Central aortic pressure and vascular stiffness: relevance in modern cardiology
The increase in cardiovascular diseases, observed in all developed countries of the world, requires close attention to the prevention and effective treatment of heart and vascular diseases.
Research data suggests that hypertension affects approximately 65 million Americans aged 18–39 years and 1 billion people worldwide. Arterial hypertension (AH) is a risk factor for the development and progression of atherosclerosis, coronary heart disease, chronic heart failure and acute cerebrovascular accidents. Changes in elastic vessels (aorta, pulmonary artery and large arteries branching from them) are an important part of the pathogenesis of hypertension. Normally, the elastic properties of these vessels, especially the aorta, help smooth out the periodic waves of blood produced by the left ventricle during systole and convert them into continuous peripheral blood flow. The elastic properties of the aorta modulate left ventricular function by reducing left ventricular afterload and end-systolic and diastolic volumes. This leads to a decrease in the tension of the walls of the left ventricle, as a result of which the trophism of the subendocardial layers of the myocardium, which are most sensitive to hypoxia, improves and coronary blood flow improves. One of the significant characteristics of elastic-type vessels is rigidity, which determines the ability of the arterial wall to resist deformation. The stiffness of the vascular wall depends on age, the severity of atherosclerotic changes, the speed and degree of age-related involution of the most important structural proteins elastin and fibulin, an age-related increase in collagen stiffness, genetically determined characteristics of elastin fibers and the level of blood pressure (BP). A number of studies have emphasized the role of inflammation in the pathogenesis of large artery stiffness. The classic marker of arterial stiffness/elasticity of large vessels is pulse wave velocity (PWV). The value of this indicator largely depends on the ratio of the thickness of the vessel wall to the radius of the vessel lumen and the elasticity of the vessel wall. The more distensible the vessel, the slower the pulse wave propagates and the faster it weakens, and vice versa - the more rigid and thick the vessel and the smaller its radius, the higher the PWV. Normally, PWV in the aorta is 4–6 m/s; in less elastic arteries of the muscular type, in particular the radial artery, it is 8–12 m/s. The gold standard for assessing aortic stiffness is the PWV between the carotid and femoral arteries.
Central (aortic) and peripheral blood pressure
In a normal arterial system, after contraction of the ventricle in systole, the pulse wave is directed from the site of origin (aorta) to large medium and then small vessels at a certain speed. Along the way, the pulse wave encounters various obstacles (for example, bifurcations, resistive vessels, stenoses), leading to the appearance of reflected pulse waves directed to the aorta. With sufficient elasticity of large vessels, primarily the aorta, the reflected wave is absorbed. The sum of direct and reflected pulse waves differs in different vessels; as a result, blood pressure, primarily systolic blood pressure (SBP), differs in different main vessels and does not coincide with that measured on the shoulder. The degree of increase in SBP in the peripheral arteries relative to SBP in the aorta varies greatly between subjects and is determined by the elastic modulus of the arteries studied and the distance from the measurement site. Because of this, the cuff pressure in the brachial artery does not always correspond to the pressure in the descending aorta. A certain contribution to the increase in blood pressure in the brachial artery relative to blood pressure in the aorta is made by an increase in the rigidity of its wall, which means the need to create greater compression in the cuff. Unlike peripheral blood pressure, the level of central blood pressure is modulated by the elastic characteristics of large arteries, as well as the structural and functional state of medium-sized arteries and the microvasculature and, thus, is an indicator that indirectly reflects the state of the entire cardiovascular system. The greatest prognostic value is blood pressure in the ascending and central parts of the aorta, or central blood pressure. In the case of increased stiffness (decreased elasticity) of the aorta, the reflected wave is not absorbed sufficiently and, as a rule, due to a higher PWV, returns during systole, which leads to an increase in central SBP. The consequence of increased rigidity and increased central blood pressure is a change in afterload on the left ventricle and impaired coronary perfusion, which leads to left ventricular hypertrophy and increased myocardial oxygen demand.
