Functions of the leg veins
The veins of the legs have a difficult task - without contractility, they must deliver a mass of blood from the most distant parts of the body to the heart.
This is what predetermined the structure of the network, divided into superficial and deep vessels, connected by a network of perforating ducts. Their walls consist of three layers:
- Intima is the inner layer of endothelium, separated from the middle layer by a thin membrane.
- The medial layer is the middle “layer” of the tube, represented by elastic fibers and a small proportion of muscle fibers. It is this layer that gives them strength and stretchability.
- The outer layer, consisting of connective tissue bordering the membrane that separates the blood tubes from the muscle tissue.
Despite the fact that in the lower extremities the drainage network is represented by tubes of different diameters (from 1.5 to 11 mm), the anatomy of the veins is almost the same. The only difference is the thickness of each layer and the number of valves. For example, the veins of the lower leg have more valves, but their diameter is 2 times smaller than that of the great saphenous vein.
In addition to blood pressure, superficial vessels experience significant stress due to external influences, so the thickness of their middle layer is much greater than that of deep-lying tubes. For example, the walls of the great saphenous vein are 1.3 times thicker and stronger than those of the deep vein.
The main functions of the VNK are:
- Ensuring uninterrupted outflow of blood, in which carbon dioxide and waste products of tissues located within their reach are dissolved.
- Delivery to tissues of hormones, organic compounds (enzymes, amino acids, proteins), vitamins and microelements coming from the intestines.
- Regulation of general blood pressure.
It is the variety of tasks assigned to the VNK that has led to close attention to the condition of the blood vessels. Any deviation in their functionality can cause irreparable harm to health.
Arteries
Human arterial system
The arteries of the lower extremities are blood vessels through which blood pumped by the heart is distributed to all organs and parts of the human body, including the lower extremities. Arterial vessels are also represented by arterioles. They have three-layer walls consisting of intima, media and adventitia. They have their own classification characteristics. These vessels have three varieties, which differ from each other in the structure of the middle layer. They are:
- Elastic. The middle layer of these arterial vessels contains elastic fibers that withstand the high blood pressure generated in them when the blood flow is released. They are represented by the aorta and pulmonary trunk.
- Mixed. Here, in the middle layer, different numbers of elastic and myocyte fibers are combined. They are represented by the carotid, subclavian and popliteal arteries.
- Muscular. The middle layer of these arteries consists of individual, circularly located myocyte fibers.
The diagram of arterial vessels according to the location of the internal ones is divided into three types, presented:
- Main, providing blood flow in the lower and upper extremities.
- Organs that supply blood to the internal organs of a person.
- Intraorgan, having their own network, branched throughout all organs.
Deep veins of the lower extremities
Localization of the deep veins of the lower extremities (abbreviated as DVNK) is the thickness of the muscles along the entire length of the legs and thighs. The GVNK include:
- femoral;
- anterior tibial;
- posterior tibial;
- fibula;
- popliteal
The deep ducts are located near the arteries of the same name, and are connected to the superficial ones by a network of perforating vessels. Their walls are highly elastic and resilient. There are numerous valves along the entire length. The thickness of the GVNK ranges from 3 to 10 mm.
In the lower part of the bed, metatarsal vessels flow into the GVNK, from where blood flows through the tibial anterior vein into the popliteal vein. Next, the deep vein of the thigh, which flows into the iliac vessel located in the groin area, is responsible for the drainage of blood. It contains up to 5 valves that support fluid flow in one direction. Part of the blood is “dumped” through a network of perforating tubes into the superficial channels.
The deep-lying network at the level of the lower leg runs virtually parallel to the arterial network, and in the thigh area they are located at a distance from each other.
Net
The artery of the femoral region is located in a lacuna formed from vessels. The external iliac artery is its continuation. It passes under the inguinal ligamentous apparatus, after which it passes into the adductor canal, consisting of a wide medial muscle sheet and a large adductor and membranous membrane located between them. From the adductor canal the arterial vessel exits into the popliteal cavity. The lacuna, consisting of vessels, is separated from its muscular area by the edge of the lata femoral muscular fascia in the form of a sickle. This area contains nerve tissue that provides sensation to the lower limb. At the top is the inguinal ligamentous apparatus. The femoral artery of the lower extremities has branches represented by:
- Superficial epigastric.
