In medical practice, there are cases when treatment of a seemingly simple disease does not give the desired result. In this case, an experienced doctor may suspect the presence of hereditary pathologies. An example of this is genetic thrombophilia, a pathological condition characterized by increased blood clotting and a tendency to thrombosis and thromboembolism. In this case, observation by a specialized specialist is required, especially for pregnant women.
Appointment with a hemostasiologist, MD. 2,600 rub.
Appointment with a geneticist, doctor of the highest category RUB 3,000.
All prices Make an appointment
If you encounter a similar problem, you should immediately seek medical help. Our International Hemostasis Clinic in Moscow can offer consultation with an experienced geneticist and hemostasiologist, as well as the necessary diagnostics for the presence of hereditary thrombophilia.
Causes of thrombophilia
The main cause of thrombophilia is considered to be a disorder of hemostasis, which provokes a tendency to form blood clots. Repeated thrombosis should lead the patient and his attending physician to suspect the presence of the disease. Thrombophilia is often hereditary. However, it may not manifest itself in any way without appropriate provocateurs. An incorrect lifestyle can lead to thrombophilia even in an initially healthy person.
According to official statistics, thrombophilia is a common disease. Almost half of the adult population suffers from it in one form or another.
Congenital disorders of hemostasis leading to chronic hereditary thrombophilia include gene mutations, protein C and S deficiency, HHC, antiphospholipid syndrome, antithrombin deficiency, and prothrombin abnormalities.
The acquisition of the disease in adulthood is associated with the presence of severe pathologies (for example, cancer), pregnancy, physical inactivity (voluntary or forced), taking certain medications (including oral contraceptives), and chronological aging.
Additional triggers for the development of pathology include:
- Surgical interventions in the locations of the largest venous lines;
- Prolonged immobilization (postoperative, post-traumatic, associated with complications of a number of diseases);
- Obesity (endocrine and nutritional-constitutional)
- Decompensated diabetes mellitus;
- Oncology (undergoing a certain type of chemotherapy);
- Human immunodeficiency virus (HIV);
- Autoimmune diseases;
- Heart failure;
- Atrial fibrillation;
- Heart defects;
- Progressive atherosclerosis;
- Varicose veins of the lower extremities;
- Arterial hypertension of 2-3 degrees, complicated by hypertensive crises;
- Previous heart attacks and strokes;
- Smoking.
Acquired thrombophilia is observed mainly in representatives of the mature and elderly population.
References
- Academician RAMS, prof. IN AND. Krasnopolsky, Doctor of Medical Sciences, Prof. V.A. Petrukhin, Ph.D. A.P. Melnikov: Management of pregnant women with thrombophilia. — Russian Bulletin of Obstetrician-Gynecologist 4, 2013
- R.G. Shmakov, P.A. Kiryushchenkov, A.V. Pyregov, M.A. Vinogradova, O.R. Baev, N.E. Kahn, O.G. Pekarev, N.I. Klimenchenko, N.K. Tetruashvili, V.L. Tyutyunnik, Z.S. Khodzhaeva, N.V. Dolgushina, Brief protocol: Study of the hemostatic system during pregnancy and after childbirth, 2015.
- Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy. American College of Chest Physicians evidence-based clinical practice guidelines 8th edition. American College of Chest Physicians – Medical Specialty Society. 2001 January.
- Tsantes AE, et al. Association between the plasminogen activator inhibitor-1 4G/5G polymorphism and venous thrombosis. A meta-analysis. Thromb Haemost 2007 Jun;97(6):907-13.
Forms and stages of the disease
Experts in the field of phlebology classify the disease into two main categories.
The first category includes thrombophilias provoked by pathological changes in the cellular composition of the blood and its normal rheology. Such violations result from the following processes:
- Blood thickening;
- Change in plasma viscosity;
- Defects in the natural shape of red blood cells.
The listed processes are often caused by exogenous triggers.
The second category is caused by primary disorders of coagulation and hemostasis. It includes congenital pathological conditions caused by a deficiency or excess of coagulation factors.
Thrombophilia can be vascular, hemodynamic and hematogenous.
Folate cycle gene defects and pregnancy
Genes involved in the metabolism of folic acid and vitamin B12 may play a certain role in miscarriage.
Folic acid (vitamin B9) is responsible for the transfer of methyl groups (CH3-) during chemical reactions in the body - these are reactions during which DNA, RNA and a number of amino acids (glycine, methionine) are synthesized. Therefore, it is so important for pregnant women and the fetus not to have a deficiency of both folic acid itself and the enzymes involved in its metabolism.
