Coronary heart disease is a disease that occurs when there is a lack of oxygen in the myocardial tissues. Most often, the cause of this disease is the presence of atherosclerotic plaques in the main vessels, which in turn partially block the blood flow.
IHD has 2 forms – acute and chronic. Symptoms of the disease are: frequent attacks of angina pectoris (“angina pectoris”), rhythm disturbances, atrial fibrillation. Against the background of coronary artery disease, the risk of developing a heart attack increases, often with a fatal outcome.
Etiology of IHD
Previously, it was assumed that IHD mainly manifests itself only in men, since IHD was practically not recorded in women.
Currently, this disease is diagnosed in equal proportions in both men and women. Moreover, the age at which IHD is most often detected is “younger”, since people whose age does not exceed 45 years are at risk. The causes of the disease may be high blood pressure, bad habits (smoking, frequent drinking), excess weight, type 2 diabetes, genetic factors, physical inactivity, constant fatigue and exposure to stress factors.
The course of IHD is characterized by a wave-like character: against the background of the chronic course of the disease, attacks of angina often occur. In the early stages of the disease, symptoms intensify after exposure to excessive loads or after suffering stress. During such an attack, the patient experiences severe chest pain, respiratory function is impaired, and fear of death arises. The difference between an attack of coronary heart disease and myocardial infarction is the independent and rapid relief of symptoms. Subsequently, the number of attacks increases, and the disease becomes chronic.
The presence of coronary artery disease in a patient increases the risk of developing serious complications, especially without appropriate therapy. The main complications are: heart attack, heart failure and arrhythmias. All of these factors negatively affect the patient’s quality of life and can lead to disability, and in some cases, death. Every year, coronary heart disease kills more than 2 million people across the planet.
Hypertension with predominant heart damage without heart failure
Michael
1833 views
November 19, 2020
Hello! 36 years old, 83 kg, 192 cm, male Complaints: periodic pressure surges, underwent examination, verbally the doctor said that carvedilol should be increased from 12.5 to 25 once a day. When I read the diagnosis at home, I was stunned by “hypertension with primary damage to the heart without heart failure” and Possibly an enlargement of the left atrium Interatrial conduction disturbance The phenomenon of early ventricular repolarization How severe is the deviation from the norm? ——=======Stress echocardiography=======—— Initially: blood pressure 130/80 mmHg, heart rate 84 beats per minute During the test, a load of 12.7 METs was achieved. Duration of the test was: 12 min 29 sec At the height of the load, the heart rate was recorded: 166 beats per 1 min, 90% of the maximum heart rate, blood pressure 160x80 mm Hg. Reason for stopping the test: achievement of submaximal heart rate Load tolerance according to the test results: high Blood pressure response to load: adequate No significant ischemic changes in the ECG were noted Anginal attack: not recorded Echoradiography data Before load: LV walls with normal contractility After load: No disturbances in regional contractility revealed Conclusion: Test negative ——=======Electrocardiogram=======—— Heart rate: 60 beats per minute PQ: 141 ms QRS: 101 ms QT: 380 ms QTc: 388 ms Alpha angle: 37 Grad Regulation EOS: Intermediate ST: I 21 μV V1 -88 μV II 6 μV V2 121 MMV III -29 μV V3 155 μV AVR -4 μV v4 AVL 27 μV V5 197 197 μV AVF -11 μV Conclusion Conclusion : Sinus rhythm with heart rate 60/bpm Incomplete blockade of PNPG Possibly enlarged left atrium Impaired interatrial conduction Phenomenon of early ventricular repolarization ——=======Echocardiographic study (with calculations)=======—— Aorta diameter in the area of the sinuses of Valsalva 38 mm; diameter of the ascending aorta 32 mm; the walls are not changed. The left atrium diameter is 39 mm; indLP 1.81 cm/m2; LA volume 61 ml; LA volume index 28.24 ml/µV; MPP is not changed Left ventricle. MZhP 9 mm, CDR 50 mm, CL 10 mm, CDR index 2.31 cm/m2, FROM 0.38, EDV (Th) 118.24 ml, MM 169.80 g, IMM 78.61 g/m2 KDOV-mode 122 ml, EDC v-mode 46 ml , EDV index 56.48 ml/m2, ESV index 21.30 ml/m2, Simpson EF 62%, kinetics unchanged Right ventricle paramternal position 31 mm; 4-chamber 31 mm Right atrium area 17.3 cm2 Pulmonary artery 20 mm, estimated systolic pressure 23 mm Hg Inferior vena cava: 20 mm, burning on inspiration: >50% Aortic valve leaflets are not changed; Vmax 1.15 m/s, dPmax 5.32 mm Hg, no regurgitation The mitral valve leaflets are not changed; Ve 0.81 cm/s, Va 0.55 cm/s, Ve\Va 1.47, Tdec 137 ms, no regurgitation Tricusidal valve leaflets are not changed, regurgitation is valvular dPtr 17.74 mm Hg Pulmonary valve Vmax 0.73 m/s, dPmax 2 ,14 mm Hg, valvular regurgitation Description of the study: The heart chambers are not dilated. The walls of the LV are not thickened, the calculated values of the myocardial mass are not increased. Global contractility of the LV is not impaired. No zones of violation of regional contractility have been reliably identified. Normal diastolic function and LV filling pressure. E/Em-4.56 RV contractility according to TDI (TAVS = 14.0 cm/s) is preserved. TAPSE = 2.4 cm The IVS and IVS are located intact. During CDI mapping, no convincing evidence for transseptal blood shunting was obtained. The root, ascending section and arch (33 mm) of the aorta are not dilated, the walls are not changed. The pulmonary trunk is not dilated. The aortic valve is tricuspid, its crescents are not changed. Blood flow in the AC and in the LVOT is not accelerated. SV (LVOT) ~ 74ml. The leaflets of the mitral valve and tricuspid valves are not imzened. Mitral regurgitation is valvular. Tricuspid regurgitation, valvular. Estimated MPAP is not increased The amount of fluid in the periocardial cavity is not increased
The question is closed
aorta
maximum heart rate
estimated value
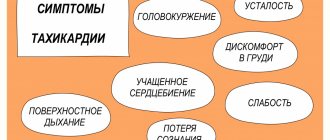
Symptoms of the disease
The main symptoms of IHD are heaviness in the chest and chest pain, the severity of which is determined only subjectively. Early detection and diagnosis will make it easier to treat the disease. Unpleasant sensations in the chest in older people, especially if they are permanent, should alert the patient. To find out the causes of pain, you should consult a doctor at our medical office for advice and treatment.
The possible presence of IHD may be due to the appearance of chest pain associated with physical or psychological stress. In addition, monotonous, incessant chest pain should also be examined after consulting a cardiologist, and you should consult a doctor regardless of the severity of symptoms, age and general condition of the person.
As a rule, coronary heart disease manifests itself in the form of paroxysms: attacks are followed by periods of calm. The disease can develop over several years, during this process its form may change, which affects the symptoms of IHD. Thus, the symptoms of IHD may vary widely.
Based on this, the most frequently occurring forms of IHD along with their symptoms will be described below. However, it must be emphasized that approximately 1/3 of patients with ischemia may not notice any symptoms and, accordingly, may not suspect the presence of the disease. Other patients often note pain in the chest, radiating pain (pain radiating to the back, arm, jaw), breathing problems, nausea, hyperhidrosis, tachycardia and arrhythmia.
Symptoms of hypertension
In the absence of treatment and secondary prevention, the disease progresses. Depending on the damage to target organs, they are distinguished: Stage I. Typically, but not necessarily, characterized by a mild and intermittent increase in blood pressure without target organ damage. However, it is quite possible for both a crisis and a completely asymptomatic course of the disease. In addition to high blood pressure, the patient may be concerned about:
- headache;
- decreased performance;
- tendency to fluid retention;
- fast fatiguability.
Stage II is characterized by the appearance of signs of damage to target organs (heart, kidneys and brain, as well as blood vessels, including the eyes, which may be accompanied by the appearance of new symptoms and complaints, as well as according to additional laboratory and instrumental studies:
- pain in the “heart area”;
- dizziness;
- visual impairment;
- the appearance of edema;
- memory loss;
- shortness of breath on exertion.
Stage III - complicated hypertension. The main sign of the course of the disease at this stage is severe damage to target organs with thrombosis, including heart attacks and strokes, accompanied by the following symptoms:
- hand tremors;
- noise in the head or ears;
- significant memory loss;
- nausea, vomiting;
- persistent visual impairment;
- various heart disorders.
Most of these symptoms are stable and usually progress, reducing performance.
Factors in the development of ischemic heart disease
The heart muscle, which is essentially the “motor” of the body, itself needs oxygen and unhindered blood flow. Blood flows to the heart through 2 coronary vessels. In the heart, both of these arteries are divided into small vessels that supply one of the sections of the myocardium.
There are simply no other vessels involved in feeding the heart with blood. Consequently, narrowing of the arteries or blockage of any of them leads to a lack of oxygen in the tissues of the heart and coronary disease develops.
One of the risk factors for the development of coronary artery disease is atherosclerosis of the great vessels and, as a consequence, the deposition of cholesterol on the walls of these arteries. As a result, plaques block blood flow, and the heart does not receive the required amount of blood.