- Surface envelope.
- External genitalia.
- Deep femoral.
The deep femoral arterial vessel also has a branching consisting of the lateral and medial arteries and a network of perforating arteries.
The popliteal arterial vessel begins from the adductor canal and ends in a membranous interosseous junction with two openings. In the place where the superior opening is located, the vessel is divided into anterior and posterior arterial sections. Its lower border is represented by the popliteal artery. Further, it branches into five parts, represented by arteries of the following types:
- Upper lateral/middle medial, passing under the knee joint.
- Inferior lateral/middle medial, passing through the knee joint.
- Middle genicular artery.
- Posterior artery of the tibial portion of the lower limb.
Then there are two tibial arterial vessels - posterior and anterior. The posterior one passes in the popliteal-crural area, located between the superficial and deep muscular apparatus of the posterior part of the lower leg (small arteries of the lower leg pass there). Next, it passes next to the medial malleolus, near the flexor digitalis brevis. From it depart arterial vessels that bend around the fibular bone area, a fibular vessel, calcaneal and ankle branches.
The anterior arterial vessel passes close to the muscular system of the ankle. It is continued by the dorsal foot artery. Next, an anastomosis occurs with an arcuate arterial section, from which the dorsal arteries and those responsible for blood flow in the fingers depart. The interdigital spaces are a conductor for the deep arterial vessel, from which the anterior and posterior sections of the recurrent tibial arteries, the medial and lateral ankle-type arteries and muscle branches depart.
Anastomoses that help people maintain balance are represented by the calcaneal and dorsal anastomosis. The first passes between the medial and lateral arteries of the calcaneal area. The second is between the external foot and arcuate arteries. The deep arteries form a vertical type anastomosis.
Deep veins of the legs
The inferior vena cava system originates from the veins of the fingers, the venous arch of the sole and the dorsum of the foot.
- Varicose veins of the lower extremities: stages, causes, symptoms and treatment
From the venous arch of the dorsum of the foot, blood flows into the deep anterior tibial veins (DATIVs).
From the venous arch of the sole, the posterior tibial veins (PTV) and peroneal veins (MPV) are born.
The deep veins of the leg follow with the artery two, rarely four or more; merge before PKV.
PBBV lie in the anterior muscle bed of the leg; through the interosseous membrane they merge into the BBBV.
The internal and external marginal veins of the sole in the calcaneal canal will form two trunks of the BBBV.
ZBBV on n/3 of the leg immediately behind the muscular fascia, then between the flexors and the triceps muscle.
The MBV arises from the posterolateral calcaneus, superiorly between the MBV and the flexor pollicis longus.
On the third third of the leg, the deep veins merge, thus giving rise to the short trunk of the popliteal vein (PCV).
Drainage of the soleus and gastrocnemius muscles into the soleus and gastrocnemius (sural) veins.
- The structure of the human heart and its functions
Close to the joint space of the knee joint, the soleus and gastrocnemius veins merge into the PCV.
The SVC lies posterior to the RCA, from its junction with the thigh, called the superficial femoral vein (SFE).
The SMV from its confluence with the deep femoral vein (DFE) is called the common femoral vein (CFV).
The EIVs collect blood from the lower extremities and continue into the external iliac veins (ELVs).
At L5, the iliac vein and internal iliac vein (Iiliac vein) join to form the common iliac vein (CIV).
At L4, the IVCs drain into the inferior vena cava (IVC); The IVC runs to the right of the aorta and has no valves.
How are the legs supplied with blood?
Depending on the structural features and functions performed, all vessels can be divided into arteries, veins and capillaries.
Arteries are hollow tubular formations that carry blood from the heart to peripheral tissues.
Morphologically they consist of three layers:
- external – loose tissue with feeding vessels and nerves;
- medium, made of muscle cells, as well as elastin and collagen fibers;
- internal (intima), which is represented by endothelium, consisting of squamous epithelial cells, and subendothelium (loose connective tissue).
Transport of oxygenated blood
Depending on the structure of the middle layer, medical instructions distinguish three types of arteries.
Table 1: Classification of arterial vessels:
| Name | Description | Vessels in the body |
| Elastic | The middle layer of such vessels is represented mainly by elastic fibers. They are able to withstand large pressure differences. |
|
| Mixed | The number of elastic and muscle fibers in such vessels is approximately the same. |
|
| Muscular | The middle layer is represented mainly by muscle fibers located along the diameter. |
|
Note! Arteries are also represented by arterioles - small vessels that directly continue into the capillary network.