In recent years, special techniques have appeared (for example, applanation tonometry of the radial or carotid arteries) that make it possible to record such determinants of pulse pressure as pulse (oscillations of the arterial wall from the heart to resistive vessels) and reflected (oscillations of the arterial wall from resistive vessels to the heart) waves, and, using computer processing when recording radial artery oscillations, calculate the values of central pressure in the aorta (Fig. 1). Within 10 seconds, the pressure curve in the radial artery of the upper limb is recorded using an applanation tonometer. The data is processed using software: the average shape of the curve is calculated, which is transformed using the accepted mathematical method into a graph of central pressure in the aorta (CPA). Computer processing of the obtained central pressure curves allows one to determine the parameters of the central pressure: the time to the first (T1) and second (T2) systolic peaks of the wave. The pressure at the first peak/kink (P1) is taken as the ejection pressure, a further increase to the second peak (ΔP) means the reflected pressure, their sum (maximum pressure during systole) is the systolic central pressure (CPAs). In addition to the value of central blood pressure, there is an indicator of pressure increase, augmentation index (amplification, AIx) expressed as a percentage, which is defined as the pressure difference between the first, early peak (caused by cardiac systole) and the second, late (appearing as a result of reflection of the first pulse wave) systolic peak, divided by the central pulse pressure. Thus, central aortic pressure is a calculated hemodynamic parameter that depends not only on cardiac output and peripheral vascular resistance, but also on the structural and functional characteristics of the main arteries (their elastic properties). Differences between central and peripheral SBP levels are most pronounced in young people and decrease in older people. Central blood pressure, especially central pulse pressure, and the augmentation index have been shown to correlate with the degree of large artery remodeling and PWV as a classic indicator of vascular wall stiffness.
Arterial stiffness as a cardiovascular risk factor
Changes in the mechanical properties of large arteries have a clear pathophysiological relationship with clinical outcomes. Research suggests that PWV, a measure of arterial stiffness, may be a better predictor of subsequent cardiovascular events than known risk factors such as age, blood pressure, hypercholesterolemia and diabetes. Studies assessing PWV have established that increased arterial stiffness is a predictor of cardiovascular risk in apparently healthy individuals, patients with diabetes mellitus, end-stage renal disease, and the elderly. It has been demonstrated that arterial stiffness is a predictor of mortality in patients with hypertension. Thus, in a population-based study of the Copenhagen County population, it was demonstrated that an increase in PWV (>12 m/s) is associated with a 50% increase in the risk of cardiovascular events. In addition, the prognostic value of PWV was found in a Japanese study with an average follow-up of 8.2 years. Indirect indices of aortic stiffness and reflected waveforms, such as central aortic pressure and augmentation index, have been found to be independent predictors of cardiovascular events and mortality. Thus, in a study that included 1272 normotensive and untreated patients with hypertension, it was demonstrated that central SBP was an independent predictor of cardiovascular mortality after adjustment for various cardiovascular risk factors, including left ventricular myocardial mass and determination of intima-media thickness. with ultrasound examination of the carotid arteries. Moreover, patients with high aortic pressure have a worse cardiovascular prognosis than patients with better control of central aortic pressure.
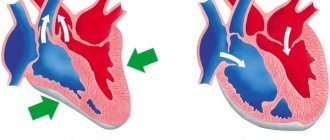
Increased aortic stiffness is also an independent predictor of diastolic dysfunction in patients with hypertension (Fig. 2) and may also limit exercise capacity in dilated cardiomyopathy. In patients with heart failure with preserved left ventricular ejection fraction, systolic dysfunction and arterial stiffness appear with age and/or progression of hypertension. Increased arterial stiffness is associated with endothelial dysfunction and decreased nitric oxide (NO) bioavailability. Endothelial dysfunction in patients at high cardiovascular risk may explain why these conditions are associated with increased arterial stiffness in the early stages before the onset of atheroma. Therefore, drugs such as nebivolol that increase NO production may reduce large artery stiffness, which in turn may lead to a reduction in cardiovascular risk. Thus, the importance of arterial stiffness, assessed by PWV, for the risk of cardiovascular outcomes has been demonstrated in a number of prospective studies both in patients with hypertension and in the general population. Since 2007, assessment of PWV on the carotid-femoral segment has been recommended as an additional research method for identifying target organ damage in hypertension.
Authors
A.N. Belovol, Doctor of Medical Sciences, Professor, Corresponding Member of the National Academy of Medical Sciences of Ukraine;
I.I. Kknyazkova, Doctor of Medical Sciences, Associate Professor
Kharkov National Medical University
Article provided by the WEB site “Country of Doctors”
Blood pressure
Why does a person feel uncomfortable with hyper- or hypotension: headache, pounding in the temples, weakness, etc.?
Blood pressure is the pressure inside blood vessels (inside arteries - arterial pressure, inside capillaries - capillary pressure and inside veins - venous pressure). It allows blood to move through the circulatory system, resulting in metabolic processes in the tissues of the body.
The value of blood pressure (BP) is determined mainly by the strength of heart contractions, the amount of blood that the heart ejects with each contraction, and the resistance provided to blood flow by the walls of blood vessels (especially peripheral ones). The amount of circulating blood, its viscosity, pressure fluctuations in the abdominal and thoracic cavities associated with respiratory movements, and other factors also influence the value of blood pressure.
