Cardiac cycle - systole and diastole
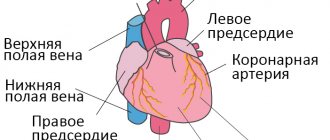
Alternate contraction and relaxation of cardiomyocytes ensures synchronous functioning of the entire heart. The cardiac cycle consists of:
- pauses – general relaxation (diastole) of all parts of the myocardium, atrioventricular valves are open, blood passes into the cavities of the heart;
- atrial systole - movement of blood into the ventricles;
- contractions of the ventricles - release of the great vessels.
Atrial
The impulse for myocardial contraction occurs in the sinus node. After the vascular openings are blocked, the atrial cavity becomes closed. At the moment the entire muscle layer is covered by excitation, the fibers are compressed and blood is pushed into the ventricles. The valve flaps open under pressure. The atria then relax.
Normally, the atrial contribution to the total filling of the ventricles is insignificant, since they are already 80% filled during the pause period. But with an increase in the frequency of contractions (flickering, fluttering, fibrillation, supraventricular form of tachycardia), their role in filling increases significantly.
We recommend reading the article on systolic and diastolic pressure. From it you will learn about the norm in indicators between systolic and diastolic pressure, what affects the indicators and how to normalize the values. And here is more information about functional extrasytols.
Zheludochkov
The first period of contractions is called myocardial tension. It lasts until the valve flaps of large vessels leaving the ventricles open. Consists of 2 parts: non-simultaneous contraction (asynchronous) and isometric. The latter means the involvement of all myocardial cells in the work. The blood flow closes the atrial valves, and the ventricle is completely closed on all sides.
The second stage (expulsion) begins with the opening of the valve flaps of the pulmonary trunk and aorta. It also has two periods - fast and slow. At the end of cardiac output, pressure increases in the vascular network, and when it becomes equal to cardiac pressure, systole stops and diastole begins.
Diastole
A Wiggers diagram showing various events during diastole. During early ventricular diastole -
see the vertical bar labeled “Isovolumetric Relaxation”—the pressure in each ventricle (blue curve) begins to fall rapidly from the wave height reached during systole.
When ventricular pressure drops below the atrial chambers, the atrioventricular (mitral and tricuspid) valves open, causing the volume of blood (red trace) in the atria to flow into the ventricles. + In late ventricular diastole,
the two atrial chambers begin to contract (atrial systole), causing an increase in blood pressure in both atria and forcing additional blood volume into the ventricles. This onset of atrial systole is known as the atrial kick—see the Ventricular Volume graph (red) just above the P wave on the electrocardiogram graph (dark blue).
For a healthy human heart, the entire cardiac cycle usually lasts less than one second. That is, for a typical heart rate of 75 beats per minute (beats per minute), the cycle requires 0.3 seconds of ventricular systole (contraction) - pumping blood to all body systems from the two ventricles; and 0.5 seconds in diastole (dilatation), refilling the four chambers of the heart, for a total of 0.8 seconds to complete the cycle. [2]
Early ventricular diastole
During early ventricular diastole, the pressure in the two ventricles begins to fall from the peak reached during systole. When the pressure in the left ventricle falls below that in the left atrium, the mitral valve opens due to a negative pressure difference (suction) between the two chambers, causing blood in the atrium (accumulated during atrial diastole) to flow into the ventricle (see figure above ). Likewise, the same phenomenon occurs simultaneously in the right ventricle and right atrium through the tricuspid valve.
Ventricular filling flow (or flow from the atria to the ventricles) has an early (E) diastolic component caused by ventricular suction, followed by a late component produced by atrial systole (A). The E/A ratio is used as a diagnostic measure because its decrease indicates possible diastolic dysfunction. [3]
Late ventricular diastole
Early diastole is the mechanism of suction between the atrial and ventricular chambers. [4] Then, during late ventricular diastole, the two atrial chambers contract (atrial systole), causing an increase in blood pressure in both atria and forcing additional blood flow into the ventricles. This onset of atrial systole is known as the atrial impulse -
see Wiggers diagram.
The atrial impulse does not
provide a greater volume of blood flow (during the cardiac cycle), since about 80 percent of the collected blood volume enters the ventricles during the period of active absorption. [5]
Atrial diastole
At the beginning of the cardiac cycle, all four chambers of the heart, two atria and two ventricles synchronously approach relaxation and expansion, or diastole. The atria fill with separate volumes of blood returning to the right atrium (from the vena cava) and to the left atrium (from the lungs). Once chamber pressure and back pressure are equalized, the mitral and tricuspid valves open and returning blood flows through the atria into the ventricles. When the ventricles are completely filled, the atria begin to contract (atrial systole), forcing blood under pressure into the ventricles. The ventricles now begin to contract, and as the pressure inside the ventricles increases, the mitral and tricuspid valves close.
