© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
The right aortic arch in the fetus is a congenital heart defect, which can occur alone or be combined with other, sometimes severe, defects. In any case, during the formation of the right arch, disturbances in the normal development of the fetal heart occur.
The aorta is the largest vessel in the human body, the function of which is to move blood from the heart to other arterial trunks, up to the arteries and capillaries of the whole body.
Phylogenetically, the development of the aorta undergoes complex changes during evolution. Thus, the formation of the aorta as an integral vessel occurs only in vertebrates, in particular in fish (two-chamber heart), amphibians (two-chamber heart with an incomplete septum), reptiles (three-chamber heart), birds and mammals (four-chamber heart). However, all vertebrates have an aorta, into which arterial blood mixed with venous, or entirely arterial, flows.
During the process of individual development of the embryo (ontogenesis), the formation of the aorta undergoes changes as complex as the heart itself. Starting from the first two weeks of embryo development, there is an increased convergence of the arterial trunk and the venous sinus, located in the cervical part of the embryo, which subsequently migrated more medially, towards the future thoracic cavity. The arterial trunk gives rise not only to two ventricles subsequently, but also to six branchial (arterial) arches (six on each side), which, as they develop, within 3-4 weeks, are formed as follows:
- the first and second aortic arches are reduced,
- the third arch gives rise to the internal carotid arteries that supply the brain,
- the fourth arch gives rise to the aortic arch and the so-called “right” part,
- the fifth arc is reduced,
- the sixth arch gives rise to the pulmonary trunk and the arterial (Botallov) duct.
The heart becomes completely four-chambered, with a clear division of the cardiac vessels into the aorta and pulmonary trunk, by the sixth week of development. A 6-week embryo has a fully formed, beating heart with large vessels.
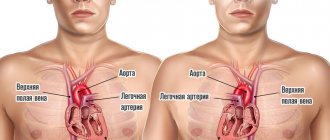
After the formation of the aorta and other internal organs, the topography of the vessel looks like this. Normally, the left aortic arch begins from the aortic bulb in its ascending part, which, in turn, originates from the left ventricle. That is, the ascending part of the aorta passes into the arch approximately at the level of the second rib on the left, and the arch bends around the left main bronchus, heading posteriorly and to the left. The uppermost part of the aortic arch projects onto the jugular notch just above the upper part of the sternum. The aortic arch goes down to the fourth rib, located to the left of the spine, and then passes into the descending part of the aorta.
In the case when the aortic arch “turns” not to the left, but to the right, due to a failure in the formation of human vessels from the branchial arches of the embryo, they speak of a right-sided aortic arch. In this case, the aortic arch extends through the right main bronchus, and not through the left, as it should normally be.
Why does vice occur?
Any malformation is formed in the fetus if a woman is influenced by negative environmental factors during pregnancy - smoking, alcoholism, drug addiction, ecology and unfavorable background radiation. However, genetic (hereditary) factors play an important role in the development of the child’s heart, as well as existing chronic diseases in the mother or past infectious diseases, especially in the early stages of pregnancy (influenza, herpes infection, chickenpox, rubella, measles, toxoplasmosis and many others) .
But, in any case, when any of these factors influence a woman in the early stages of pregnancy, the normal processes of ontogenesis (individual development) of the heart and aorta, formed during evolution, are disrupted.
So, in particular, the period of pregnancy of approximately 2-6 weeks is especially vulnerable to the fetal heart, since it is at this time that the formation of the aorta occurs.
Development mechanism
The basis of the pathological process is destruction of the aortic wall or a constant increased impact on the structure.
In the first case, we are talking about infectious-inflammatory, less often autoimmune processes. As a result of the constant violation of the anatomical integrity of the endothelium and other tissues, severe scarring occurs.
Epithelization leads to a gradual overgrowing of the lumen with dense connective tissue and its narrowing. The blood flow weakens, and the pressure in the local area becomes higher due to the need to overcome a mechanical obstacle.
The second factor is approximately identical, in terms of creating excess load on the walls of blood vessels. The main etiological point is an increase in blood pressure and the constant preservation of tonometer readings at consistently high numbers.
Both options pose a colossal danger to human life and health.