High concentrations of the active form of folate are required to convert homocysteine to methionine. The main genes whose products control the conversion of folic acid into metabolically active forms and regulate homocysteine metabolism are MTHFR (methylenetetrahydrofolate reductase), MTR (methionine reductase), and MTRR (methionine synthetase reductase). A decrease in the activity of these enzymes is one of the important reasons for the accumulation of homocysteine in the body.
Symptoms and clinical picture
Symptomatically, thrombophilia is expressed in the following manifestations:
- Infarction of internal organs at a young or relatively young age;
- Multiple (recurrent) thrombosis;
- Tendency to pulmonary embolism (PE).
Vascular thrombosis does not always appear immediately. The patient may not suspect that he has a blood clot for a long time until a serious complication occurs.
Complications of thrombosis:
- Ischemic stroke;
- Myocardial infarction;
- Chronic venous insufficiency;
- Pulmonary embolism;
- Necrosis of intestinal tissue and the development of acute peritonitis against its background;
- Gangrene of the lower extremities (subject to appropriate localization of the blood clot);
- Spontaneous abortion (in pregnant women suffering from thrombophilia).
In almost all cases, thrombophilia is discovered accidentally, due to patient complaints of one or more of the listed complications.
When do you need to take the THROMBOPHILIA extended test?
- Cases of hereditary thromboembolism in the family.
- History of thrombosis:
- single thrombosis before 50 years of age;
- repeated thromboses;
- a case of thrombosis at any age with a family history;
- thrombosis of unusual localization (portal, mesenteric, cerebral veins);
- thrombosis of unknown etiology after 50 years.
- High risk situations:
- massive surgical interventions;
- long-term immobilization;
- oncological diseases;
- chemotherapy.
- Ischemic stroke.
- Cardiovascular diseases.
- Prescription of standard antiplatelet therapy.
- Use of hormonal contraception or hormone replacement therapy.
- Planning pregnancy in women with a history of thrombosis, 1st degree relatives with diagnosed hereditary thrombophilia, or a family history of thromboembolic complications.
- Complicated obstetric history.
Diagnostics
Diagnosis of thrombophilia is not difficult for a qualified phlebologist.
It includes the following steps:
- Questioning the patient about current complaints;
- Study of anamnesis (patient medical history);
- Assessment of family history (questioning the patient regarding the tendency to thrombosis in close relatives - mother, father, brothers, sisters);
- Laboratory tests (blood tests for prothrombin time, APTT, coagulation factors, fibrinogen, plasminogen, VWF, D-dimers and other studies at the discretion of the doctor).
The results of the listed examinations are sufficient to make a correct and accurate diagnosis.
Once the diagnosis is established, some hardware manipulation may be required to detect the thrombus. Next, specialists decide on therapeutic tactics. It can be conservative and selected by a phlebologist, or operative (surgical removal of a blood clot) and performed by a vascular surgeon.
Diagram of folic acid metabolism
The reasons for the toxic effect of excess homocysteine on the body of a woman and fetus are as follows (6):
- homocysteine damages the vascular endothelium, which leads to stimulation of thrombus formation. This can lead to placentation disorders and fetoplacental circulation disorders, resulting in infertility and miscarriage;
- elevated levels of homocysteine in late pregnancy can cause placental insufficiency and, as a result, intrauterine growth retardation and chronic fetal hypoxia;
- There was a positive correlation between the level of homocysteine in the blood and the severity of gestosis.
| Gene | Name | Polymorphism: names and [synonyms] | Clinical significance |
| MTHFR | Methylenetetrahydrofolate reductase | C677T; Ala222Val; A222V | The 677T mutant variant of this polymorphism leads to the formation of a heat-labile enzyme and an increase in homocysteine levels in the blood |
| MTHFR | Methylenetetrahydrofolate reductase | A1298C; Glu429Ala; E429A | An increased frequency of the A/C and C/C genotypes for this polymorphism has been reported in women with recurrent early miscarriages. |
| MTR | Methionine reductase | Asp919Gly; A2756G | An increase in the frequency of occurrence of the 66A allele of the MTRR gene and the 2756G allele of the MTR gene was shown in women with a history of premature birth (after the 22nd week of pregnancy). |
| MTRR | Methionine synthetase reductase | Ile22Met; A66G | The MTRR A66C gene polymorphism is associated with Down syndrome and spinal cord defects. |
Treatment of thrombophilia
Complex treatment of thrombophilia is focused on achieving two main goals: prevention of thrombosis and immediate treatment of the provoking pathology. Specialists provide separate treatment for complications, if any are observed.