As the pressure inside the ventricles continues to rise, they exceed the "back pressure" in the aortic trunk
and pulmonary arteries
of the trunk
. The aortic and pulmonary valves open and blood is pumped out of the heart. The expulsion causes the pressure in the ventricles to drop, and at the same time the atria begin to fill (atrial diastole). Finally, the pressure inside the ventricles drops below the back pressure in the aortic trunks and pulmonary arteries, and the aortic and pulmonary valves close. The ventricles begin to relax, the mitral and tricuspid valves begin to open, and the cycle begins again. [6]
Thus, when the ventricles are in systole and contracting, the atria are relaxed and collect returning blood. When the ventricles become fully dilated in late diastole (referred to as LVEDV and RVEDV in the images), the atria begin to contract, pumping blood into the ventricles. The atria provide a constant flow of blood to the ventricles, thereby serving as a reservoir for the ventricles and ensuring that these pumps never run dry. [7] This coordination ensures that blood is pumped and circulated efficiently throughout the body. [8]
Difference between systole and diastole
For the heart muscle, relaxation is no less important than contraction. By apt definition, diastole makes systole. This period is just as active. During this time, actin and myosin filaments diverge in the cardiac muscle, which, according to the Frank-Starling law, determines the force of cardiac output - the greater the stretch, the greater the contraction.
The ability to relax depends on the fitness of the heart muscle; in athletes, due to prolonged diastole, the contraction frequency is reduced, and blood flow through the coronary vessels increases at this time. There are two phases during the relaxation period:
- protodiastolic (the reverse movement of blood closes the valve flaps of blood vessels);
- isometric – straightening of the ventricles.
This is followed by filling, and then atrial systole begins. Upon completion, the ventricular cavities are ready for subsequent contraction.
What does diastole and systole show?
Diastolic pressure refers to the lower limits of blood pressure, showing the level of blood pressure when the heart muscle is relaxed, the resistance force of blood vessels located on the periphery.
In a normal state, diastole is 80 mmHg. A drop in this figure occurs as a consequence of the reducing effect during the passage of blood flow through the venous, arterial, and capillary lines.
Systolic pressure is the maximum indicator of blood pressure, recorded when the heart contracts and sends blood flow through the vessels. Systole is the upper value, which in a healthy body (without cardiovascular pathologies) is equal to 120 mmHg.
In a person without hidden or obvious diseases, systolic blood pressure changes under the influence of individual triggers:
- strength of heart contractions;
- the level of elasticity of veins, arteries and capillaries, their tone;
- physical activity;
- stress, emotional turmoil.
An increase in systole indicates hidden or obvious pathological processes in the heart and blood vessels. Deviations require a full laboratory diagnostic examination and a competent approach to subsequent therapy.
Time of systole, diastole, pause
If the heart rate is normal, then the approximate duration of the entire cycle is 800 milliseconds. Of these, individual stages account for (ms):
- atrial contraction 100, relaxation 700;
- ventricular systole 330 – asynchronous tension 50, isometric 30, ejection 250;
- Ventricular diastole 470 – relaxation 120, filling 350.
Expert opinion
Alena Ariko
Expert in Cardiology
That is, for most of the life (470 to 330) the heart is in a state of active rest. In response to stress, the frequency of contractions increases precisely due to a decrease in relaxation time. An accelerated pulse is considered one of the risk factors for diseases of the circulatory system, since the myocardium does not have time to recover and accumulate energy for the next beat, which leads to a weakening of the heart.
Concept of pressure, resistance and heart rate
Take a rubber bulb in your palm and fill it with water. Now squeeze it as hard as you can, trying not to leave a single drop inside. The water will pour out of the outlet, and the larger it is, the less effort you need to make. And vice versa. The narrower the hole, the more difficult it is to squeeze everything out of the pear cavity without leaving a trace. Now we’ll do the same thing, but let’s try to put two rubber bulbs together. Let's fill them with the same volume of water, but in one we will make a large hole for exit, and in the other - a small one. From the first, when compressed, water will pour out easily, with a slight squeeze, but to empty the second, much more force will be required. This is what happens with the heart. With one important exception: there is no one to squeeze him, and his own muscular system does all the work.
