In the medical literature, Behçet's disease is often called Touraine's aphthosis major or Adamantiad syndrome. This rare disease belongs to the category of systemic chronic pathologies with unknown causes. The peculiarity of this defect lies in the fact that several types of symptoms are simultaneously observed with it. Although, against the background of a pronounced clinical picture, other anomalies can be identified.
Most often, Behçet's disease occurs in Japan and Mediterranean countries, among which it is worth highlighting Turkey with a very unusual cuisine. Tourists from other areas do not always notice differences in food habits. In addition to belonging to the indigenous populations of the Mediterranean and Japan, people who consume too many walnuts should be considered at risk.
You may be interested in: Bronze disease: possible causes, symptoms and treatment
General information
Initially, the description of Behcet's syndrome included the mandatory presence of several symptoms:
- iritis - inflammation of the iris;
- hypopyon - purulent contents in the lower part of the eye;
- ulcers on the mucous membranes of the genitals and oral cavity.
You will be interested in: “Diprospan”: analogues and substitutes, instructions for use, reviews
The disease owes its name to the Turkish dermatologist Behçet, who actually described its features and proposed classifying it into a separate nosological group. A few years earlier, this pathology was studied by another Greek doctor, Adamantiad. That is why some sources mention the double name of the disease - Behçet-Adamantiad syndrome.
True, in fact, the first information about such a rare vice is found in the works of Hippocrates from 377 BC. It was this scientist who described eye damage, causing blindness, accompanied by ulcerative injury to the skin and mucous membranes, mainly in residents of Asia Minor.
According to the ICD, Behçet's disease is coded M35.2.
Causes
The exact cause of the disease is unknown. Behcet's syndrome is believed to be caused by an autoimmune reaction (the body's immune system, whose normal function is to protect the body from harmful foreign agents and influences, mistakenly attacks some of its own tissues and organs). The “attack” that the immune system carries out against the body is called an autoimmune response. This causes an inflammatory process in the affected tissues and organs.
It is believed that some people are genetically predisposed to this type of immune system response, i.e., to factors that can stimulate and provoke an autoimmune attack. Some viruses and bacteria are also suspected of causing this. People with common streptococcal infections are known to be more likely to develop Behcet's syndrome.
The disease is not contagious, that is, it cannot be transmitted from person to person.
At-risk groups
Taking into account the fact that the pathology occurs most often in the territory between the Mediterranean and Asia, it is also often called the Silk Road defect. In other areas, cases of Behcet's disease are recorded extremely rarely.
You will be interested in: “Blepharogel-2”: instructions for use, reviews
The disease is most common in Turkey, followed by Japan, Saudi Arabia, Iran and Korea. In other countries, the incidence is only one case per 100 thousand people.
Behçet's disease is diagnosed much more often in men than in women. The only exceptions are Japan and Korea - here the pathology mainly affects the female population. The first signs usually appear in patients over 40 years of age.
References
- Behçet's disease (BD). Clinical recommendations. 2021
- Shenavandeh S, Jahanshahi KA, Aflaki E, Tavassoli A. Frequency of HLA-B5, HLA-B51 and HLA-B27 in patients with idiopathic uveitis and Behçet's disease: a case-control study. Reumatologia. 2018;56(2):67-72. doi: 10.5114/reum.2018.75516. Epub 2021 May 9. PMID: 29853720; PMCID: PMC5974627.
- Sakly K, Lahmar R, Nefzi F, Hammami S, Harzallah O, Sakly N, Sakly W, Hassine M, Mahjoub S, Ghedira I, Feki S. Phenotypic abnormalities of peripheral blood mononuclear cells in patients with Behçet's disease and association with HLA- B51 expression. Immunol Invest. 2014;43(5):463-78. doi: 10.3109/08820139.2014.886260. Epub 2014 Mar 24. PMID: 24661088.
- Shadmanfar S, Shahram F, Nadji A, Akhlaghi M, Faezi ST, Sadeghi-Abdollahi B, Faridar A, Madanchi N, Davatchi F. The relationship between plasma homocysteine level and HLA-B51 in patients with Behcet's disease: a case-control study . Int J Rheum Dis. 2014 May;17(4):466-70. doi:10.1111/1756-185X.12271. Epub 2014 Jan 16. PMID: 24428874.
Etiology of the disease
The specific causes of Behcet's disease have not yet been identified. Today there are two theories of the appearance of pathology: genetic and infectious. Taking into account the fact that the defect is much more common in older people, it is likely that hereditary predisposition in combination with external harmful factors plays an important role.
Genetically, people who have HLA-B51 antigens and abnormal levels of cytokines IL-6, 17, 8, 21 are more susceptible to the disease.
As for the infectious theory of the development of the disease, the main place in it is given to streptococci, herpetic viruses and mycobacterium tuberculosis.