Blood pressure reaches its maximum level during contraction (systole) of the left ventricle of the heart. In this case, 60-70 ml of blood is pushed out of the heart. This amount of blood cannot pass immediately through small blood vessels (especially capillaries), so the elastic aorta is stretched and the pressure in it increases (systolic pressure). Normally, it reaches 100-140 mm Hg in large arteries. Art.
During the pause between contractions of the ventricles of the heart (diastole), the walls of the blood vessels (aorta and large arteries), being stretched, begin to contract and push blood into the capillaries. Blood pressure gradually drops and by the end of diastole reaches a minimum value (70-80 mm Hg in large arteries). We perceive the difference in the magnitude of systolic and diastolic pressure, or rather fluctuations in their values, in the form of a pulse wave, which is called the pulse.
Blood pressure in blood vessels decreases as it moves away from the heart. So, in the aorta the pressure is 140/90 mm Hg. (the first number indicates systolic, or upper, pressure, and the second - diastolic, or lower). In large arteries the pressure averages 120/75 mm Hg. In arterioles, there is practically no difference in systolic and diastolic pressure, and blood pressure is about 40 mmHg. In the capillaries, blood pressure drops to 10-15 mm Hg. As blood moves into the venous bed, blood pressure decreases even more, and in the largest veins (superior and inferior vena cava) blood pressure may be negative.
Normally, the value of blood pressure depends on individual characteristics, lifestyle, and occupation. Its value changes with age, increases with physical activity, emotional stress, etc. However, in people who systematically engage in heavy physical labor, as well as in athletes, the value of systolic pressure can decrease and amount to 100-90, and diastolic pressure - 60 and even 50 mm Hg.
Normal blood pressure for a healthy adult is 100-129 (upper) and 70-80 (lower). If the pressure is above these values, but below 140 (upper) and 90 (lower), it is called “normal elevated”. In children, the value of systolic pressure can be approximately calculated using the formula 80 + 2a, where a is the number of years of the child’s life.
Despite significant fluctuations in blood pressure (for example, depending on the load, emotional state, etc.), the body has complex mechanisms for regulating its level, striving to return the pressure to normal after the effects of these factors cease. In some cases, the mechanisms of this regulation are disrupted, which leads to changes in blood pressure levels. A persistent change in blood pressure in the upward direction is called arterial hypertension (hypertension), and in the downward direction - arterial hypotension. Although changes in blood pressure often play a protective and adaptive role, if it deviates from the norm, it is better to consult a doctor.
Hypertension (essential hypertension) accounts for up to 90% of all cases of chronic high blood pressure. In economically developed countries, 18-20% of adults suffer from hypertension, that is, they have repeated rises in blood pressure up to 140/90 mm Hg. and higher. They focus on the values of the so-called “random” pressure, measured after a five-minute rest, in a sitting position, three times in a row (the lowest values are taken into account). During the first examination of patients, the doctor always measures the pressure on both arms, and, if necessary, on the legs.
Go to tonometers - devices designed to measure blood pressure.
Symptoms and course
Hypertension usually occurs between the ages of 30 and 60 and is chronic with periods of deterioration and improvement.
- Stage I (mild) is characterized by increases in blood pressure in the range of 160-180/95-105 mm Hg. Art. This level is unstable and gradually returns to normal during rest. I am concerned about pain and noise in the head, poor sleep, and decreased mental performance. Occasionally - dizziness, nosebleeds.
- Stage II (intermediate) - higher and more stable blood pressure levels (180200/105-115 mmHg at rest). Headaches in the heart area and dizziness also increase. Hypertensive crises (sudden and significant increases in blood pressure) are possible. Signs of damage to the heart, central nervous system (transient cerebrovascular accidents, strokes), changes in the fundus, and decreased blood flow in the kidneys appear.
- Stage III (severe) - pressure reaches 200-230/115-130 mm Hg. Art., there is no independent normalization of it. This load on the vessels causes irreversible changes in the activity of the heart (angina pectoris, myocardial infarction, heart failure, arrhythmias), brain (strokes, encephalopathy), fundus of the eye (damage to retinal vessels - retinopathy), kidneys (decreased blood flow, glomerular filtration, chronic renal failure ).
Recognition is carried out on the basis of systematic determination of blood pressure, identification of characteristic changes in the fundus and electrocardiogram.