Contracting, or “contracting,” in the systole phase, it pushes out of its ventricles all the blood coming from the atria, and in the diastole phase
– rests, gaining strength for the next contraction, which will follow in a split second.
The force with which the heart muscle compresses this volume of blood in the cavity of the ventricles creates pressure, as a result of which the blood is thrown into the great vessels. But the speed with which it leaves the ventricles will depend not only on the force of compression, but also on how difficult or easy it is for it to leave the ventricle and enter the lumen of the vessel. That is, if we return to our two rubber bulbs: it will go through the larger hole, or through the smaller one. In other words, what is also important is what kind of resistance will be provided to this release from the side, so to speak, that receives it, i.e. vascular bed. Here we have come to understand several main laws that govern both the movement of blood in the heart and its movement in the body, i.e. to what forces and along what currents our kayak moved.
So, a few new concepts: blood volume, pressure and resistance to blood flow.
The simplest and long-known most important parameter that can be measured and expressed in numbers is pressure. But what is pressure? Believe me, if you want to understand what’s wrong with your child, you need to know this clearly. Only then will you be able to understand what the doctors will tell you. It's actually very simple.
Blood pressure is a number that speaks about two important aspects of blood movement: its volume and resistance to its flow in each individual period of time. It can be measured in any vessel, in any chamber of the heart. And it gives a fairly accurate idea of what is happening there, inside the chamber, at each phase of the cardiac cycle.
For now we are only talking about the work of a healthy heart. And it is clear that the greater the volume of blood in the ventricle, the greater the effort required to eject it, i.e. put him under more pressure. And - the greater the resistance to ejection, the greater the effort (pressure) needed to empty the ventricle, preparing it for a new portion of blood.
The vascular bed resists blood flow as a whole, from the beginning, i.e. from the ascending aorta, to the smallest arteries and capillaries - in the large circle, and the pulmonary arteries, arterioles and capillaries - in the small circle. Consequently, the powerful left arterial ventricle works against the resistance of the gigantic vascular bed of the entire body. The right ventricle, venous, thinner-walled, works against the same gigantic volume, but much more elastic, short and “soft” vascular bed of the lungs. Accordingly, the pressure figures in the cavities of the ventricles are different, and in the vessels extending from them. These figures are reflected in Table No. 1, and you can see that the pressure under normal conditions in the right ventricle and pulmonary artery is approximately one third of the pressure in the left ventricle and vessels of the systemic circle. Remember that quantity, i.e. The volume of blood ejected from each ventricle with each contraction is normally the same. So far we have only talked about the compression of blood volume under pressure. This is the so-called systolic pressure, or the maximum pressure created in the system at the moment of contraction.
But there is a second number - this is the blood pressure in the vessels during diastole, or a relaxed and filling heart. In this phase, the valves of the aorta and pulmonary artery are closed and, with their integrity, the blood in the vessels is under pressure from the closed system of the vascular bed of the body (in the large circle) and the lungs (in the small circle). Therefore, there are two numbers of pressure - the so-called “upper” (systolic) and “lower” (diastolic) pressure.
Average numbers of normal pressure in the cavities of the heart and large vessels (mm Hg)
| Newborns | Children (1 month – teenagers) | |
| Right atrium | 0 — 3 | 2 — 5 |
| Right ventricle | 35 – 65 | 15 -30 / 2 – 5 |
| Pulmonary artery | 35 – 65 / 20 – 40 | 15 – 30 / 5 – 10 |
| Left atrium | 1 — 4 | 5 – 15 |
| Left ventricle | 70 – 90 | 80 – 130 / 5 – 10 |
| Artery | 80 – 100 / 50- 60 | 90 – 130 / 60 — 90 |
Please note that in newborns the pressure in the right ventricle and pulmonary artery is significantly higher than in children even in the first month of life. This is explained by the fact that the vessels and all 700 million alveoli of the lungs open gradually and are fully ready to receive the entire volume of blood from the right ventricle only a few weeks after birth.
Now let's try to answer the question - what moves the heart, what causes its rhythmic contractions. Believe me, this is also very important.