Veins are hollow tubes that carry blood from organs and tissues to the heart.
They are divided into:
- Muscular - have a myocyte layer. Depending on the degree of its development, there are underdeveloped, moderately developed, and highly developed. The latter are located in the legs.
- Non-muscular - consist of endothelium and loose connective tissue. Found in the musculoskeletal system, somatic organs, and brain.
Vein structure
Arterial and venous vessels have a number of significant differences, presented in the table below.
Table 2: Differences in the structure of arteries and veins:
| Sign | Arteries | Vienna |
| Diameter | Less | More |
| Number of elastic vessels | More | Less |
| Walls | Thicker | Thinner |
| Middle layer | Developed | Not developed |
| Outer layer | Weakly expressed | Strongly expressed |
| Valves | None | Made of venous wall and endothelium. Regulate the movement of blood “from bottom to top” |
The photo shows a schematic representation of the arteriovenous network in the human body.
Arteries of the legs
Blood supply to the legs occurs through the femoral artery. A. femoralis continues the iliac a., which in turn extends from the abdominal aorta. The largest arterial vessel of the lower limb lies in the anterior groove of the thigh, then descends into the popliteal fossa.
Blood supply to the thigh
Note! If there is severe blood loss due to a wound in the lower limb, the femoral artery is pressed against the pubic bone at its exit.
Femoral a. gives several branches represented by:
- superficial epigastric, rising to the anterior wall of the abdomen almost to the navel;
- 2-3 external genitalia, supplying the scrotum and penis in men or the vulva in women; give off 3-4 thin branches called inguinal;
- superficial circumflex, directed to the upper anterior surface of the ilium;
- deep femoral - the largest branch, starting 3-4 cm below the inguinal ligament.
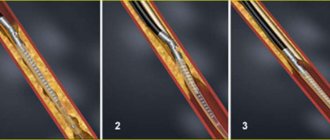
With atherosclerosis, blood circulation is often impaired at level a. femoralis
Note! The deep femoral artery is the main vessel providing O2 access to the tissues of the thigh. A. femoralis, after its departure, goes down and supplies blood to the lower leg and foot.
The popliteal artery begins from the adductor canal.
It has several branches:
- the superior lateral and middle medial branches pass under the knee joint;
- lower lateral – directly in the knee joint;
- middle genicular branch;
- posterior branch of the tibial region.
In the area of the lower leg, popliteal a. continues into two large arterial vessels called tibial (posterior, anterior). Distal from them are the arteries that supply the dorsum and plantar surfaces of the foot.
Blood supply to the leg and foot
Veins of the legs
Veins provide blood flow from the periphery to the heart muscle. They are divided into deep and superficial (subcutaneous).
The deep veins, located in the foot and leg, are double and run next to the arteries. Together they form a single trunk of V. poplitea, located slightly posterior to the popliteal fossa.
The outflow of blood from the NK is carried out through numerous veins
Superficial veins of the lower extremities
Superficial VNK are responsible for draining blood from the toes and metatarsal part of the foot, therefore the localization of the superficial veins of the lower extremities is limited to the foot and ankle. The list of blood vessels located along the upper (front) part of the leg includes:
- dorsal digital vessels;
- dorsal arch of the foot;
- medial marginal tube;
- lateral marginal tube.
On the one hand, the superficial VNCs border with the venules of the toes and feet, and on the other, they connect with the large and small saphenous ducts.
- Why the veins in the hands swell and hurt: causes and treatment
On the underside of the foot, the superficial network is represented by plantar digital ducts flowing into the plantar arch. The vessels then connect to the medial and lateral plantar tubes, which empty into the posterior tibial tube.
The diameter of this group of blood ducts ranges from 1.5 to 3 mm. Due to their short length, they have fewer valves, but the walls are quite dense and elastic due to the large number of reticular and collagen fibers, as well as spirally arranged muscle cells.
Superficial VNK are clearly visible under the thin skin of the feet, which is practically devoid of subcutaneous tissue. They look like bluish tracks, and with heavy stress on the legs they can swell and become bulging.