In the early stages of the disease, the lack of oxygen in the heart is expressed only when the load increases, for example, during fast running. Pain that occurs in the chest is called angina pectoris. Over time, the lumen of the main vessels decreases, metabolic processes in the myocardium deteriorate, as a result of which the frequency of pain becomes more frequent; During the course of the disease, pain can occur during low-intensity exercise, as well as at rest.
Angina pectoris may be accompanied by the development of heart failure with the appearance of shortness of breath and fluid retention (due to the presence of edema).
When plaque detaches from the walls of the artery, blockage of the vessel can occur, thereby provoking the development of a heart attack and cardiac arrest. The severity of symptoms when heart tissue is damaged depends on the location of the blockage. Blockage of the main arteries can be fatal.
For the development of a heart attack, the vascular lumen must be reduced to 80% of the original. Rapid and sudden blockage of blood vessels prevents the heart from adapting to changes in blood flow and often leads to early death.
Symptoms of IHD are:
- Rhythm disorders
- Muscle weakness
- Feeling of heaviness behind the sternum
- Nausea
- Shortness of breath during moderate exercise
- Increased sweating
Symptoms of coronary heart disease are characterized by the occurrence of paroxysmal pain that lasts a short time. The feeling of tightness in the chest is popularly called “angina pectoris.” Ischemia and angina are distinguished by the presence of chest pain. As a rule, pain occurs in one part of the body and radiates to the arms, legs, shoulder blades, neck and jaw. Often, the symptoms of IHD can be confused with symptoms of gastrointestinal dysfunction. In such cases, heartburn and dyspeptic disorders may occur against the background of coronary artery disease. Therefore, a person may not suspect the presence of ischemia for a long time.
Ischemic disease is accompanied by:
- Mental stress
- Panic
- Bad mood
- Apathy
Also a symptom of the disease is pain in the chest that does not go away after using nitroglycerin. Often, coronary heart disease and angina are accompanied by constant pain that occurs suddenly, for example, this can happen while taking a shower, with a sudden change in temperature, while smoking, and also with sudden movements.
Most people often do not take the signs of IHD seriously and therefore do not consult a doctor for a long time. At the same time, the symptoms of IHD should not be left to chance, since complications of the disease can lead to dire consequences.
IHD is one of the causes of mortality from cardiovascular diseases in many countries, regardless of the level of development of medicine. If the patient has significant complications of this disease, for example, a significant decrease in the lumen of blood vessels, then for the treatment of IHD it is necessary to use surgical methods of therapy: coronary bypass surgery (replacing the affected vessel with an implant), angioplasty (insertion of a stent or balloon into the affected vessel) and other surgical procedures .
Treatment of ischemic disease consists of several stages:
- Pain relief and rest. In severe cases of coronary artery disease, epidural anesthesia should be used.
- Anticoagulation of blood and improvement of its rheological properties. It is necessary to conduct a laboratory examination of the blood, determine the level of platelets, measure the concentration of cholesterol in the blood and other parameters.
- Use of antiplatelet drugs. Treatment of coronary heart disease involves the mandatory use of such drugs, as they will help minimize the risk of developing blockage of blood vessels with blood clots.
- Prevention of atherosclerosis – one of the main causes of impaired blood flow.
- Diagnosis and appropriate therapy of other diseases. This includes other diseases of the heart and blood vessels, as well as disorders of the central nervous system.
- The use of prostaglandins.
- The use of medications that affect the transport of oxygen molecules. Such drugs include antihypoxants, calcium channel blockers and beta blockers. (They reduce the oxygen demand of heart tissue).
- Ultrasound diagnostics of the arteries of the heart, determination of gas exchange indicators and other examinations prescribed by a surgeon.
To relieve symptoms of ischemia, drugs containing potassium and magnesium are often used. They reduce the likelihood of thrombosis, normalize the elasticity of vascular walls, suppress the growth of cholesterol plaques, accelerate metabolic processes in the myocardium and energy exchange in it.
Hypertonic disease
Hypertension is a pathology of the cardiovascular system, developing as a result of dysfunction of higher centers of vascular regulation, neurohumoral and renal mechanisms and leading to arterial hypertension, functional and organic changes in the heart, central nervous system and kidneys. Subjective manifestations of high blood pressure include headaches, tinnitus, palpitations, shortness of breath, pain in the heart, blurred vision, etc. Examination for hypertension includes monitoring of blood pressure, ECG, echocardiography, ultrasound of the arteries of the kidneys and neck, urine analysis and biochemical parameters blood. Once the diagnosis is confirmed, drug therapy is selected taking into account all risk factors.
The leading manifestation of hypertension is persistently high blood pressure, i.e. blood pressure that does not return to normal levels after a situational rise as a result of psycho-emotional or physical stress, but decreases only after taking antihypertensive drugs. According to WHO recommendations, normal blood pressure is not exceeding 140/90 mmHg. Art. Exceeding the systolic reading over 140-160 mmHg. Art. and diastolic - over 90-95 mm Hg. Art., recorded at rest with double measurements during two medical examinations, is considered hypertension.