The rhythmic, sequential, regular cycle of contraction and relaxation of the heart is controlled by electrical impulses. These impulses arise in special cells of the heart muscle, the so-called cells of the conduction system. Foci of large accumulations of these cells are called “nodes”, and their branches running along the muscle fibers are called “conducting paths”. There are two nodes of the conduction system: sinus and atrioventricular, and there are several pathways. The peculiarity of the cells themselves that conduct electrical impulses is that they are capable of being excited and transmitting this excitation much faster than neighboring cells of the working, contracting myocardium, or cardiac muscle. Therefore, they are guides, showing the way to others, understanding faster than others where to go. In a normal heart, the superior sinus node is excited first. The impulse is transmitted along the conductive pathways of the walls of the atria to the lower, atrioventricular node, and then, through thinner pathways, it enters the ventricles, causing their contraction in response - the systole phase. This is followed by a pause period - diastole - and the myocardium prepares to receive a new impulse. The frequency of such impulses is the frequency of the heartbeat and pulse. In newborns - 110-120 beats per minute, in adults much less often - 65-75 beats per minute. These electrical impulses are easily recorded by fairly simple instruments. The recording of the devices is called an electrocardiogram.
We are far from thinking of teaching you how to read it: this is a matter for professionals. We just want to explain what it is and why it is done. An electrocardiogram makes it possible not only to identify disturbances in the normal conduction of impulses, but also to determine which parts of the heart are abnormally enlarged, which are constantly working with increased load, and how they cope with it. If a heart defect is suspected, your child will have this test done many times. It is painless and very informative.
We can only marvel at the incredible perfection of the cardiovascular system, which, despite all its complexity, is surprisingly simple, logical and harmonious. However, it must be absolutely accurately and correctly created. Even small changes in its structure are enough to disrupt this constant, calm and synchronous work.
Quoted from the book by G. E. Falkovsky, S. M. Krupyanko. The heart of a child. A book for parents about congenital heart defects
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
What determine the phases of systole and diastole?
The factors that determine the distensibility and subsequent contractility of the myocardium include:
- wall elasticity;
- thickness of the heart muscle, its structure (scar changes, inflammation, dystrophy due to malnutrition);
- cavity size;
- structure and patency of valves, aorta, pulmonary artery;
- activity of the sinus node and the speed of propagation of the excitation wave;
- condition of the pericardial sac;
- blood viscosity.
Watch the video about the cardiac cycle:
Diastolic dysfunction
Disturbance in the diastolic phase can cause several problems. Inadequate filling of the left ventricle leads to a decrease in the amount of blood that is pumped from the heart to oxygenate various parts of the body. Additionally, if the ventricle does not fill properly with blood, blood is drawn back into the atrium and then into the lungs, increasing the pressure gradient of the blood in the pulmonary vessels. This inappropriate pressure gradient causes fluid or transudate to leak from these vessels into the alveoli of the lungs, causing pulmonary edema.
Symptoms and treatment of diastolic dysfunction
Diastolic dysfunction can cause symptoms for many months or even years, and the slow progression of the disease means that many people survive the disease without requiring any specific treatment.
In cases of conditions that predispose to diastolic dysfunction, the underlying disease should be treated. For example, high blood pressure and diabetes should be treated appropriately.
Atrial fibrillation is another condition that requires immediate treatment, as inadequate pumping of blood through the atria into the ventricles can also lead to diastolic dysfunction. If atrial fibrillation causes your heart to beat faster, medications may be given to slow the heart rate.
Atrial fibrillation
Reasons for violation of indicators
Violation of myocardial contractility and weakening of systole cause ischemic and dystrophic processes - angina pectoris, cardiosclerosis, amyloidosis, myocardial dystrophy, myocarditis. Due to narrowing of the valve openings or difficulty in ejecting blood from the ventricles, the amount of residual blood in their cavities increases, and a reduced volume enters the vascular network.
Such changes are characteristic of congenital and acquired heart defects, hypertrophic cardiomyopathy, and narrowing of the great vessels.
Violation of the formation of an impulse or its movement through the conduction system changes the sequence of myocardial excitation, the synchrony of systole and diastole of parts of the heart, and reduces cardiac output. Arrhythmias change the duration of the phases of the cardiac cycle, the efficiency of ventricular contractions and the possibility of their complete relaxation.
Diseases that are accompanied by diastolic and then systolic dysfunction also include:
- pericarditis;
- bacterial endocarditis;
- arterial and pulmonary hypertension;
- hypotension;
- systemic autoimmune pathologies;
- disorders of endocrine regulation - diseases of the thyroid gland, pituitary gland, adrenal glands;
- vegetative-vascular dystonia is an imbalance between parts of the autonomic nervous system.