Organic disorders are difficult to treat, and not every doctor is ready to take on such unpredictable cases. Therefore, the logical solution would be to carry out treatment in the early stages, when there are no anatomical abnormalities yet.
Classification of the right-sided aortic arch
variant of the right aortic arch with the formation of a vascular ring
Depending on the anatomy of the duct anomaly, there are:
- The right aortic arch without the formation of a vascular ring, when the arterial ligament (overgrown arterial, or Botallov, duct, as it should be normally after childbirth) is located behind the esophagus and trachea,
- The right arch of the aorta with the formation of a vascular ring, code arterial ligament, or patent ductus arteriosus, is located on the left of the trachea and esophagus, as if surrounding them.
- As well as a separate similar form, the double arch of the aorta is distinguished - in this case, the vascular ring is formed not by the connective ligament, but by the inflow of the vessel.
Figure: a variety of options for the atypical structure of the aortic arch
Depending on whether any other structures of the heart were damaged during its formation, the following types of defect are distinguished:
- An isolated type of defect, without other developmental anomalies (in this case, if the right-sided aorta is not combined with the DiGeorge syndrome characteristic of it in some cases, the prognosis is as favorable as possible);
- In combination with dextraposition (mirror, right position of the heart and great vessels, including the aorta), (which is also usually not dangerous),
- In combination with a more serious heart defect - in particular tetralogy of Fallot (dextraposition of the aorta, ventricular septal defect, pulmonary stenosis, right ventricular hypertrophy).
Tetralogy of Fallot combined with the right arch is an unfavorable development option
Forecast
{banner_banstat9}
In itself, aortic thickening is not a diagnosis, but just an instrumental finding. You can say anything concrete after assessing the root cause.
The following factors play a major role:
- Dynamics of deviation. Progression is associated with more severe general condition and outcome.
- The age of the person. Elderly people have a relatively unfavorable prognosis.
- Family history. If there was at least one representative in the family with the condition in question, it is necessary to carefully check every six months. In such individuals, the anomaly progresses rapidly. Therefore, delay reduces the chances of successful treatment.
- The presence of concomitant somatic pathologies. Among the especially dangerous ones are hypertension, diabetes mellitus, metabolic syndromes, and atherosclerosis.
- Possibility and necessity of radical treatment. If surgery is required, the prognosis is initially worse. Further, everything depends on the success of the therapy. The absence of such a need gives a better outcome, although it does not guarantee it.
In general, even an aneurysm, as one of the most severe complications, is associated with a survival rate of 85-90%.
Attention:
Heart failure and circulatory disorders in the brain reduce the patient's chances by 30-40%.
How to recognize a vice?
Diagnosis of the defect is not difficult even during pregnancy. This is especially true in cases where the right aortic arch is combined with other, more severe anomalies of heart development. However, to confirm the diagnosis, a pregnant woman is repeatedly examined, including with expert-class ultrasound machines, and a council of geneticists, cardiologists and cardiac surgeons is assembled to make a decision on the prognosis and the possibility of delivery in a specialized perinatal center. This is due to the fact that with some types of defects combined with the right aortic arch, the newborn baby may require heart surgery immediately after delivery.
Regarding the clinical manifestations of the right aortic arch, it should be mentioned that an isolated defect may not manifest itself at all, only sometimes accompanied by frequent obsessive hiccups in a child. In the case of a combination with tetralogy of Fallot, which accompanies the defect in some cases, the clinical manifestations are pronounced and appear in the first days after birth, such as increasing pulmonary heart failure with severe cyanosis (blue discoloration of the skin) in the baby. That is why tetralogy of Fallot is classified as a “blue” heart defect.
What screening shows a defect in pregnant women?
The diagnosis of a right-sided aortic arch can be made already at the first screening, that is, at 12-13 weeks of pregnancy. More accurate information about the condition of the fetal heart can be obtained at the second and third screening ultrasound examinations (20 and 30 weeks of pregnancy).
An analysis of fetal DNA can further clarify the absence of a connection between the formation of a right-sided aorta and severe genetic mutations. In this case, chorionic villus material or amniotic fluid is usually collected through a puncture. First of all, DiGeorge syndrome is excluded.