Thrombophilia therapy includes:
- The use of anticoagulants, thrombolytics and disaggregants;
- Methods of hemocorrection and hydremia;
- Jet blood transfusion (blood transfusion);
- Plasma transfusion;
- Diet therapy;
- Lifestyle correction (especially in the presence of bad habits and physical inactivity);
- Physiotherapy.
Complications are treated and prevented by additional methods. For example, in case of venous insufficiency, it may be necessary to wear a compression device, and in case of intestinal infarction, emergency abdominal surgery may be required to resect the affected areas of the organ.
Thrombophilias in obstetric practice
Currently, thrombophilias are the cause of more than 45% of miscarriage cases, 80% of preeclampsia, often leading to premature placental abruption (PNA), fetal growth restriction syndrome (FGR) with its antenatal death, as well as subsequent and postpartum hemorrhages ( 2, 4)
The connection between thrombophilia and pregnancy pathologies:
F5 - The most significant and common hereditary defect. leading to thrombophilia is the Leiden mutation of factor 5. It is found in 20-40% of patients with venous thrombosis and thromboembolism. Heterozygotes have a 3-7-fold increase in the risk of thrombosis, homozygotes have an 80-100-fold increase. The risk of thrombosis in carriers of the A allele increases sharply during surgical interventions, and in women - when taking oral contraceptives and hormone replacement therapy. During pregnancy, various complications are observed - fetal loss syndrome, preeclampsia, premature placental abruption
F2 - The risk of developing thrombosis in carriers of allele A increases 2-5 times. In pregnant women with this mutation, the risk of not only venous, but also arterial thrombosis increases significantly, which can lead to the development of strokes and coronary artery disease.
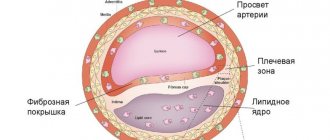
FGB - The mutation is a risk factor for peripheral and coronary thrombosis and is associated with the degree of atherosclerotic vascular damage. During pregnancy, the risk of thrombosis, miscarriage, and thromboembolic complications during childbirth and the postpartum period increases.
F7 - “Wild” allele G is a risk factor for the development of thrombotic disorders and obstetric pathologies (arrest of pregnancy in the early stages, intrauterine growth retardation, fetoplacental insufficiency, fetal development abnormalities, IVF failures). Allele A—reduces the risk of hypertension, atherosclerosis, and pregnancy pathologies.
Genetic predisposition to myocardial infarction, coronary artery disease, coronary atherosclerosis, venous and arterial thrombosis, during pregnancy - late gestosis and fetal growth retardation, phytoplacental insufficiency.
| F5 Leiden mutation (G1691A) | Found in 20-40% of patients with venous thrombosis and thromboembolism. Heterozygotes have a 3-7-fold increase in the risk of thrombosis, homozygotes have an 80-100-fold increase. The risk of thrombosis in carriers of the A allele increases sharply during surgical interventions, and in women - when taking oral contraceptives and hormone replacement therapy. During pregnancy, various complications are observed - fetal loss syndrome, preeclampsia, premature placental abruption |
| F2 Coagulation factor 2 / Prothrombin (G20210A) | The risk of developing thrombosis in carriers of the A allele increases 2-5 times. In pregnant women with this mutation, the risk of not only venous, but also arterial thrombosis increases significantly, which can lead to the development of strokes and coronary artery disease. |
| FGB Firinogen (G-455A) | The mutation is a risk factor for peripheral and coronary thrombosis and is associated with the degree of atherosclerotic vascular damage. During pregnancy, the risk of thrombosis, miscarriage, and thromboembolic complications during childbirth and the postpartum period increases. |
| F7 Coagulation factor 7 (G10976A) | The “wild” allele G is a risk factor for the development of thrombotic disorders and obstetric pathologies (arrest of pregnancy in the early stages, intrauterine growth retardation, fetoplacental insufficiency, fetal development abnormalities, IVF failures). Allele A—reduces risk of hypertension, atherosclerosis, and pregnancy pathologies. |
| SERPINE 1 Plasminogen activator inhibitor type 1 (5G>4G) | The presence of the 4G allele increases the risk of myocardial infarction and a high incidence of venous and arterial thrombosis. Complications of pregnancy - early preembryonic and embryonic losses, gestosis and IVF failures. |
| Mutations in platelet factor genes | Genetic predisposition to myocardial infarction, coronary heart disease, coronary atherosclerosis, venous and arterial thrombosis, during pregnancy - late gestosis and fetal growth retardation, phytoplacental insufficiency. |
| MTHFR 5,10-methylenetetrahydrofolate reductase (C677T) | Allele T—hyperhomocysteinemia. Venous and arterial thrombosis. Homozygotes for T - preeclampsia, premature abruption of a normally located placenta, intrauterine growth retardation, fetal loss syndrome, increased risk of development during pregnancy and the development of neural tube defects. |
Prevention
It is important for individuals diagnosed with thrombophilia to understand the consequences they may face if treatment and prevention are ignored.