Diastolic heart failure and vascular stiffness
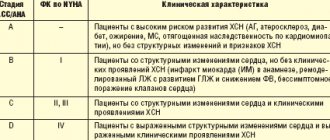
Academician Ivashkin V.T.: – I ask Oksana Mikhailovna to make another message. "Diastolic heart failure and vascular stiffness." Please. Professor Drapkina O.M.: – Thank you very much. Dear colleagues, today I talked about myocardial fibrosis, and, in principle, when talking about myocardial fibrosis, one way or another you are talking about diastolic heart failure. We at the clinic and at the department are dealing with this problem, accordingly, now there are also certain opportunities to share the experience that we have accumulated.
We are talking about diastolic heart failure, we are talking about arterial hypertension and we say that, after all, impaired diastole is the fate of patients with a high risk of arterial hypertension. But when the risk of arterial hypertension according to SCORE is high, we know that this is severe target organ damage and more than three risk factors or, for example, metabolic syndrome, when there are other risk factors (Sergei Rudzherovich spoke today, and we together recalled the Jupiter study ", where the marker in healthy people was an increase in high-sensitivity C-reactive protein).
So the question arises. We say all the time: “Patients come to us with myocardial infarction because we treated arterial hypertension incorrectly.” What if we treated arterial hypertension correctly? Then you get myocardial hypertrophy and, accordingly, an increase in rigidity. So what happens that chronic heart failure with preserved ejection fraction is the correct treatment for arterial hypertension and that there is no other way?
Of course this is not true. But nevertheless, with this slide I would like to draw attention to this postulate: delaying myocardial infarction in a patient with arterial hypertension is not our only task. The range of our tasks is much larger, including preventing this stage, when the patient moves from simply being hypertensive to being hypertensive with chronic heart failure, usually with preserved ejection fraction.
Therefore, once again a few words about terminology. We will talk about heart failure with preserved ejection fraction. In principle, this is the correct term, but we, the medical community, allow each other to call this heart failure diastolic heart failure - probably just for shorthand.
The epidemiology is known. There are slightly different data – European and ours. According to the EPOCHA study, more than 70% of patients with heart failure have preserved ejection fraction. Of course, this is the lot of the elderly, since we are all fighting for the fact that our population is getting older, we are all fighting for life expectancy. This will lead to the fact that there will also be more patients with diastolic heart failure, and we will need to manage them somehow for many years.
Here, in my opinion, is interesting data. The annual mortality rate of patients with diastolic heart failure is indeed somewhat lower. But when we looked at mortality after three years, it almost leveled off. But, most importantly, statistics say that among patients with chronic heart failure with an ejection fraction of more than 50%, less than 60% remain alive after three years, which means 40% die.
But here, I would say, is data that shocks me. If the prognosis improves with treatment for heart failure with preserved ejection fraction (and we see here the range since 1987, when we mainly talked about the cardiorenal theory of chronic heart failure), then please note, dear colleagues, nothing happens with the improvement in prognosis patients with preserved ejection fraction - just as 60% of them died three years later, strictly speaking, after diagnosis, everything remains so. This raises the question that we may not yet know exactly how to treat this form of chronic heart failure.
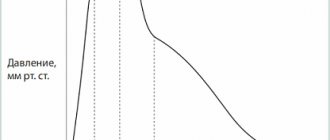
Well, very briefly I would like to remind you of the basic knowledge that we receive from the physiology course in the third year, the so-called equator (students say “equator”; having completed the third year means that you have completed half of your studies at the institute). This is the pressure-volume curve in the left ventricle, and it is the change in this curve that characterizes the main changes that occur in patients with rigid myocardium and first with diastolic dysfunction, and then with diastolic heart failure.
So, the end of diastole marks the phase of isovolumic contraction. We see that here the pressure in the left ventricle is rapidly increasing without changing its volume. The aortic valve opens and the same systole, or ejection phase, occurs. It was precisely in the shadow of this systole that there was always diastole, since we assessed the work of the heart precisely by how it contracts, by its contractile function.
Then the period of systole closes, the aortic valve naturally closes, and exactly the most interesting stage at the moment, at the time of my story today, occurs - this is diastole. The first period, it is precisely characterized by the stage of isovolumic relaxation (we see that it is very similar to the stage of isovolumic contraction), that is, a sharp decrease in pressure in the left ventricle, the mitral valve opens, and finally the filling stage occurs. You must understand that this stage is a fairly energy-intensive process, therefore, in order for diastole to be perfect, a sufficient number of macroergs is needed.