Diagnostics
It takes place on an outpatient basis, under the supervision of a cardiologist or vascular surgeon. The following activities are shown:
- Oral interview with a person. To get a rough picture.
- Anamnesis collection. Family history, addictions, past pathologies.
- Measurement of blood pressure and heart rate.
- Echocardiography. One of the first methods. Gives an idea of the state of the muscular organ itself and the ascending aorta, arch.
- Aortography. Targeted assessment of the largest vessel. It is used both to verify the diagnosis and to determine the effectiveness of the treatment.
- MRI. Used to clarify the localization of the pathological focus. Typically, tomography is prescribed before surgery as an informative way to visualize tissue.
- ECG. To identify functional disorders that inevitably arise at advanced stages of changes in the aorta.
- Ultrasound of the abdominal cavity.
- Plain chest x-ray.
Methods provide nuggets of valuable information. To get a complete picture, you need to carry out all these activities. They are not dangerous and painless. Therefore, it is not recommended to hesitate.
Treatment
In the event that the right aortic arch is isolated and is not accompanied by any clinical manifestations after the birth of the child, the defect does not require surgical treatment. All you need is a monthly examination by a pediatric cardiologist with regular (every six months - once a year) ultrasound of the heart.
When combined with other heart defects, the type of surgical intervention is selected based on the type of defect. Thus, with tetralogy of Fallot, surgery is indicated in the first year of a child’s life, carried out in stages. At the first stage, palliative (auxiliary) shunts are applied between the aorta and the pulmonary trunk to improve blood flow into the pulmonary circulation. At the second stage, open heart surgery is performed using a cardiopulmonary bypass machine (ACB) to eliminate pulmonary stenosis.
In addition to surgery, cardiotropic drugs that can slow the progression of chronic heart failure (ACE inhibitors, diuretics, etc.) are prescribed for auxiliary purposes.
Symptoms
There are no such manifestations. If the walls of the aorta are compacted, there is no clinical picture. Signs and disturbances in well-being arise later, after complications of the pathological process.
Organic changes, such as an aortic aneurysm, give the following moments:
- Pain syndrome. Localization and nature depend on the location of the violation. If the abdominal region is affected, there is discomfort in the abdomen, and in the chest there is a pressing, burning sensation. If the aortic arch is compacted, there is pain in the neck, turning into discomfort at the location of the heart.
- Dyspnea. Disruption of a natural physiological process.
Further manifestations depend on which area has undergone changes.
Abdominal:
- Nausea, vomiting, heartburn, belching, other dyspeptic symptoms. Such patients are falsely sent to gastroenterology.
- Increased gas formation in the intestines.
- Pulsating sensations in the abdomen.
Arc, descending section:
- Inability to swallow normally.
- Violations of voice, timbre and general ability to speak.
- Excessive saliva production.
- Weakness.
- Numbness of the upper and lower extremities. In exceptional cases, paresis and paralysis occur. This is the result of compression of the nerve roots.
Such conditions require urgent treatment; irreversible changes in the musculoskeletal system are possible.
Compaction of the aortic root and ascending section:
- Chest pain.
- Dyspnea.
- Abnormal heart rate, other arrhythmias.
- Cephalgia, vertigo.
- Loss of consciousness, fainting.
Classic signs of damage to cardiac structures.
Attention:
You cannot focus on symptoms when identifying the causes of poor health. These are unreliable clinical signs.
Complications
{banner_banstat10}
Possible consequences:
- Thrombosis. The formation of a clot in one of the arteries, sometimes in the aorta itself. Causes local ischemia. When torn off and moved along the riverbed, it often blocks the pulmonary vessel and coronary structures, which immediately leads to death.
- Aneurysm. Wall protrusion. It is observed against the background of stable degeneration and dystrophy of aortic tissue.
- Rupture, delamination. Leads to death within a matter of seconds. There were cases to the contrary, but they were casuistic. There are hardly more than 0.5%.
Thickening of the aortic walls is not an independent disease. It is not considered a diagnosis and is not represented in the ICD-10 classifier. This is a consequence, an accidental find.
After eliminating the root cause, there is every chance to stop the progression and achieve results without affecting the quality and length of life.