The prevalence of hypertension among women and men is approximately the same 10-20%; the disease most often develops after the age of 40, although hypertension is often found even in adolescents. Hypertension contributes to a more rapid development and severe course of atherosclerosis and the occurrence of life-threatening complications. Along with atherosclerosis, hypertension is one of the most common causes of premature mortality in the young working population.
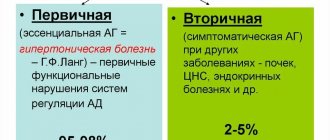
There are primary (essential) arterial hypertension (or hypertension) and secondary (symptomatic) arterial hypertension. Symptomatic hypertension accounts for 5 to 10% of hypertension cases. Secondary hypertension is a manifestation of the underlying disease: kidney diseases (glomerulonephritis, pyelonephritis, tuberculosis, hydronephrosis, tumors, renal artery stenosis), thyroid gland (thyrotoxicosis), adrenal glands (pheochromocytoma, Itsenko-Cushing syndrome, primary hyperaldosteronism), coarctation or atherosclerosis of the aorta, etc. .
Primary arterial hypertension develops as an independent chronic disease and accounts for up to 90% of cases of arterial hypertension. In hypertension, high blood pressure is a consequence of an imbalance in the body's regulatory system.
Mechanism of development of hypertension
The pathogenesis of hypertension is based on an increase in cardiac output and peripheral vascular resistance. In response to the influence of a stress factor, disturbances in the regulation of peripheral vascular tone by higher centers of the brain (hypothalamus and medulla oblongata) occur. A spasm of arterioles occurs on the periphery, including renal arterioles, which causes the formation of dyskinetic and dyscirculatory syndromes. The secretion of neurohormones of the renin-angiotensin-aldosterone system increases. Aldosterone, which is involved in mineral metabolism, causes retention of water and sodium in the vascular bed, which further increases the volume of blood circulating in the vessels and increases blood pressure.
With arterial hypertension, blood viscosity increases, which causes a decrease in the speed of blood flow and metabolic processes in tissues. The inert walls of the vessels thicken, their lumen narrows, which fixes a high level of total peripheral vascular resistance and makes arterial hypertension irreversible. Subsequently, as a result of increased permeability and plasma saturation of the vascular walls, the development of elastofibrosis and arteriolosclerosis occurs, which ultimately leads to secondary changes in organ tissues: myocardial sclerosis, hypertensive encephalopathy, primary nephroangiosclerosis.
The degree of damage to various organs in hypertension may be different, so there are several clinical and anatomical variants of hypertension with predominant damage to the vessels of the kidneys, heart and brain.
Classification of hypertension
Hypertension is classified according to a number of criteria: the reasons for the rise in blood pressure, damage to target organs, the level of blood pressure, the course, etc. Based on the etiological principle, they distinguish between: essential (primary) and secondary (symptomatic) arterial hypertension. According to the nature of the course, hypertension can have a benign (slowly progressive) or malignant (rapidly progressive) course.
The level and stability of blood pressure is of greatest practical importance. Depending on the level there are:
- Optimal blood pressure is <120/80 mmHg. Art.
- Normal blood pressure is 120-129/84 mm Hg. Art.
- Borderline normal blood pressure - 130-139/85-89 mm Hg. Art.
- Arterial hypertension of the 1st degree - 140-159/90-99 mm Hg. Art.
- Arterial hypertension II degree - 160-179/100-109 mm Hg. Art.
- Stage III arterial hypertension - more than 180/110 mm Hg. Art.
According to the level of diastolic blood pressure, the following types of hypertension are distinguished:
- Mild course - diastolic blood pressure < 100 mm Hg. Art.
- Moderate course - diastolic blood pressure from 100 to 115 mm Hg. Art.
- Severe - diastolic blood pressure > 115 mm Hg. Art.
Benign, slowly progressive hypertension, depending on target organ damage and the development of associated (concomitant) conditions, goes through three stages:
Stage I (mild and moderate hypertension) - blood pressure is unstable, fluctuating during the day from 140/90 to 160-179/95-114 mm Hg. Art., hypertensive crises occur rarely and are not severe. There are no signs of organic damage to the central nervous system and internal organs.
Stage II (severe hypertension) - blood pressure in the range of 180-209/115-124 mm Hg. Art., hypertensive crises are typical. Objectively (with physical and laboratory examination, echocardiography, electrocardiography, radiography), narrowing of the retinal arteries, microalbuminuria, increased creatinine in the blood plasma, left ventricular hypertrophy, and transient cerebral ischemia are recorded.