Well, the mitral valve closes, and we see (where the point that shows the mitral valve closes) that the end of diastole occurs at such a positive end-diastolic pressure. So, if the left ventricle is rigid, then this slight rise will be steeper, and the pressure that will be in the left ventricle will be higher.
The graph is two-dimensional, so it is impossible here - at least I could not - show the time, the so-called “tau”, of isovolumic relaxation. This is a very important indicator, and we will return to it below.
Thus, we can summarize those factors that influence diastole. We can summarize them by dividing them into two, in my opinion, absolutely unequal, but quite important groups. The first is, of course, the work of the ventricle, this is the early diastolic filling of the ventricle. And it is precisely factors such as: elastic return of blood to the left ventricle, contractile function of the left ventricle, stiffness of the left ventricle in diastole, properties of the pulmonary veins, area of the mitral valve opening that make an 80 percent contribution to full diastole.
But there is still a small contribution, and nevertheless, we should not forget about it either, especially when, for example, a patient comes to us with rhythm disturbances, and chronic heart failure becomes decompensated. This is the contribution of the atrium. And here the following are very important: the PQ interval, the contractile function of the atrium itself (now there are methods that evaluate this contractile function, they are not invasive - echocardiographic), heart rate (of course, the less often the heart beats, the better the diastole) and the activity of the sympathetic nervous system .
Thus, the portrait of a typical patient with arterial hypertension and diastolic heart failure is an elderly woman (usually a woman, although, of course, it can also be a man) with a long history of arterial hypertension, which is still poorly treated; with a bouquet of other pathologies, which also contributes to the possible processes of fibrosis in the heart of such patients: this is diabetes mellitus, this is coronary heart disease, this is supraventricular rhythm disturbance, kidney dysfunction, which we determine by the glomerular filtration rate, and with vascular fibrosis.
There are key differences, and we can detect them already at the stage of getting to know the patient and at the stage of his examination. Muffled heart sounds are characteristic of systolic heart failure with reduced ejection fraction. With the ejection fraction preserved, the tones can be quite decent, and even the first tone can be preserved.
Most often, we hear a gallop rhythm in both cases, and just if we are talking about systolic heart failure, then it manifests itself with the appearance of a proto-diastolic gallop rhythm - due to S3, an additional tone, a third tone. And finally, diastolic heart failure, where the greater contribution of the atria, exhausted by high end-diastolic pressure in the left ventricle, is S4.
Diastolic heart failure sometimes progresses rapidly to pulmonary edema. And here is also amazing data. Dmitry Alexandrovich, I want to discuss them with you. It turns out (I came across this article) when... Patients with pulmonary edema, completely clinically justified pulmonary edema, are admitted to the intensive care unit, and they all had their left ventricular ejection fraction measured. Then the pulmonary edema was stopped and the left ventricular ejection fraction was measured again. So, there was no pattern. It would seem that if pulmonary edema was stopped, the ejection fraction should increase, or if you were admitted with pulmonary edema, the ejection fraction should be low. There were patients with a high ejection fraction during the culmination of pulmonary edema, and vice versa.
How do you think we, as clinicians, should evaluate this, since we so often rely on this parameter - the ejection fraction?
Professor Zateyshchikov D.A.: – Well, as they say, so much the worse for the ejection fraction. In fact, many have been saying for a long time that the ejection fraction is, so to speak, not a very good parameter. And, obviously, with the advent of new non-invasive techniques - tomography, magnetic resonance imaging - we will have a more accurate method of assessment. And, perhaps, what we today accept as this very diastolic dysfunction will partially move into another category, into the systolic category. Hard to say.
But in any case, in my opinion, this once again shows that this is not the only parameter: systole is not only systole, but also something else.
Professor Drapkina O.M.: – And yet the clinic, the clinical picture is what should mainly determine our attitude towards this patient and his prognosis.
Let's get back to the slides. Thus, there are disputes, they are not over. Is this one syndrome, in which provoked diastole is, as it were, a precursor to reduced ejection fraction, or are there two syndromes? There are both supporters and opponents of various theories. To be honest, I take the position that these are still two different syndromes. Because even the portrait of these hearts, which we see during a pathological autopsy, is so different that the question immediately arises: how can such different hearts be treated with the same approaches? Well, this question is probably still eternal, there is no answer to it.
Nevertheless, we must treat such patients; we must diagnose heart failure with preserved ejection fraction. As always, algorithms come to the rescue.