Among other things, the appearance of this defect can be influenced by prolonged abuse of alcohol, drugs, tobacco, and the presence of autoimmune pathologies, which are accompanied by damage to the mucous membranes.
Prevention
There is no specific prevention against Behçet's disease because its causes are not clear. We can only highlight the main points that will help maintain normal immunity:
- promptly treat infectious diseases;
- stop chronic infectious diseases;
- monitor your daily routine;
- regulate physical activity;
- stop taking uncontrolled medications;
- strictly follow the doctor's instructions;
- take measures to boost immunity;
It is recommended to follow a hypoallergenic diet with a high fiber content.
Danger of the syndrome
What consequences can Behcet's disease have for the patient? The syndrome can lead to:
- generalized aphthous stomatitis;
- deep ulcers on the mucous membranes of the vagina, penis, mouth, scrotum;
- large scars instead of ulcers.
If a bacterial infection occurs, the resulting ulcers may fill with pus. Skin symptoms of the disease are characterized by the occurrence of papulovesicular rashes, vasculitis of varying severity, erythema nodosum, purulent pustules, and pyoderma. Many patients also experience hair loss in the form of stellar alopecia.
If joints are involved in the pathological process, symmetrical polyarthritis occurs, which is characterized by the absence of destructive changes.
The appearance of uveitis provokes blurred vision, photophobia, chronic lacrimation, fogginess and blurred images. The development of this condition can lead to complete blindness.
Publications in the media
Behçet's disease (Behçet's syndrome, Touraine's major aphthosis) is a systemic chronic disease of unknown etiology with a relapsing course, manifested by a characteristic triad: recurrent aphthous stomatitis, ulcerative changes in the mucous membrane and skin of the genital organs, eye damage in the form of uveitis or iridocyclitis. Additionally, damage to other organs is possible - arthritis, thrombophlebitis, colitis, and neurological symptoms often occur. Statistical data. The disease is common in Japan and Mediterranean countries (including Turkey). Prevalence in the USA is 1:100,000, in Russia - 3:100,000, in Japan - 670:100,000. The predominant age is 30–40 years. The predominant gender is male (2:1).
Genetic aspects. Several cases of familial disease have been described. The disease is listed in the McKusick Catalog of Inherited Diseases (109650). In Japan and Mediterranean countries, the disease is associated with HLA B5 and HLA DR5 Ag.
Risk factors • Consumption of large quantities of walnuts • Belonging to indigenous ethnic groups of the Mediterranean, Japan, Middle East.
Pathomorphology • Mononuclear perivascular infiltration • Swelling of endothelial cells • Partial obliteration of the vascular lumen • Mononuclear infiltration of the synovial membrane • Neutrophilic dermatitis, consistent with the picture of Sweet's syndrome • There may be no morphological changes.
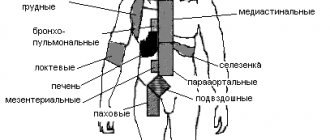
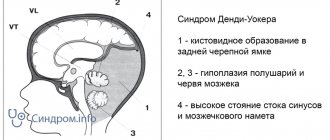
Clinical picture • Oral mucosa: aphthous stomatitis (99%). Ulcers - shallow, painful, last from several days to several weeks, heal without a scar • Genital organs •• men - painful ulcers on the skin of the penis and scrotum •• women - ulcers on the mucous membrane of the vulva and vagina, often painful • Eye lesions: iritis, iridocyclitis, chorioretinitis, hypopyon (accumulation of pus in the anterior chamber of the eye), retinal hemorrhages, disc edema, optic nerve atrophy • Skin manifestations - papulovesicular rash, changes like erythema nodosum, vasculitis, pyoderma. Possible patchy hair loss. The formation of a purulent pustule at the injection site of any drug is very specific • Joint damage •• Morning stiffness occurs in 30% of patients •• Symmetrical polyarthritis of large joints of the lower extremities without signs of destruction • Thrombophlebitis: superficial veins, less often - pulmonary veins, cerebral veins • Neurological symptoms : damage to cranial nerves; symptoms reminiscent of multiple sclerosis, pyramidal insufficiency. In the cerebrospinal fluid - lymphocytosis, normal content of g-globulins • Gastrointestinal tract damage: aphthous-ulcerative changes in the gastrointestinal mucosa, often clinically indistinguishable from those with ulcerative colitis or Crohn's disease • Lung damage: thrombosis or PE, less often - pulmonary infiltrates, pleurisy • Rarely Myopathy or myositis, gangrene, epididymitis, glomerulonephritis, and schizoaffective disorders occur.