Stage III (very severe hypertension) – blood pressure from 200-300/125-129 mm Hg. Art. and higher, severe hypertensive crises often develop. The damaging effect of hypertension causes the phenomena of hypertensive encephalopathy, left ventricular failure, the development of thrombosis of cerebral vessels, hemorrhages and edema of the optic nerve, dissecting vascular aneurysm, nephroangiosclerosis, renal failure, etc.
Risk factors for developing hypertension
The leading role in the development of hypertension is played by disruption of the regulatory activity of the higher parts of the central nervous system, which control the functioning of internal organs, including the cardiovascular system. Therefore, the development of hypertension can be caused by frequently repeated nervous overstrain, prolonged and severe anxiety, and frequent nervous shocks. The occurrence of hypertension is facilitated by excessive stress associated with intellectual activity, night work, and exposure to vibration and noise.
A risk factor in the development of hypertension is increased salt intake, which causes arterial spasm and fluid retention. It has been proven that consuming >5 g of salt per day significantly increases the risk of developing hypertension, especially if there is a hereditary predisposition.
Heredity, aggravated by hypertension, plays a significant role in its development in close relatives (parents, sisters, brothers). The likelihood of developing hypertension increases significantly if two or more close relatives have hypertension.
Arterial hypertension in combination with diseases of the adrenal glands, thyroid gland, kidneys, diabetes mellitus, atherosclerosis, obesity, chronic infections (tonsillitis) contribute to the development of hypertension and mutually support each other.
In women, the risk of developing hypertension increases during menopause due to hormonal imbalance and exacerbation of emotional and nervous reactions. 60% of women develop hypertension during menopause.
Age factors and gender determine an increased risk of developing hypertension in men. At the age of 20-30 years, hypertension develops in 9.4% of men, after 40 years - in 35%, and after 60-65 years - in 50%. In the age group under 40 years, hypertension is more common in men; in older age groups, the ratio changes in favor of women. This is due to a higher rate of male premature mortality in middle age from complications of hypertension, as well as menopausal changes in the female body. Currently, hypertension is increasingly being detected in people at a young and mature age.
Alcoholism and smoking, poor diet, excess weight, physical inactivity, and poor ecology are extremely conducive to the development of hypertension.
Symptoms of hypertension
The course of hypertension is varied and depends on the level of increase in blood pressure and the involvement of target organs. In the early stages, hypertension is characterized by neurotic disorders: dizziness, transient headaches (usually in the back of the head) and heaviness in the head, tinnitus, pulsation in the head, sleep disturbance, fatigue, lethargy, a feeling of weakness, palpitations, nausea.
Later, shortness of breath occurs when walking quickly, running, exercising, or climbing stairs. Blood pressure is persistently above 140-160/90-95 mm Hg. (or 19-21/12 hPa). Sweating, redness of the face, chill-like tremor, numbness of the toes and hands are noted, and dull, prolonged pain in the heart area is typical. With fluid retention, swelling of the hands (“ring symptom” - it is difficult to remove the ring from the finger), swelling of the face, puffiness of the eyelids, and stiffness are observed.
In patients with hypertension, there is a veil, flickering of flies and lightning before the eyes, which is associated with vasospasm in the retina; There is a progressive decrease in vision; retinal hemorrhages can cause complete loss of vision.
Complications of hypertension
With a long-term or malignant course of hypertension, chronic damage to the blood vessels of target organs develops: the brain, kidneys, heart, eyes. Instability of blood circulation in these organs against the background of persistently elevated blood pressure can cause the development of angina pectoris, myocardial infarction, hemorrhagic or ischemic stroke, cardiac asthma, pulmonary edema, dissecting aortic aneurysm, retinal detachment, uremia. The development of acute emergency conditions against the background of hypertension requires a decrease in blood pressure in the first minutes and hours, as it can lead to the death of the patient.
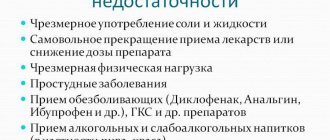
The course of hypertension is often complicated by hypertensive crises - periodic short-term increases in blood pressure. The development of crises may be preceded by emotional or physical overstrain, stress, changes in meteorological conditions, etc. In a hypertensive crisis, there is a sudden rise in blood pressure, which can last several hours or days and is accompanied by dizziness, severe headaches, a feeling of heat, palpitations, vomiting, cardialgia , visual impairment.
During a hypertensive crisis, patients are frightened, excited or inhibited, and drowsy; in severe cases they may lose consciousness. Against the background of a hypertensive crisis and existing organic changes in blood vessels, myocardial infarction, acute cerebrovascular accidents, and acute left ventricular failure can often occur.