The algorithm of the European Society of Cardiology also places the clinical picture of chronic heart failure at the forefront. But translating into our daily practice, this is an obese patient who came in with shortness of breath. Then normal or only slightly reduced systolic function. Let us again translate to our realities, this is a woman who came with shortness of breath, we listened to her, examined her, we see that she is obese, we see that there are fine rales in the lungs.
We send her for an echocardiographic study to clarify the diagnosis and are surprised to see that the ejection fraction is normal. This is not a reason to send this patient to a pulmonologist, this is a reason to give such a patient at least a six-minute walk test. And we will see that she may not walk the same 450 meters that would not classify her as a patient with heart failure.
Then there's really a lot of focus on biomarkers of chronic heart failure, particularly natriuretic peptide and its terminal fragment. If it is greater than 220 and we have Doppler signs, that is, we do a regular Doppler study and see when assessing flows that the E to A ratio is less than 0.5, or just the left atrium is large, or the patient has atrial fibrillation, then we can say that we have a patient with diastolic heart failure.
But, in fact, there are more difficulties than any substantiated facts, since none of the echocardiographic criteria is sufficiently accurate today. We say that tissue Doppler is very good, and this ratio E/E' is the best, but also not ideal, characterizes diastole. It is not readily available to conduct (exactly what we were talking about) MRI and various invasive hemodynamic studies. Well, in my opinion, the exact threshold values of various biological markers of heart failure have not been determined.
This raises the question: maybe we should look for possible mechanisms of diastole development in the periphery? Why? Firstly, with diastolic heart failure, certain moments of aortic stiffness also arise, but the aorta is a second heart if it is elastic. If there is an increase in the stiffness of blood vessels in general, then these reflected waves (we’ll talk about them a little later), which gather at the periphery, go to the center, to the heart. They arrive, it turns out, just at the moment of systole, they arrive a little later than they should have arrived, and collide with the newly formed pulse wave.
Again the question: does diastolic heart failure begin in the periphery? We know that blood vessels in arterial hypertension are both the culprits and the victim. Because the high pressure itself acts on the blood vessels, and at the same time the stiffness of the blood vessels, for other reasons, spasm can lead to high blood pressure.
If we talk about the main mechanisms, then, probably, the main mechanism that is responsible for the development of diastolic heart failure is precisely the increase in preload due to the stiffness of peripheral vessels. As I have already said, the speed of propagation of pulse waves increases, the preload on the left ventricle increases and the central pulse pressure increases. Right now, central pulse pressure, or pressure in the aorta, and pressure variability are given the greatest importance in the prognosis of hypertensive patients.
How does this happen? Let's imagine our vessels. Basically, these are tubes. They are elastic. And if they are elastic, as shown in the first figure, to release a blood flow - a large blood flow, since blood spreads at high speed... An elastic vessel, as it were, dampens this wave, that is, it expands a little, and then returns to normal, and we see such a schematic pulse wave, which is shown under the elastic aortic capillary tube.
If the vessel is rigid, then it cannot dampen the wave, it cannot relax a little and then contract again. And this leads to the so-called pulse wave augmentation phenomenon.
Here, dear colleagues, we can consider this phenomenon in this diagram. The gray line shows the pulse wave, which reflects the ejection of blood from the left ventricle into the aorta. The dotted line, which is shifted slightly to the right, depicts a reflected wave that comes from the periphery, from our vessels, which have damping abilities, to the center. And when these two waves are layered on top of each other, the presence of a type “C” wave occurs, or a pulse wave of type “C”, which characterizes all healthy people.
Now the arrows will show what happens in hypertensive patients, what happens with a stiff aorta. So, this graph shifts to the left, this graph shifts upward, and the formation of the so-called “A” or “B” wave occurs, which characterizes an increase in preload on the left ventricular myocardium and a decrease in diastolic blood pressure.
Thus, the analysis of this problem, in my opinion, makes it possible to provide a diagram to help the practicing physician. An increase in vascular stiffness leads to an increase in central systolic pressure in the aorta and a decrease in diastolic pressure, hence the pulse pressure increases. Increased systolic pressure in the aorta leads to increased preload on the left ventricle. Hypertrophy and the preload itself on the left ventricle and impaired relaxation lead to subendocardial ischemia. Low aortic diastolic pressure results in decreased coronary perfusion because the coronary artery fills during diastole. This diastolic pressure, which is not very low, is also important. A study of the aorta confirmed that reducing diastolic pressure below 70 for cardiovascular events is bad. Accompanying myocardial fibrosis leads to diastolic dysfunction.