Peculiarities
Let's look at some of the features of this network:
- Compared to arterial vessels, venous vessels have a larger diameter.
- They have an underdeveloped subendothelial layer and have fewer elastic fibers.
- They have thin walls that fall off easily.
- The middle layer, consisting of smooth muscle elements, is poorly developed.
- The outer layer is quite pronounced.
- They have a valve mechanism created by the venous wall and inner layer. The valve consists of myocyte fibers, and the inner leaflets consist of connective tissue. The outside of the valve is lined with an endothelial layer.
- All venous membranes have vascular vessels.
The balance between venous and arterial blood flow is ensured due to the density of the venous networks, their large number, venous plexuses, and larger sizes compared to arteries.
Vein structure
Their structure has a thinner layer of muscle mass and is less elastic, since the blood pressure in them is several times lower than in the artery.
The veins contain valves that are responsible for the correct direction of blood circulation. Arteries, in turn, do not have valves. This is the main difference between the anatomy of the veins of the lower extremities and the arteries.
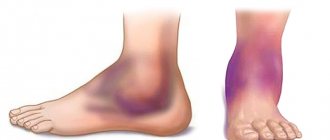
Pathologies may be associated with disruption of the functioning of arteries and veins. The walls of blood vessels are modified, which leads to serious disturbances in blood circulation.
Differences
How does the vascular network differ from the arterial network - these vessels have not only similarities, but also differences, which will be discussed below.
Structure
Arterial vessels are thicker-walled. They contain a large amount of elastin. They have well-developed smooth muscles, that is, if there is no blood in them, they will not fall off. They ensure rapid delivery of oxygen-enriched blood to all organs and limbs, thanks to the good contractility of their walls. The cells included in the wall layers allow blood to circulate through the arteries without obstruction.
They have an internal corrugated surface. They have this structure due to the fact that the vessels must withstand the pressure generated in them due to powerful blood emissions.
Venous pressure is much lower, so their walls are thinner. If there is no blood in them, then the walls collapse. Their muscle fibers have weak contractile activity. The inside of the veins has a smooth surface. Blood flow through them is much slower.
Their thickest layer is considered to be the outer one, in the arteries - the middle one. Veins do not have elastic membranes; in arteries they are represented by internal and external sections.
Form
The arteries have a regular cylindrical shape and a round cross-section. Venous vessels have flattening and a tortuous shape. This is due to the valve system, thanks to which they can contract and expand.
Quantity
There are approximately 2 times fewer arteries in the body than veins. There are several veins for each middle artery.
Valves
Many veins have a valve system that prevents blood flow from flowing in the opposite direction. The valves are always paired and are located across the entire length of the vessels opposite each other. Some veins do not have them. In arteries, the valve system is present only at the exit from the heart muscle.
Blood
Blood flows in veins many times more than in arteries.
Location
Arteries are located deep in the tissues. They reach the skin only in areas where the pulse can be heard. All people have approximately the same pulse zones.
Direction
Blood flows through arteries faster than through veins due to the pressure of the heart. At first the blood flow is accelerated, and then it decreases.
Venous blood flow is represented by the following factors:
- The force of pressure, which depends on the blood impulses coming from the heart and arteries.
- Suction force of the heart during relaxation between contractile movements.
- Suction venous action during breathing.
- Contractile activity of the upper and lower extremities.
Also, the blood supply is located in the so-called venous depot, represented by the portal vein, the walls of the stomach and intestines, the skin and the spleen. This blood will be pushed out of the depot in case of large blood loss or severe physical exertion.
Color
Since arterial blood contains a large number of oxygen molecules, it has a scarlet color. Venous blood is dark because it contains decay elements and carbon dioxide.
During arterial bleeding, the blood flows like a fountain, and during venous bleeding, it flows in a stream. The first poses a serious danger to human life, especially if the arteries of the lower extremities are damaged. The distinctive features of veins and arteries are:
- Transportation of blood and its composition.
- Different wall thicknesses, valve systems and blood flow strength.
- Number and depth of location.
Veins, unlike arterial vessels, are used by doctors to draw blood and inject drugs directly into the bloodstream to treat various ailments.
Knowing the anatomical features and the arrangement of arteries and veins not only in the lower extremities, but throughout the body, you can not only correctly provide first aid for bleeding, but also understand how blood circulates throughout the body.