Hypertension must be distinguished from secondary arterial hypertension (symptomatic) that occurs with diseases of the kidneys, renal vessels, endocrine organs (Itsepko-Cushing's disease, acromegaly, primary aldosteronism, thyrotoxicosis), circulatory disorders (atherosclerosis of the aorta, aortic valve insufficiency, complete atrioventricular blockade, coarctation of the aorta).
Treatment
Non-medicinal: weight loss, limiting salt intake, spa treatment, physiotherapeutic procedures.
The doctor prescribes drug treatment, which may include various types of drugs that lower blood pressure (enalapril, metoprolol, etc.), diuretics (hypothiazide, brinaldix, triampur, etc.), etc. In this case, the selection of therapy should be carried out purely individually.
So, for a patient with hypertension:
It is forbidden:
- Smoking.
- Eat salty, spicy, fatty foods.
- Gain extra pounds.
- Abuse alcohol, especially combining libations with taking medications.
- Work at night, sleep less than 7 hours.
- Be nervous about trifles.
- Lead a sedentary lifestyle
- Skip or stop taking medications prescribed by your doctor
- Try on yourself medicines that “helped” your neighbor (brother, matchmaker, etc.)
Need to:
- Quit smoking.
- Limit salt intake. Herbal seasonings will help make dishes less bland.
- Eat more greens, fruits, foods rich in potassium, and do not get carried away with protein foods.
- Eat regularly, especially if you are taking medications at the same time as eating.
- Try to lose extra pounds.
- Be able to switch gears and not get hung up on troubles.
- Move more. Walking, swimming, and therapeutic exercises are especially useful.
- Regularly measure blood pressure using a tonometer.
- Follow all doctor's recommendations. You should listen especially carefully when it comes to taking medications.
Hypotonic disease (primary chronic hypotension, essential hypotension) is a disease associated with dysfunction of the nervous system and neurohormonal regulation of vascular tone, accompanied by a decrease in blood pressure. The initial background of this condition is asthenia associated with traumatic situations, chronic infections and intoxications (occupational hazards, alcohol abuse), and neuroses.
Symptoms and course
Patients are lethargic, apathetic, they are overcome by extreme weakness and fatigue in the morning, they do not feel cheerful even after a long sleep; Memory deteriorates, a person becomes absent-minded, his attention is unstable, performance decreases, he is constantly bothered by the feeling of lack of air, potency and libido in men and the menstrual cycle in women are disrupted.
Emotional instability, irritability, increased sensitivity to bright light and loud speech predominate. Habitual headaches are often associated with fluctuations in atmospheric pressure, large meals, and prolonged stay in an upright position. It occurs like a migraine with nausea and vomiting, and decreases after a walk in the fresh air or exercise, rubbing the temporal areas with vinegar, applying ice or a cold towel to the head. There are dizziness, staggering when walking, fainting. Blood pressure is usually slightly or moderately reduced to 90/60-50 mmHg.
Recognition is carried out on the basis of clinical signs and the exclusion of diseases accompanied by secondary arterial hypotension (Addison's disease, pituitary insufficiency, Simmonds' disease, acute and chronic infections, tuberculosis, peptic ulcer, etc.).
Treatment
Correct work and rest schedule. The attending physician may prescribe sedatives and tranquilizers (mezatone, ephedrine), drugs that stimulate the central nervous system (tincture of ginseng, Chinese schisandra, zamanikhi, pantocrine, etc.). Physiotherapeutic (baths, massage), sanatorium-resort treatment, physical therapy are possible.
Aortic aneurysm - symptoms and treatment
Treatment of aortic aneurysms is aimed at preventing its rupture. It can be conservative or surgical.
Conservative treatment
The main purpose of conservative therapy is to reduce blood pressure and the force of heart contraction, as well as the correction of concomitant diseases, such as coronary heart disease, diabetes, kidney disease, etc. [1]
Surgery
Modern surgical techniques for treating aortic aneurysms are divided into endovascular and traditional surgical interventions.
The endovascular method is the remote implantation of special tubular prostheses (stent grafts) into the affected area of the aorta from the inside through a catheter installed in the femoral artery. This method of treatment is performed under local or regional anesthesia, it is low-traumatic, low-painful and reduces hospital stay, and also reduces mortality. Increasingly, in the practice of vascular surgery, minimally invasive endovascular technologies are used in the treatment of aneurysms of the thoracic and abdominal aorta, although it is still too early to discount open surgical interventions [4].
Major operations for thoracic aneurysms are among the most difficult in medicine. They are performed in specialized cardiac surgery centers with the heart turned off during artificial circulation. The technology of the operation consists of replacing the dilated section of the aorta with a special tubular prosthesis, which is sewn into place of the aneurysmal sac [5][10]. The surgeon makes an incision to provide access to the aneurysm, excises the affected part and replaces it with a prosthesis. But in some cases, for example after injury, the aorta can be sutured end to end without the use of a prosthesis.