Timely diagnosis of thrombophilia is extremely important when making a prognosis. The sooner you contact a specialist for help in eliminating characteristic complaints, the higher your chances of avoiding all known complications of the disease.
It is important for patients at risk to be examined routinely. This is especially true for smokers, people with chronic provoking diseases, people undergoing aggressive therapy (for example, antitumor), pregnant women, girls taking oral contraceptives.
Prevention of thrombosis in thrombophilia involves:
- Refusal of excessive physical activity (professional sports);
- Systematic use of compression hosiery;
- Avoiding injuries and impacts;
- Drink plenty of fluids;
- Taking medications prescribed by a phlebologist according to the specified course and schedule.
In severe forms of thrombophilia, treatment and prevention often become lifelong.
We strongly recommend that you contact competent specialists in the field of phlebology and vascular surgery if you suspect a disease. Do not attempt self-medication and do not use “traditional methods,” at least without prior consultation with a specialist.
Thrombophilia - what kind of disease is it?
Thrombosis is the process of forming blood clots where the vascular wall is damaged; its purpose is to ensure the safety of the vascular system.
This process itself is physiologically normal; it prevents excessive blood loss at the sites of injury. But if the thrombotic process is excessive, then pathological thrombosis occurs. When answering the question of what thrombophilia is, we can give a clear example in the form of a photo that shows increased activity of blood cells and the formation of a blood clot. The disease is not always accompanied by thromboembolism or thrombosis, but the risk of blood clots in various places of the circulatory system greatly increases. Now modern medicine is concerned about the problem of this disease, since deaths quite often occur due to blockage of a blood vessel. The most commonly diagnosed hereditary thrombophilia is hereditary thrombophilia. According to statistics, in Europe about 15% of people suffer from this disease.
Do not confuse concepts such as thrombophilia and trypophilia. These are completely unrelated terms. But sometimes you can hear the question: trypophilia, what is it? The concept means phobia, fear of accumulation of objects with a rounded shape, cluster holes. So tripophilia is fear and discomfort associated, for example, with lotus seeds, honeycombs, and not a disease that manifests itself as pathologies in the body.
What are blood clots and why do they appear?
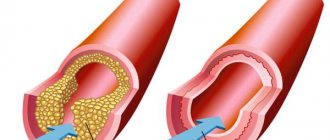
Thrombi are clots that form from connections between blood cells. Platelets, sticking together in chains, form lumps that are attached to the walls of blood vessels. In some situations, blood clots form due to disorders of the hematopoietic system, in others - as a result of damage to the inner wall of the vessel.
Large growths inside the vein prevent blood flow from passing through the obstructed area. As a result, congestion forms in the veins, leading to varicose veins. When a blood clot blocks the lumen, a heart attack occurs—the death of tissue that has not received oxygen through the bloodstream.
The formation of blood clots is influenced by several factors from a person’s daily life:
- Sedentary lifestyle. Lack of active mobility leads to stagnation of blood in the lower legs. Therefore, constantly sitting at a computer, as well as choosing an escalator instead of stairs, give the blood a reason to stagnate and form clots.
- Insufficient fluid intake. The quality of blood directly depends on what a person eats. With insufficient fluid intake, the blood becomes thick, which means it cannot fully perform its functions and puts a greater strain on the heart. It is easy to pump liquid blood through the system, but thick blood is much more difficult.
- Taking medications that affect the hematopoietic system. In medical practice, drugs are often used to treat certain diseases, one of the side effects of which is blood thickening. Therefore, such medications must be taken simultaneously with anticoagulants that prevent the formation of blood clots.
You can protect yourself from blood clots by regularly exposing your body to physical activity, drinking enough fluids, and including more plant-based foods rich in fiber in your diet.
Thrombosis factors
An increased risk of blood clots is caused by:
- Genetic inheritance to predisposition.
- Diseases that force you to limit physical activity, for example, bed rest.
- High degree of blood clotting.
- Arrhythmia, cardiomyopathy and other diseases that disrupt the strength and rhythm of blood flow throughout the system.
- Varicose veins.
- Liver dysfunction.
- Alcoholism.
- Smoking.
- High body mass index.
- Age-related changes in hormone levels in both men and women.
Some of these factors cannot be influenced, for example, genetic predisposition. However, you can protect yourself from the serious consequences of blood clots by maintaining an active and healthy lifestyle.