Diagnosis of hypertension
Examination of patients with suspected hypertension has the following goals: to confirm a stable increase in blood pressure, exclude secondary arterial hypertension, identify the presence and degree of damage to target organs, assess the stage of arterial hypertension and the degree of risk of complications. When collecting anamnesis, special attention is paid to the patient’s exposure to risk factors for hypertension, complaints, level of increase in blood pressure, the presence of hypertensive crises and concomitant diseases.
Dynamic measurement of blood pressure is informative for determining the presence and degree of hypertension. To obtain reliable blood pressure levels, the following conditions must be met:
- Blood pressure measurement is carried out in a comfortable, quiet environment, after 5-10 minutes of patient adaptation. It is recommended to exclude smoking, exercise, eating, tea and coffee, and the use of nasal and eye drops (sympathomimetics) 1 hour before measurement.
- The patient's position is sitting, standing or lying down, with the arm at the same level as the heart. The cuff is placed on the shoulder, 2.5 cm above the fossa of the elbow.
- At the patient's first visit, blood pressure is measured in both arms, with repeated measurements after a 1-2 minute interval. If blood pressure asymmetry is > 5 mm Hg, subsequent measurements should be carried out on the arm with higher values. In other cases, blood pressure is usually measured on the “non-working” arm.
If blood pressure readings differ from each other during repeated measurements, then the arithmetic mean is taken as the true one (excluding the minimum and maximum blood pressure readings). In case of hypertension, self-monitoring of blood pressure at home is extremely important.
Laboratory tests include clinical blood and urine tests, biochemical determination of the level of potassium, glucose, creatinine, total blood cholesterol, triglycerides, urine analysis according to Zimnitsky and Nechiporenko, Rehberg test.
On electrocardiography in 12 leads in hypertension, left ventricular hypertrophy is determined. ECG data is clarified by echocardiography. Ophthalmoscopy with fundus examination reveals the degree of hypertensive angioretinopathy. An ultrasound scan of the heart determines enlargement of the left chambers of the heart. To determine target organ damage, ultrasound of the abdominal cavity, EEG, urography, aortography, CT scan of the kidneys and adrenal glands are performed.
Treatment of hypertension
When treating hypertension, it is important not only to lower blood pressure, but also to correct and reduce the risk of complications as much as possible. It is impossible to completely cure hypertension, but it is quite possible to stop its development and reduce the frequency of crises.
Hypertension requires the combined efforts of the patient and the doctor to achieve a common goal. At any stage of hypertension it is necessary:
- Follow a diet with increased consumption of potassium and magnesium, limiting the consumption of table salt;
- Stop or sharply limit alcohol intake and smoking;
- Get rid of excess weight;
- Increase physical activity: it is useful to engage in swimming, physical therapy, and walking;
- Take prescribed medications systematically and for a long time under the control of blood pressure and dynamic supervision of a cardiologist.
For hypertension, antihypertensive drugs are prescribed that depress vasomotor activity and inhibit the synthesis of norepinephrine, diuretics, β-blockers, antiplatelet agents, hypolipidemic and hypoglycemic drugs, and sedatives. The selection of drug therapy is carried out strictly individually, taking into account the entire range of risk factors, blood pressure levels, the presence of concomitant diseases and target organ damage.
The criteria for the effectiveness of treatment of hypertension is the achievement of:
- short-term goals: maximum reduction in blood pressure to a level of good tolerance;
- medium-term goals: preventing the development or progression of changes in target organs;
- long-term goals: prevention of cardiovascular and other complications and prolongation of the patient’s life.
Prognosis for hypertension
The long-term consequences of hypertension are determined by the stage and nature (benign or malignant) of the disease. Severe course, rapid progression of hypertension, stage III hypertension with severe vascular damage significantly increases the frequency of vascular complications and worsens the prognosis.
With hypertension, the risk of myocardial infarction, stroke, heart failure and premature death is extremely high. Hypertension has an unfavorable course in people who become ill at a young age. Early, systematic therapy and blood pressure control can slow the progression of hypertension.
Prevention of hypertension
For primary prevention of hypertension, it is necessary to exclude existing risk factors. Moderate physical activity, a low-salt and low-cholesterol diet, psychological relief, and giving up bad habits are useful. It is important to early identify hypertension through monitoring and self-monitoring of blood pressure, follow-up of patients, adherence to individual antihypertensive therapy and maintenance of optimal blood pressure levels.
Diagnosis of IHD
The main objectives of the survey are:
- Determination of risk factors - high blood pressure, high cholesterol concentrations, diabetes mellitus, chronic renal failure.
- Assessment of heart function.
- Analysis of the condition of the great vessels.
- Choosing a method of therapy.
- Prognosis of the need for surgical intervention.
Observation by a cardiologist
Patients with confirmed coronary artery disease should visit a cardiologist more often and receive appropriate advice from him. If new risk factors are discovered and the condition worsens, emergency surgery may be necessary. If the patient’s diagnosis is complicated by diabetes mellitus or he has high blood sugar, he is recommended to consult an endocrinologist and prescribe a treatment plan.