Abdominal aortic aneurysms with a diameter of more than 5.5 cm in men and 5.2 cm in women have a high risk of rupture, and therefore require immediate consultation with a vascular surgeon to determine indications for surgical treatment. It is performed in the vascular departments with access through the anterior abdominal wall (laparotomy) and also aims to replace the affected segment of the aorta with a prosthesis. Some medical centers have mastered laparoscopic treatment of aneurysms, which does not require incisions [4][7].
During surgical treatment of such severe diseases (as with other therapeutic and diagnostic interventions), there is a possibility of complications. It is also worth noting that not all regional, regional and republican medical centers have specialists who work on open heart surgery.
Cardiovascular diseases (CVD) remain one of the leading causes of mortality in most economically developed countries according to epidemiological studies [1]. This is despite the fact that for many years the most important goal of treating patients with CVD is not the symptomatic effects of pharmacotherapy, but reducing the risk of fatal and non-fatal complications [1-3].
The nature of the course of arterial hypertension (AH), which underlies the cardiovascular continuum, largely determines the individual prognosis. This necessitates a continuous search for indicators of prognosis of long-term results of antihypertensive therapy (AHT) that are more reliable than measuring blood pressure (BP) at a doctor’s appointment. Measurement of central blood pressure (CAP) in patients with hypertension is of increasing interest due to the fact that it can be significant for stratifying the risk of developing cardiovascular complications (CVD) and responds differently to antihypertensive drugs (AHD) than blood pressure. measured on the brachial artery (BA) [2, 4].
In accordance with the concept of the cardiovascular continuum, in addition to high blood pressure, diabetes mellitus (DM), hyperlipidemia also affect the prognosis and management of patients [5, 6]. The multiorgan changes are based on a subclinically developing increase in stiffness and decrease in elasticity of the main arteries, which certainly determines the further course of CVD [7, 8]. Thus, the study of the structural and functional properties of the vascular wall is a promising direction in modern cardiology.
Types of arterial wall rigidity and methods of their registration.
Previously, the structural and functional state of the arteries, in particular the aorta, was studied using invasive methods. Thus, the elasticity of the arterial wall was assessed by changes in the pressure/diameter ratio using a sensor mounted in the catheter during vessel catheterization. The advantages of the described technique are reliability and diagnostic accuracy, the disadvantages are the complexity of implementation and the high cost of equipment. For obvious reasons, in recent years, increasing preference has been given to non-invasive methods, such as magnetic resonance imaging, Doppler ultrasound, and volumetric sphygmography [9, 10].
Modern devices for indirect (non-invasive) assessment of the structural and functional properties of the vascular wall make it possible to study 3 types of stiffness: systemic, regional and local. Systemic stiffness is studied only on circulatory models, regional and local - directly on various parts of the arterial system [11].
The technique for non-invasive recording of systemic compliance of the proximal and distal segments of the arterial bed is based on an electrical circuit built by analogy with the modified Windkessel model. In this case, stiffness is determined by recording the pulsation of the radial or common carotid artery using applanation tonometry [12, 13]. Unfortunately, prospective studies have not proven that systemic arterial stiffness determined by these methods has an independent prognostic value for the development of CVD [14].
Currently, the most widespread determination of regional stiffness is by measuring pulse wave velocity (PWV) during sphygmography as the simplest and most reproducible technique [11]. There are 2 methods and, accordingly, 2 groups of devices for automatic recording of PWV. The first is based on synchronous recording of 2 pressure pulse waves (PPs) with subsequent analysis of the correlation between them [11]. Another method is based on sequential recording of the propagation time of PVs, provided they are synchronized relative to a simultaneously recorded electrocardiogram (ECG) [10, 11].
According to European and Russian recommendations (ESH, 2007; VNOK, 2008), measurement of carotid-femoral PWV is the “gold standard” for assessing aortic stiffness. When assessing subclinical lesions in middle-aged hypertensive patients, a PWV of more than 12 m/s was accepted as pathological [2, 11].
The latest ESH consensus statement (2012) recommended that aortofemoral PWV of more than 10 m/s be considered the threshold value [15]. The adjustments made to the indicator are due to the smaller true distance that the PV travels in the designated section of the arterial bed [3, 15].
