For many patients with varicose veins, surgery to remove veins is scary: if the veins are removed or ligated, how will blood circulate in the vessels of the legs? In fact, only a tenth of the blood circulates through the veins located under the skin - the same ones that form unaesthetic varicose veins. Removing superficial veins does not create noticeable additional stress on the deep veins.
Recovery after surgery to remove varicose veins on the legs should be comprehensive, its goal is to prevent complications of the disease, relapses, and return the patient to work and usual activities as soon as possible. The measures that form the recovery program after surgery depend on the degree of neglect of the disease, the nature of the operation, as well as the general condition of the patient and the characteristics of his body.
What operations are performed for varicose veins in the legs?
There are three main types of operations for varicose veins of the lower extremities: classic venectomy (phlebectomy), stripping and vein ligation.
Classical venectomy (phlebectomy). During this intervention, a longitudinal skin incision is made on the leg, corresponding to the course of the varicose vein. The vessel is isolated, ligated in the area of the ankle and knee (if we are talking about the lower leg) or the knee and groin (if a vein on the thigh is removed), large branches of the vein are ligated and it is cut off, after which the incision is sutured. Phlebectomy is an outdated technology that is practically not used these days, as it has been replaced by new, less traumatic and more effective methods of surgery.
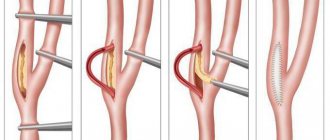
Stripping. A more advanced and modern modification of phlebectomy and less traumatic than the classic operation. The essence of the intervention is that small punctures are made in the area of the ankle and knee (or knee and groin), the vein is isolated, ligated, a special flexible wire probe is inserted into its lumen and with its help the vein is “pulled out” from under the skin. Scarring after such an intervention is minimal.
Vein ligation. With this intervention, the varicose vein is not completely removed, it is only tied at the base of the varicose nodes, due to which blood circulation in the vessel stops and the nodes collapse.
This type of intervention is considered ineffective for large veins, but for small-diameter vessels it is more appropriate than their complete removal. Also, vein ligation makes sense if the vessel is naturally very tortuous, has sharp bends or sharp narrowings, which makes it impossible to pass the probe along the entire length of the vein.
Contraindications
Despite the large number of advantages and indications for use, phlebectomy has some limitations. These include:
- Acute viral or infectious diseases. Such conditions increase the possibility of developing postoperative complications in the form of sepsis.
- Severe hypertension, uncontrolled by medications.
- Chronic heart failure in the stage of decompensation.
- Pregnancy period. An absolute contraindication is the second half of gestation. This is due to the fact that any intervention can provoke the development of spontaneous abortion.
- The presence of inflammatory diseases in the lower extremities. These conditions can trigger the spread of inflammation to other organs and tissues.
- Age over 65 years. With age, surgical interventions are more difficult to tolerate. This is due to the presence of a sufficient number of concomitant pathologies. Phlebectomy of veins can lead to exacerbation of chronic diseases, which will negatively affect the course of the recovery period.
Some of the listed contraindications are temporary. This means that after removing the restrictions, the surgical intervention can be carried out in full. Depending on the severity of the condition and the type of affected vessel, the doctor selects a phlebectomy technique that will be most effective in each specific case.
What may be the consequences after vein removal?
Surgeries to remove varicose veins are quite traumatic interventions that seriously disrupt the internal balance of the body. Therefore, you need to be prepared for certain discomfort in the postoperative period: pain in the intervention area; hematomas at the site of the removed vein and at the sites of sutures on the skin; swelling of the leg at the site of the removed vein and sutures; moderate bleeding of the postoperative wound; general weakness, fever, nausea.
Why do such consequences occur? After removal of veins in the legs, an inflammatory process inevitably occurs in the tissues that previously surrounded the vessel - this is a natural, physiological reaction of the body to the intervention, aimed at healing the damage. Any inflammatory process is accompanied by local swelling and pain, and general symptoms of malaise are possible: nausea, fever, weakness. They disappear a few days after the intervention. Minor bleeding from a postoperative wound should not be a concern either: when a vein is removed, small vessels break off, which then collapse and the flow of blood stops. If you follow the surgeon’s recommendations, the unpleasant phenomena will quickly disappear.
In some cases, after venectomy surgery on the legs, infection of the intervention area, suppuration, thromboembolism, or accumulation of blood in the ligated vein with the development of inflammation of the vessel is possible. But thanks to modern surgical capabilities and the perfection of surgical technology, such complications are extremely rare.
Get an online consultation
right now.
Get
Preoperative preparation
The operation is preceded by a face-to-face consultation with a vascular surgeon – phlebologist. After collecting an anamnesis and conducting an examination, an ultrasound duplex scanning of the veins is performed, after which indications and contraindications for treatment are determined. Preoperative preparation includes standard tests, an electrocardiogram, chest x-ray, as well as consultation with a therapist to obtain permission for surgical treatment if the patient has serious concomitant diseases.