Medical specialists will listen to all your problems and provide all the necessary qualified assistance.
What tests need to be done
Blood tests:
- CBC - a general blood test helps assess the condition of the blood.
- Donating blood to determine glucose levels - detecting diabetes mellitus.
- Indicators of total cholesterol, HDL and LDL (high and low density lipoproteins, respectively), triglyceride levels.
- Determination of urea and creatinine levels shows kidney function. Diagnosis of the excretory system is very important, since the kidneys are target organs for the development of hypertension and some cardiovascular diseases.
Urine tests:
- Presence of protein in urine tests. Determines the degree of destruction of kidney tissue.
- Measuring albumin levels in urine. Albumin concentration may identify additional risk factors for CAD.
Other types of diagnostics:
- Determination of blood pressure indicators. If necessary, to confirm hypertension, daily blood pressure monitoring may be prescribed - ABPM or treadmill.
- Chest X-ray – helps study the size of the heart and congestion in the lungs.
- Echocardiography (ECG) – shows the electrical conductivity of the heart. Prescribed to detect rhythm disturbances and signs of a heart attack.
- Holter heart monitoring is a periodic ECG throughout the day, performed using a special device attached to a person’s belt. The sensors are attached at chest level, the device is adjusted and the patient is allowed to go home for a day. Doctors often recommend keeping a diary during a Holter mount; in it, as a rule, they record the time and nature of pain, as well as the level of physical activity on the day of the examination. An undoubted advantage of Holter is its ability to assess heart function in normal everyday conditions, since when measured on stationary ECG equipment, patients may experience “white coat” syndrome, in which ECG readings may be interpreted incorrectly.
- Stress test (ECG on a bicycle ergometer or treadmill) – recording an ECG and measuring blood pressure during physical activity. Helps determine the functioning of the heart and blood vessels, as well as differentiate angina from other chest pains.
- Echocardiography (ECHO-CG, ultrasound of the heart) – helps to analyze the structure of the myocardium and evaluate the functions of the heart valves.
- Coronary angiography is an X-ray diagnosis of the heart. Using a probe from the femoral artery, a contrast agent is injected into the coronary vessels, then X-rays are taken. The contrast contains isotopes that are highlighted in the image, so this diagnostic procedure helps determine the exact location of plaques and the severity of narrowing of the main arteries of the heart.
Development of hypertension
The essence of the disease is frequent and/or persistent increase in blood pressure.
The origin of the disease is still unknown, but there is disruption of the heart and increased vascular tone. Depending on the level of high blood pressure, there are three degrees of severity of hypertension: 1 degree (mild, soft) - the patient’s pressure is in the range from 140/90 to 159/99; 2nd degree (moderate) - pressure ranges from 160/100 to 179/109; Grade 3 (severe) - blood pressure above 180/110.
Treatment methods for coronary heart disease
To accurately diagnose a patient with coronary artery disease, it is necessary to conduct a complete examination of the heart and blood vessels, which includes:
- Echocardiography (ECHO-CG).
- Electrocardiogram (ECG).
- Coronary angiography.
- Measuring blood cholesterol and triglyceride levels.
To treat coronary heart disease, the first step is to eliminate all negative factors that negatively affect the course of the disease: if you smoke, you need to quit smoking, limit alcohol consumption, exercise, maintain normal blood pressure levels, lose weight, reduce cholesterol levels (if it is high) and reconsider your diet (try to eat right).
In special cases, to normalize blood flow in the heart, special surgical procedures on damaged main arteries are indicated:
- Angioplasty involves installing a stent or balloon in an artery of the heart. The operation is performed under x-ray. During angioplasty, a balloon catheter is inserted into the artery and guided towards the narrowed artery. The functions of the balloon are to push through cholesterol plaques, as if “smoothing” them. If this does not happen, then a special stent is installed in this place, preventing the vascular lumen from narrowing.
- Coronary artery bypass grafting is a rather complex surgical operation that uses artificial blood circulation. Part of the blocked vessel is bypassed using a vein taken from the leg or arm. The new artery joins the aorta and coronary artery. In this way, the blocked vessel is excluded from the circulatory system. In other words, during the operation, a bypass of the blood is made, bypassing the artery in which the lumen has narrowed.
Degrees and stages of hypertension
Hypertension is classified according to stages and degrees. The division into degrees is based on the level of pressure rise:
- I degree - rise in systolic pressure above 139 up to 159 mm Hg. art (diastolic fluctuates in the range of 90-99 mm Hg);
- II degree - from 160 to 170 mm Hg. Art. (diastolic oscillation interval - 100-109);
- III degree - pressure rises above 180 mm Hg. Art.