Carotid-femoral PWV is measured by the “foot-to-foot” method, which involves synchronous graphical recording of arterial wall oscillations with sphygmotransducers over the projections of the carotid and femoral arteries, followed by calculation of the time by which the moment of appearance of one pulsation is delayed relative to the other [10, 11]. Japanese scientists have developed a method for recording PWV in the brachial- malleolar segment, which has demonstrated an independent correlation with the PV velocity in the aorta [16].
Another group of devices for determining PWV includes Doppler methods using specialized ultrasound devices. The propagation time required to measure the indicator is also determined between two PTs recorded simultaneously using 2 sensors or sequentially with one sensor synchronized with respect to the ECG [11, 17].
Local stiffness is studied by determining the diameter of superficial and deep arteries during the systolic and diastolic phases of the cardiac cycle. Classic two-dimensional ultrasound systems are used to assess carotid artery stiffness. Local aortic stiffness is measured using nuclear magnetic resonance and ultrasound echo tracking techniques. The latter is “dynamic tracking of the echo-contrast boundary” with devices with modules for highly accurate determination of arterial diameter [10, 11, 18].
Experts from the European Society of Cardiology believe that recording the arterial wave at the central level is preferable, i.e. in the ascending aorta, since it is this that reflects the true load on the left ventricle (LV) and the walls of the main arteries [3, 11]. In this case, PT must be assessed according to 3 main parameters: central systolic blood pressure (SBP) and pulse blood pressure (PBP), as well as the augmentation index. This is due to the independent prognostic value of the listed parameters when predicting the risk of death from all causes in patients with end-stage chronic renal failure (CRF), cardiovascular complications in patients undergoing percutaneous coronary intervention, in people suffering from hypertension [19-21].
To calculate the indicators described above, a recording of the blood flow of the radial artery is used, followed by a mathematical transformation using a transfer function. An alternative method is to analyze the central pressure wave from the common carotid artery. The registration of pulse fluctuations in the above sections of the arterial bed is based on the technique of applanation tonometry [11].
PV in large arteries consists of 2 components: a direct wave created by LV contraction, and reflected from the aortic bifurcation. It is important to emphasize the contribution of the reflected wave to the process of adequate functioning of the arterial system. Under conditions of preserved elasticity of the arteries, the PV, being reflected, returns to diastole, smoothes out blood pressure fluctuations and maintains an adequate level of diastolic blood pressure (DBP). This cushioning of blood flow by the aorta helps to minimize the work of the heart. In stiff arteries, early accelerated return of PV is observed. By joining the direct wave, the reflected pressure wave contributes to an increase in systolic pressure in the aorta [7].
Quantitative assessment of PT is possible by calculating the augmentation index, i.e. systolic wave growth index. This indicator allows you to estimate the relative magnitude of the reflected wave and is calculated as the difference between the first and second systolic peaks, expressed as a percentage of the heart rate-corrected BP. It directly depends on aortic stiffness and peripheral vascular resistance. The augmentation index is a relative value and can be calculated without calibration, while central PAP and SBP are absolute values and require calibration to determine them.
Conducting arteries are heterogeneous in their structure: the elasticity of the proximal vessels gradually decreases as they move to the distal ones. PWV varies accordingly: it increases from the center to the periphery. Thus, in the ascending aorta it is 4-5 m/s, and in the iliac and femoral arteries - 8-9 m/s [22, 23]. Along with an increase in PWV, the reflection of PV in places of numerous branches of the arteries causes an increase (“amplification”) of PV in the distal sections of the arteries compared to the central ones. Thus, SBP and PBP in the periphery, including those measured at the VA, will be higher than in the aorta and carotid artery. This applies primarily to young people, since it is in them that the elasticity of the central arteries is much higher than that of the peripheral ones. In some young healthy men, an increase in SBP during PA creates the preconditions for an unjustified diagnosis of isolated systolic arterial hypertension (ISAH), while this “amplification phenomenon” is associated primarily with a pronounced gradient of stiffness in the arterial system, and CBP remains normal. The results of prospective studies do not confirm the subsequent development of hypertension in individuals in this category [11]. There is also no evidence of a possible benefit of AHT. Consequently, measuring PBP on the PA, and not on the aorta and carotid artery, is sometimes not completely incorrect, especially in young people [11].
Currently, methods for daily recording of vascular stiffness have been developed, implemented in oscillometric and auscultatory devices for ambulatory blood pressure monitoring. The auscultatory method is based on recording the time interval from the beginning of the QRS
on the ECG until the V Korotkoff sound appears, and is designated
QKD
(
QRS
-Korotkoff Diastolic pressure delay) [24-27]. The oscillometric method is based on the synchronous recording of sphygmograms (oscillograms) of PA and ECG. The resulting indicator is a value averaged over all cardiac cycles within one blood pressure measurement, and is identified by the concept of pulse transit time - PTT [18, 28-30].