Laboratory data • Increased ESR (not always) • Detection of immune complexes, cryoglobulins in the blood serum • Hypergammaglobulinemia • Complement levels are normal or elevated • Abs to mucosal cells • RF absent • ANATs absent • Abs to cytoplasmic Ag of neutrophils • Demyelinating Abs in nerve damage systems • Antiphospholipid antibodies • The degree of decrease in the level of antithrombin III in the blood plasma correlates with the activity of the process • An increase in fibrinolytic activity of plasma occurs during exacerbation of the disease • In the synovial fluid there are 5000–20,000 leukocytes per 1 μl, neutrophils predominate.
Arteriography to detect aneurysms or thrombosis.
Diagnostic tactics. In Russia, Behcet's disease should be assumed after excluding other causes of ulceration of the mucous membranes.
International Diagnostic Criteria (1990) • Major criterion - recurrent oral ulceration, at least 3 times within 12 months • Minor criteria •• Recurrent genital ulceration •• Eye involvement (anterior uveitis, posterior uveitis, vitreous opacities) •• Skin lesion (resembling erythema nodosum or pseudofolliculitis; acne-like nodules in a postpubertal patient not receiving GC) •• Positive pathergy test: erythematous papule with a diameter of more than 2 mm after pricking with a sterile needle under the skin to a depth of 5 mm (assessed after 48 hours) .
To make a diagnosis, 1 major and 2 minor criteria are needed. Note: the criteria can be applied only in the absence of other pathology that could determine their presence.
TREATMENT
General tactics. It is based on immunosuppressive therapy (local for changes in the mucous membranes, systemic for the treatment of extramucosal manifestations). No specific regimen or diet was suggested.
Drug treatment
• For systemic reactions (fever, eye damage, central nervous system) •• Prednisolone 1 mg/kg/day or pulse therapy with methylprednisolone 1 g IV daily for 3 days. For posterior uveitis, if there is no improvement after hormone therapy, cyclosporine 5 mg/kg/day with a gradual increase in dose to 10 mg/kg/day until a therapeutic effect develops (therapeutic concentrations of cyclosporine in blood plasma are 50–200 ng/ml) •• Cytostatic agents (primarily for meningoencephalitis or eye damage) ••• Chlorambucil 0.1–0.2 mg/kg long-term (up to 2 years) ••• Azathioprine 2–3 mg/kg/day ••• Cyclophosphamide 50–100 mg/day in the morning. The patient should be warned about the need to drink at least 8-10 glasses of water during the day and if hematuria occurs, consult a doctor. Medicines should be taken orally due to the ease of formation of post-injection suppurations.
• For thrombophlebitis - acetylsalicylic acid 320 mg/day.
• In case of resistance to treatment, the use of intravenous immunoglobulin at 0.2–2 g/kg/day is recommended for 4–5 days.
Complications • Blindness • Central and peripheral paresis and paralysis • Pulmonary embolism (rare) • Vascular aneurysms • Amyloidosis.
Course and prognosis. The life expectancy of patients with damage to the nervous system is shorter than in the general population. Other manifestations (except for vascular accidents and the development of complications) do not affect life expectancy.
ICD-10 • M35.2 Behcet's disease.
Applications • MAGIC syndrome - a variant of Behçet's syndrome (English M outh A nd G enital Ulcers and Interstitial Chondritis oral ulcers, interstitial chondritis) • Mollare meningitis. More often it occurs in the form of recurrent forms of aseptic meningitis: fever, headache, malaise, meningeal signs, monocytes and endothelial-like cells in the cerebrospinal fluid.
Possible consequences of the vice
Among other things, Behçet's disease may well be accompanied by damage to the digestive system, which makes differential diagnosis with Crohn's disease and nonspecific colitis more difficult.
You may be interested in:Yellow nails: causes and treatment
Some patients may experience:
- nonspecific arthritis;
- pleurisy;
- gangrene;
- thrombosis;
- amyloidosis;
- pulmonary embolism;
- myositis;
- renal failure;
- myopathies;
- schizoaffective mental disorders.
In women with Behçet's disease, vulvovaginitis regularly occurs, and in men - epididymitis. It is noteworthy that all these pathologies are recurrent in nature.
Symptoms of Behçet's disease
Treatment of the syndrome and future prognosis largely depend on the initial manifestations of the clinical picture that worry the patient. After all, as already mentioned, pathology is often accompanied by many other diseases, which, in turn, give certain complications. That is why the patient needs high-quality diagnosis and comprehensive treatment not only of Behçet’s disease itself, but also of accompanying defects.
First of all, it is worth saying that ulcers that appear during illness in the mouth and on the skin are always recurrent. Soon the patient develops the same lesions, but on the mucous membranes of the genital organs. As the defect develops, the ulcers become more extensive; in addition, they can become infected, fill with pus and leave deep scars in their place.