The stage of hypertension also takes into account the degree of target organ damage:
- Stage 1 (low risk) - mild hypertension, in which there is no damage to target organs;
- Stage 2 (high risk) - moderate or severe course of the disease, in which target organs are involved in the process: cardiac hypertrophy, spasm of the retinal arteries, deterioration of renal blood flow;
- Stage 3 (very high risk) - an extremely severe course, accompanied by frequent hypertensive crises and dangerous damage to target organs in the form of stroke, heart attack, and retinal hemorrhages.
Operations for ischemic heart disease
Surgery for the treatment of coronary heart disease has become quite common among cardiac surgeons, in particular, it is often used in the treatment of angina pectoris. The greatest effectiveness is demonstrated by operations during which blood circulation is restored in vessels with the presence of cholesterol plaques. The main operation to normalize blood flow is coronary bypass surgery. An alternative option is angioplasty using a balloon or spring stent.
Surgical treatment is often used in the presence of a cardiac aneurysm that developed after a heart attack. The task of surgeons in this case is to prevent heart failure associated with the aneurysm. During the operation, the aneurysm is resected, and surgeons remove the platelets that have accumulated in it. Surgical treatment of ischemia is carried out using artificial circulation.
Treatment of hypertension
To treat the disease, both drug and non-drug therapy are used. Hypertension medications are aimed at preventing high blood pressure. The doctor also recommends lifestyle changes, such as a special diet or moderate exercise. In our clinics on Gorokhovaya St., 14/26
(metro station Admiralteyskaya, Admiralteysky district) and on
Varshavskaya st., 59
(metro station Moskovskaya, Moskovsky district) there are
therapists
and
cardiologists
who will diagnose and draw up a suitable treatment plan for hypertension.
You can make an appointment by calling 493-03-03 or on our website. Make an appointment
Necessary preventive measures
Proper nutrition, including a sufficient amount of proteins, fats and carbohydrates, serves as a preventive measure for coronary heart disease. You should also exclude from your diet foods containing large amounts of cholesterol and animal fats. Vegetables, fruits, lean meat, fish and seafood are allowed to be consumed with virtually no restrictions. To create an individual diet, it is recommended to consult a nutritionist.
Factors that positively affect the health of the heart and blood vessels:
- Normal body weight. It is calculated using the BMI formula (height in cm divided by the square of height in meters). To lose weight, you should consume a strictly defined amount of calories, if possible not to exceed the norm. Plus, it is also recommended to remove simple carbohydrates from your diet and minimize sugar consumption.
- Sports activities. Even light walks and exercise will help improve heart function.
- Elimination of stress factors.
- Bad habits should be eliminated. Quit smoking and limit your alcohol consumption.
- Controlling blood pressure.
Early detection and treatment of IHD virtually eliminates the development of complications.
Diet
A diet for coronary artery disease involves reducing the consumption of animal fats, since such foods contribute to the deposition of cholesterol plaques in the coronary arteries and are the main factor in the development of coronary artery disease.
The amount of fat in the diet of a person with coronary heart disease should not exceed 85g. per day. It is recommended to replace some of the saturated fats with unsaturated fats, for example, add more fish containing Omega-3 fats to your diet.
Fats, as a rule, are found in baked goods, processed meats (sausages, sausages), milk, etc., therefore, you should also limit yourself from consuming foods of this type.
If you have coronary artery disease, a person should reduce cholesterol-containing foods. Plus, it is necessary to minimize the amount of sweets and ice cream consumed.
Milk, especially those with a high fat content, should also not be consumed frequently. Limit your consumption of cottage cheese and cheese, which contain large amounts of animal fat.
Herbal preparation "Cardioton" for the prevention of coronary heart disease
Coronary heart disease is a serious disease, which is also quite common among older and elderly people. Heart problems are a major risk factor for death. Severe forms of IHD are difficult to treat and often lead to the development of complications. An attack of angina that occurs against the background of coronary artery disease can contribute to the development of myocardial infarction. Any disease is easier to prevent than to treat, every specialist will tell you this, however, in most cases, people put health in the background, sometimes forgetting about the most important thing. Preventing heart disease should be done even in the absence of any heart symptoms. To prevent heart disease, it is recommended to use the natural drug “Cardioton”. The drug is also necessary for a person to normalize the work of the myocardium, restore its contractile function and improve blood circulation in the coronary vessels, since these factors are the root causes of the development of ischemia.
Diagnosis of hypertension
Diagnosis of hypertension is performed by a cardiologist. To identify the disease and individualize treatment, the following methods are used:
- dynamic blood pressure measurement;
- laboratory tests - clinical and biochemical blood tests, general urine analysis;
- electrocardiography, including in the form of Holter monitoring;
- ultrasound examinations: heart, kidneys and other organs;
- Dopplerography (ultrasound of blood vessels).