Pathogenetic aspects of vascular remodeling.
Different basins of the arterial bed have their own characteristics of the development of atherosclerosis, which is determined by their structure and functions. Therefore, all areas of the vascular bed are of potential interest for study - from the thoracic and abdominal aorta to the VA and arteries of the lower extremities.
Arterial remodeling includes functional disorders (endothelial dysfunction) and morphological restructuring - atherosclerosis, age-related involution of the most important structural proteins of the medial layer (elastin, fibulin, collagen). Impaired conduction function is associated with a decrease in the lumen of the arteries, which is accompanied by a decrease in tissue perfusion in the distal sections. Impaired damping function is associated with loss of elasticity of the arterial wall [31-34].
The stiffness of the aorta is determined primarily by the structure of the tunica media. The aortic wall is affected by several factors, the main ones being aging, hypertension, smoking, hypercholesterolemia, and type 2 diabetes [35].
The aging process is associated with the development of arteriosclerosis, which consists of fragmentation of elastin fibers, a decrease in the ratio of the content of the latter compared to collagen, and calcification of the tunica media. Another determinant of arteriosclerosis and decreased vascular compliance is hypertension, in which changes in the medial tunic of the great arteries, characteristic of “physiological” aging of blood vessels, develop prematurely. It must be emphasized that aortic stiffness progresses not only as a result of hypertension, but is itself a pathogenetic component of increased blood pressure [35].
Increased aortic stiffness is associated with changes in the functioning of the cardiovascular system. In particular, a less distensible aorta cannot effectively damp the volume of blood ejected by the LV, resulting in increased SBP. In turn, DBP decreases, which is accompanied by an increase in PBP. High blood pressure is transmitted to small arteries, and this leads to disruption of microcirculation, in particular cerebral and renal blood flow. Due to the increased PV velocity, reflected waves return earlier - in systole, which ultimately leads to decreased myocardial perfusion, LV hypertrophy (LVH) and systolic-diastolic dysfunction [35-37].
The mechanism of the negative effect of increased central blood pressure on the myocardium is as follows. One of the key functions of the heart is to pump blood through the arterial system to meet the metabolic needs of organs and tissues. The efficiency of cardiac output is determined by the contractility of the LV, the elasticity of the great arteries, and the total peripheral resistance. It is CBP, and not peripheral blood pressure, that determines the level of afterload on the LV walls during systole [22, 37].
Under conditions of increased vascular wall stiffness, the heart generates a higher final SBP for a given stroke volume, which requires greater energy expenditure [22]. Increased aortic SBP reduces cardiac output efficiency. A stable increase in central blood pressure contributes to the development of LVH, which itself is a major risk factor for the development of cardiovascular complications and cerebrovascular complications. The close relationship between central PAP and LVH is confirmed by the fact that LV mass is more closely correlated with PAP than with BP measured at the VA [38].
Increased large artery stiffness and hence central PAP are independently associated with diastolic dysfunction in hypertensive patients [39]. This plays a role in the occurrence of myocardial ischemia, ultimately leading to diastolic heart failure. This hypothesis is confirmed by the fact that risk factors for the development of diastolic heart failure - hypertension, atherosclerosis, age - are associated with increased arterial stiffness and central blood pressure.
Increased central blood pressure negatively affects coronary perfusion. As noted earlier, loss of aortic elasticity is accompanied by an increase in SBP, PBP and a decrease in DBP. Perfusion of the coronary arteries occurs predominantly during diastole. Against the background of decreased DBP, coronary blood flow decreases, which is especially unfavorable in conditions of high load on the LV (due to increased central SBP). This situation may contribute to myocardial ischemia and sudden cardiac death [40].
There is an alternative explanation: in stiff arteries, coronary perfusion, as a rule, also occurs during systole. Accordingly, when cardiac performance decreases, for example during acute coronary syndrome, blood flow in the coronary arteries is more sensitive to a decrease in systolic function than to diastolic function [41].
Thus, regardless of which mechanism underlies myocardial blood supply, changes in coronary perfusion as a result of increased arterial stiffness and central PAP predispose to LV ischemia and significantly increase the risk of developing coronary complications.