How to spend the postoperative period
The postoperative period after phlebectomy on the legs lasts ten days: from the moment of the operation itself until the sutures are completely removed. At this time, the operated limb needs special attention and special care.
After the operation, the patient receives compression of the lower extremities using compression stockings. Compression is an important condition for the smooth course of the postoperative period, as it allows you to compress the saphenous veins, preventing stagnation of blood in them, and, accordingly, the formation of blood clots. Compression also accelerates the healing of small veins remaining after removal of the main venous trunk.
Places where stitches are placed should not be wet. For hygienic purposes in the postoperative period, wet wipes or gauze moistened with water are used. The sutures are regularly treated with iodine and a sterile bandage or sticker is applied to protect them from damage and contamination.
To reduce swelling of the lower extremities, it is recommended to keep them elevated - on a pillow, a fabric cushion up to 15 cm high. In case of intense pain after surgery, the doctor may prescribe painkillers, and antibiotics to prevent purulent complications.
What activities are recommended during the rehabilitation period?
The rehabilitation period begins immediately after the end of the postoperative period, that is, 10 days after the operation. At this point, the sutures have already been removed, the postoperative punctures, if there are no complications, have healed. But the body’s recovery processes continue. In order for recovery to occur as quickly as possible, the doctor adjusts the patient’s lifestyle. During the rehabilitation period it is necessary:
- taking medications prescribed by a phlebologist;
- reasonable physical activity, exercise therapy;
- limb compression;
- work in gentle conditions, limiting heavy physical labor;
- nutrition correction;
- physiotherapy, massage.
Drug therapy in the postoperative period involves taking drugs that increase the tone of the venous walls, improve the rheological properties (fluidity) of blood, and have an anti-edematous effect. The drugs recommended during the rehabilitation period include products based on troxerutin, diosmin, drugs with vitamins C and PP, extracts of ginkgo biloba, and horse chestnut. Preparations of salicylic acid, hirudin, and heparin are used as anticoagulants.
Medicines are prescribed both in the form of general preparations (tablets, capsules for oral administration) and local preparations (gels, ointments for application directly to the skin of the lower extremities). Competent drug therapy during the rehabilitation period can accelerate the restoration of microcirculation and at the same time serves as an effective prevention of relapses of the disease.
Moderate physical activity is necessary to stimulate blood circulation in the lower extremities, prevent its stagnation, and the formation of blood clots. Walking at a moderate pace, swimming, and exercise therapy complexes are recommended as optimal measures to activate the patient. Running during the rehabilitation period is not recommended.
During the rehabilitation period, compression on the legs is mandatory. Compression of the lower extremities is necessary for all patients suffering from varicose veins - it helps prevent the progression of the disease and the development of complications. A phlebologist recommends a compression method and selects the size of elastic underwear.
Gentle working conditions are necessary to prevent relapse of the pathology and its transfer to the deep veins of the legs. Varicose veins are often a consequence of difficult working conditions and the characteristics of professional activity. If your job involves standing for a long time, it may be worth changing it or at least regularly performing therapeutic exercises during the working day aimed at improving blood circulation in the legs. Work in conditions of high temperatures associated with vibration and heavy lifting is contraindicated.
Correction of nutrition after leg vein removal surgery should be directed towards rationalization. Food needs to be complete, healthy, rich in protein, fiber, vitamins and microelements. If you are overweight, you should reduce your caloric intake, since obesity is one of the factors in the progression of varicose veins.
Physiotherapeutic techniques during the rehabilitation period accelerate recovery. A physiotherapeutic treatment program is recommended by a doctor; wraps, electrophoresis, UHF, and magnetic therapy may be useful. Massage during the rehabilitation period helps to effectively eliminate swelling.
Competent management of the postoperative period after removal of dilated veins in the legs, a responsible attitude to the doctor’s recommendations will help eliminate the natural discomfort that occurs after surgery as soon as possible, prevent possible complications and speed up the patient’s return to a full life.
What do patients think about new treatments for varicose veins?
Until now, despite the widespread use of laser and other endovenous thermoobliteration techniques, doctors in most specialties (especially open surgeons) have a prejudice against this procedure. These misconceptions lead to misinformation of the patient who consulted such a doctor, as a result of which this skepticism is transferred to the patient, who is sent instead of a low-traumatic and cosmetic laser procedure to open surgery under anesthesia.
Most often, these misconceptions come from the lack of personal experience working with laser equipment (most information is obtained from “third”, equally incompetent persons), as well as the lack of actual patients treated with laser equipment and observation of them. That is, all the problems come from the lack of simple educational literature, although there are a huge number of scientific articles on the Internet (mainly in the foreign press) on this issue. Let's take a closer look at why this happens, namely the main misconceptions of doctors.