density lipids, and very low-density lipids. The atherogenicity coefficient is calculated.Cholesterol is an important organic substance. It is synthesized mainly by the liver (endogenous cholesterol), and also partially enters the body with food (exogenous cholesterol). Cholesterol forms the cell membranes of all organs and tissues of the body, is a precursor of steroid hormones necessary for full development, growth and puberty, and takes part in the synthesis of bile acids, which ensure the absorption of nutrients from the intestines. Cholesterol circulates in the blood in combination with lipoproteins.
High-density lipoproteins (HDL) remove excess free cholesterol accumulated in peripheral cells. They transport cholesterol to the liver, where it is catabolized to form fatty acids, or transfer it to very low-density lipoproteins (VLDL), which converts them into low-density lipoproteins (LDL). HDL are antiatherogenic factors that prevent the formation of atherosclerotic plaque in the vessel. Reduced HDL indicates the possibility of developing the disease.
60-70% of total blood cholesterol is represented by LDL, which can linger in the vascular wall and contribute to the accumulation of cholesterol in tissues. It is the levels of LDL and, to a lesser extent, total cholesterol in the blood plasma that determine the risk of developing atherosclerosis and cardiovascular diseases. Even if the cholesterol level is maintained, an increase in LDL indicates the atherogenic properties of blood lipids.
Elevated levels of triglycerides in the blood are also associated with the risk of developing atherosclerosis, coronary heart disease and cerebrovascular disease. Elevated triglyceride levels are often combined with diabetes mellitus, obesity, arterial hypertension and changes in other lipid profile parameters.
The atherogenicity coefficient is calculated based on lipid metabolism indicators: CA = (total cholesterol - HDL) / HDL or CA = (LDL + VLDL) / HDL. An atherogenic coefficient exceeding normal limits indicates an increased risk of cardiovascular diseases.
When deciphering the lipid profile, it is necessary to take into account other risk factors for the development of cardiovascular diseases. These include age, gender, hereditary predisposition to dyslipidemia and heart and vascular diseases, carbohydrate metabolism disorders (diabetes mellitus), increased blood pressure, obesity, smoking, alcohol consumption, and kidney pathology.
What is the research used for?
— To assess the risk of developing cardiovascular diseases.
— For dynamic monitoring of patients with coronary heart disease, hypertension, atherosclerosis of the heart and blood vessels, kidney pathology, diabetes mellitus.
— To evaluate patients with a family history of hypercholesterolemia and a high risk of myocardial infarction or stroke.
— To control lipid-lowering therapy and diet. When is the study scheduled?
— During a preventive examination of healthy people (after 20 years of age, it is recommended to determine the level of lipids in the blood once every 5 years).
- With an increase in total cholesterol.
- With a history of high cholesterol levels.
- With a burdened hereditary history (diabetes mellitus, stroke, myocardial infarction, arterial hypertension).
- In the presence of factors that increase the risk of cardiovascular complications (age over 45 years for men and 55 years for women, smoking, overweight, carbohydrate metabolism disorders, high blood pressure).
— When monitoring the effectiveness of a lipid-lowering diet and/or drug treatment with statins.
Decoding the results
Reference values are 0.26-1.04 mmol/l. An increase in indicators indicates a violation of lipid metabolism. The reason for this may be either a hereditary predisposition or poor nutrition (excess fat in the daily diet). If violations are detected, therapy or preventive measures are prescribed. Laboratory values are monitored at regular intervals until they return to normal. For patients with kidney pathologies and diabetes, increased levels pose a particularly high danger. A high level of VLDL in the presence of such pathologies leads to the rapid development of atherosclerosis.
It is necessary to take into account that blood is donated for research when a person is practically healthy. After an acute illness or surgery, at least 1.5 months must pass.
Relevance of the analysis
Specialists in our department prescribe a lipid profile if the following diseases are suspected:
- Atherosclerosis;
- Coronary vascular disease;
- Myocardial infarction;
- IHD (coronary heart disease);
- Vascular pathologies of the brain.
The study is prescribed for both diagnostic and preventive purposes, especially for patients at risk.
Fats are present in the blood of any person in certain concentrations. They are deposited in tissues and participate in metabolic processes that ensure the normal functioning of the body. Disorders of fat metabolism, such as increased cholesterol levels, can lead to the development of pathological processes. The main ones are atherosclerosis, ischemia, heart attacks and strokes.
The test may be part of a routine medical examination. Our specialists prescribe it to patients who are at risk according to certain criteria. If imbalances in fat levels are detected, your doctor may prescribe preventive therapy. It includes lifestyle correction - normalization and stabilization of body weight, diet, and physical exercise. In some situations, medications are prescribed.
VLDL cholesterol
Very low-density lipoprotein cholesterol (VLDL cholesterol) is a type of lipoprotein that carries cholesterol in the blood. Lipoproteins transport lipids throughout the body, making fats available to body cells through endocytosis. The generally accepted interpretation of cholesterol levels is that higher levels of VLDL particles pose an increased risk of cardiovascular disease.
Monitoring and maintaining healthy lipid levels is important for good health. Eating too many foods high in saturated fat and trans-unsaturated fat (trans fat) can lead to high levels of VLDL cholesterol in the blood
. Extra cholesterol can be deposited in the walls of blood vessels. As a result, cholesterol plaques form, which leads to changes in the arteries (atherosclerosis), increasing the risk of health problems, including coronary heart disease and cerebrovascular accident. Coronary artery disease occurs when plaque builds up in the arteries of the heart. This causes the arteries to become stiffer and narrower, which in turn slows or blocks blood flow to the heart. Since blood carries oxygen to the heart, this means that a person's heart is not able to get enough oxygen. This condition can cause angina (chest pain) or, if blood flow is completely blocked, a heart attack. If the same plaque clogs a vessel in the brain, the person may have a stroke. This distinguishes this type of cholesterol from high-density lipoprotein (HDL) cholesterol, which transports cholesterol from the artery to the liver, rather than the other way around.
Excess weight tends to raise VLDL levels, lower HDL levels, and raise total cholesterol levels. There are also a number of hereditary diseases when VLDL cholesterol in the blood remains constantly elevated. Another condition that affects cholesterol levels is cholestasis (bile stagnation). A blood test for very low-density lipoprotein cholesterol (VLDL) can help determine a person's risk of developing cardiovascular disease and help decide whether to use medications to lower their lipid levels. If a person agrees to therapy with lipid-lowering drugs, then it is necessary to be tested for VLDL and liver tests (ALAT, ASAT).
General information
The amount of VLDL serves as an indicator of the level of harmful cholesterol and lipid metabolism. Excess cholesterol is deposited on the walls of blood vessels. First, plaque forms on them, and over time plaques form. Excess cholesterol can also have a negative effect on triglyceride transport. The test results are assessed taking into account the clinical picture and data from other studies.
Cholesterol refers to substances without which the body cannot function normally. At the same time, its excess is dangerous to health. This substance is necessary for the construction of cell membranes, the synthesis of certain hormones, and the formation of fatty acids. Lack of cholesterol leads to disruption of these processes. Cholesterol, which is necessary for the functioning of the body, is produced by the liver. This substance is also absorbed from food. An increase in its level is observed if a person constantly eats too much animal fat, as well as in the presence of a hereditary predisposition.