There is an important relationship between CBP and endothelial function. The vascular endothelium plays a key role in the homeostasis of the cardiovascular system. Biologically active substances secreted by endothelial cells, in particular endothelin-1 and nitric oxide, provide a powerful vasodilator effect. Nitric oxide also has anti-atherosclerotic effects due to inhibition of platelet aggregation, adhesion expression and proliferation of smooth muscle cells [42]. In conditions of loss of vascular elasticity, the release and bioavailability of nitric oxide decrease, which is the trigger for the formation of atherosclerotic plaque. This disorder increases the risk of developing coronary complications in a number of groups of CVD patients. In turn, decreased nitric oxide production may also lead to a further increase in arterial stiffness. Blockade of the synthesis of the active mediator is accompanied by a decrease in local compliance of the vascular wall [38, 43].
Prognostic value of arterial stiffness parameters.
The emergence of new data on the high prognostic significance of an increase in central SBP, PBP and arterial stiffness indicators is driving growing interest in the study of the elastic properties of the vascular wall, the assessment of which is increasingly used in clinical practice. A number of prospective studies have demonstrated the independent prognostic value of central hemodynamics and aortic stiffness for overall and cardiovascular mortality, fatal and non-fatal coronary complications, non-fatal strokes in patients with uncomplicated hypertension, type 2 diabetes, end-stage chronic renal failure, in elderly patients and in the general population [20, 44, 45]. Aortic stiffness retained its independent prognostic value after adjustment for classical risk factors, including PAD in the VA [46].
The results of large studies suggest that changes in the structural and functional state of the aortic wall play an important role in the pathogenesis of CVD. During the aging process, elastic arteries undergo more active remodeling. Accordingly, in older people, aortic stiffness may exceed peripheral stiffness [47].
In a study by P. Boutouyrie et al. [48] carotid-femoral PWV highly significantly correlated with the development of cardiovascular complications in patients with hypertension. It is important to note that the indicator remained significant when adjusted for Framingham risk factors. In addition, PWV in the aorta is a prognostic factor for cardiovascular disease, more reliable than 24-hour blood pressure monitoring, including in people with diabetes [45, 49]. An increase in PWV in the aorta and PBP on PA is the main marker of death from CVD in patients with end-stage chronic renal failure [20]. A study by S. Laurent et al. [50] demonstrated that after adjustment for central BP level, BP measured on PA lost its predictive value.
A number of studies have shown that CBP is a more reliable predictor of death from CVD and all causes than PA BP. The CAFE-ASCOT study demonstrated that 64–70% of patients with normal SBP levels measured on PA had central SBP consistent with grade 1 hypertension [51].
According to the results of the Strong Heart study, there is a stronger independent relationship between peripheral PBP and cardiovascular mortality than with traditional risk factors - LVH, decreased ejection fraction in adults without coronary heart disease. In addition, a 5-year follow-up period allowed central PAP to be identified as a more reliable predictor of CVD development than PAP measured on PA, presumably due to a more accurate reproduction of vascular load on the LV. The prognostic value of central PAD is significant, even if subclinical atherosclerosis is taken into account [46].
Historically, the surrogate outcome used to assess the effect of AHT has always been BP measured on PA. However, in recent years, the focus has been on CBP as a more important determinant of CV risk. The reason is that the dynamics of aortic blood pressure and those measured on PA against the background of AHT can differ significantly. In particular, research results have shown that β-blockers, compared with other groups of antihypertensive drugs, have a lesser effect on cardiovascular outcomes. According to the ASCOT, REASON studies and a number of comparative meta-analyses, atenolol, despite being equally effective as other drugs in lowering peripheral blood pressure, has a lesser effect on central blood pressure. The identified differences are due to the negative effect of the β-blocker atenolol on the amplitude of the reflected wave and the augmentation index, while all other antihypertensive drugs improve these parameters [52].
Thus, the results of recent large randomized clinical trials have confirmed a natural connection between subclinically developing vascular remodeling and the subsequent manifestation of CVD. Assessing the indicators of central blood pressure and stiffness certainly makes it possible to predict the course of the disease. Based on the results of measuring arterial stiffness and central PAP, a significant number of patients from the low and medium risk group can be transferred to groups at higher risk of developing cardiovascular disease [11].
Meanwhile, the experts of the working group on the treatment of hypertension (ESH/ESC recommendations 2013) believe that although the measurement of CBP and the augmentation index is of great interest for the development of non-invasive methods of analysis in pathophysiology, pharmacology and therapy, additional study is required before recommending their clinical use this question. The exception is young patients with ISAH: measuring CBP in people in this category in some cases allows one to avoid unjustified prescription of antihypertensive therapy.
The trend is nevertheless obvious - the introduction into medical practice of methods for determining the structural and functional properties of the main arteries and, first of all, the central blood pressure is a matter of the not so distant future, since dynamic assessment of the condition of the main arteries will significantly expand the possibilities of objective analysis of the effectiveness of pharmacotherapy for hypertension.