In addition, patients complain of:
- severe visual impairment;
- pain, pain and burning in the eyes;
- the appearance of fog in vision;
- severe migraines.
Many patients also note a sign of morning stiffness in the joints and symmetrical swelling in them. The skin is likely to develop erythema nodosum, acne-like rashes, pustular neoplasms and pseudofolliculitis.
1.General information
Behcet's syndrome is a rare and not yet sufficiently studied disease, which is classified as a group of systemic vasculitis (vascular inflammation). Small and medium-sized arteries are predominantly affected, which, in turn, causes the development of a specific clinical picture (see below).
A number of etiopathogenetic, classification, diagnostic and other issues regarding Behçet's syndrome remain controversial, despite the gradual accumulation of statistical data and research results. Thus, assessments of the influence of the gender factor are contradictory (some sources report a predominance of people of one gender or another among the sick, other authors deny such trends), while a certain regional dependence cannot be explained (indigenous residents of the Mediterranean, Near and Far East get sick hundreds of times more often than residents of, say, North America), opinions differ regarding trigger and etiopathogenetic mechanisms, criteria for differential diagnosis, approaches to treatment, etc.
A must read! Help with treatment and hospitalization!
Other signs
A common symptom of Behçet's disease is undulating fever and weight loss even with adequate nutrition. In the case of ulcerative formations on the mucous membrane of the digestive tract, bloody diarrhea is observed.
Behcet's disease in children, adult women and men proceeds almost identically. The only difference lies in the fact that representatives of the stronger sex in adulthood develop damage to the visual apparatus much faster and thrombophlebitis occurs more often.
Although the full range of signs of pathology is observed, as a rule, after 40 years, already in childhood patients are faced with regular aphthous stomatitis, systematic visual disorders, convulsive attacks, migraines, bowel disorders, and sometimes blood clots after bowel movements.
Men, among other things, may also complain of chronic swelling of the scrotum.
Diagnosis of Behçet's disease
Mandatory and one of the most important criteria for diagnosis is the presence in the patient of recurrent ulcerative lesions of the oral mucosa.
In addition, important symptoms for diagnosing this pathology also include:
- the presence of chronic ulcerations of the mucous membrane of the genital organs;
- complications in the activity of the visual system - keratitis, uveitis, iridocyclitis, iritis, hypopyon, retinal hemorrhages;
- dermatological defects - erythema nodosum, papulopustules, acne-like rashes and pseudofolliculitis.
As for less significant signs, it is worth noting the symptoms of injury to internal systems:
- ulceration of the mucous membrane of the stomach and intestines;
- nonspecific arteritis, pericarditis, myocarditis;
- symptoms of damage to the central nervous system - seizures and aseptic meningitis;
- symmetrical arthritis;
- kidney destruction;
- epididymitis in men.
It is noteworthy that in order to be diagnosed with Behçet's disease, the patient must exhibit all the important symptoms of the disease. If half of these signs are present, it can be considered probable.
Features of detection
A positive pathergy test is considered a highly specific symptom of the disease. It is positive if, 1-2 days after the subcutaneous injection, the patient develops a pustular rash in the injection area.
In addition, when pathology is detected, differential diagnosis with similar ailments is mandatory:
- Crohn's disease, malignant intestinal tumors, ulcerative colitis;
- herpetic stomatitis, genital herpes;
- reactive arthritis and ankylosing spondylitis;
- multiple sclerosis.
When performing diagnostics, the following results are taken into account:
- ultrasound examination of the abdominal organs;
- tests for tumor markers;
- fundus examinations;
- biochemical blood testing;
- immunological blood test;
- irrigoscopy;
- OAM;
- UAC;
- electrocardiograms;
- colonoscopy;
- radiography and ultrasound of joints;
- fibrogastroduodenoscopy.
Histological examination of biopsy specimens of ulcers formed in the patient is mandatory.
Among other things, the victim may be recommended to consult other specialists with a narrow focus: ophthalmologist, cardiologist, neurologist, gastroenterologist, nephrologist and others.
Therapy
It is impossible to completely get rid of this pathology. Behcet's disease is characterized by a chronic course, but complex therapy makes it possible to transfer the defect into remission and constantly monitor the occurrence of exacerbations. In this way, the patient's quality of life can be significantly improved.
Treatment of Behçet's disease involves the use of immunosuppressive and cytostatic medications. These drugs can be combined with glucocorticosteroids and Infliximab.
If severe arthritis is detected, it is advisable to use non-steroidal anti-inflammatory drugs, methotrexate and colchicine.
To eliminate severe damage to the digestive system, glucocorticosteroids, azathioprine, sulfasalazine, and TNF-alpha inhibitors are prescribed.
If there are appropriate indications, the patient may be additionally prescribed antibiotics and antiviral drugs.