We decided to conduct a pilot study in order to: evaluate the degree of damage to the endothelium and vessels of different sizes in patients with diastolic heart failure; compare different methods for assessing endothelial function - photoplethysmography and AngioScan; and see what happens during therapy based on different classes of drugs - ACE inhibitors and calcium channel blockers.
We did not forget to pay attention to biological markers. Along with the well-known N-terminal prohormone brain natriuretic peptide, we also looked at the level of galectin-3 in patients with diastolic heart failure. This is a marker, or a biological substrate that is largely responsible for fibrosis - everything: the liver, blood vessels, heart, and so on.
The study design is presented. Patients are high risk with preserved ejection fraction. We analyze endothelial function using all possible methods, randomize patients to a treatment group based on calcium channel blockers and on the basis of ACE inhibitors (amprilan was chosen as the inhibitor). We observe patients for 3-5 weeks in the hospital and then repeat the same studies.
Dear colleagues, I will not dwell on the general characteristics of the patient groups, I will only say that they were comparable in age, body mass index, and various clinical characteristics.
The first day of the study, or the start of the study, was extremely important for us, since we determined all those indicators that can be viewed during contour analysis of the pulse wave: the duration of systole, the age of the vascular wall, the augmentation index, and the stiffness index. In addition, on the same day we did an occlusion test, as if we confirmed it with each other - both by the photoplethysmographic method and according to ultrasound data.
Of course, doing this showed us that it is extremely difficult to look at endothelial function and occlusion test using ultrasound: sit in a certain position for five minutes, clamp the artery for five minutes, pump 300 mm Hg... Therefore, of course, the photoplethysmographic method won us over namely simplicity.
This is what the “C” wave approximately looked like in normal vessels.
Results. The first conclusion we made was that all patients with diastolic heart failure have pulse wave changes. Waves of type “B” and “A” are recorded, which are characterized by a high amplitude and a large range between systole and diastole.
Results of pulse wave contour analysis before the start of therapy. We see that our patients do not differ, either in the stiffness index, or in the reflection index, or in the pressure in the central vessel.
What happened during therapy? It's good to have both. That is, the lower we reduce the pressure, the better for the vessel of our hypertensive patient. Nevertheless, amprilan had a slightly greater impact on the hardness index. And amprilan also had a slightly greater effect on pressure in the aorta.
The results of the test with reactive hyperemia are an occlusion test. We also see that both groups demonstrated good results. However, a slightly greater effect of ACE inhibitors on the vascular wall was also proven in this study.
The average level of NT-proBNP hormones was 153, the average level of galectin-3 was 0.98.
The assessment of endothelial vascular function occurred in this way. We see that after an occlusion test that lasted five minutes... we would like to see an increase in diameter in the brachial artery, and below exactly what happens to the pulse waves is shown.
We found that there was an association between NT-proBNP levels and a lot of parameters, such as the 6-minute walk test, the patient's Clinical Status Rating Scale, which we use in patients with heart failure.
There was no correlation between NT-proBNP levels and left ventricular ejection fraction and parameters of diastolic dysfunction.
As for galectin-3, it turned out that once galectin-3 increased, it did not change. Which, in general, is consistent with literature data. And therefore, we propose the combined use of galectin-3 and natriuretic peptide; this can be assessed to a greater extent as a prognosis for the course of the disease.
This is a combined application. In the first column - the meaning, in the second column - the interpretation. And the risk of an unfavorable outcome, we see, is highest when there are high levels of galectin-3 and natriuretic peptides.
And finally, a clinical example. An elderly patient, over 60 years old. We see that her vessels are stiff. Both the rigidity index, the reactivity index, and the augmentation index are high. Against the background of the use of amprilan, we see a change in the pulse wave, this is visible, so to speak, visually. In addition, this, of course, can be seen from the calculated indices that exist. Please note that the reactivity index decreased from 24 to almost 8.9, and how much the central pressure decreased!
This is naturally reflected in improved endothelial function. That is, an increase... the top picture compared to the bottom picture... we see an increase in the amplitude of pulse waves by 1.3 times.
Thus, dear colleagues, the analysis of this problem makes it possible to draw such preliminary conclusions for now. It is probably true to say that diastolic heart failure begins from the periphery; in any case, vascular stiffness makes a certain contribution to changes in diastole.
The second conclusion is that biological markers of chronic heart failure are again worthy of further study, and the new marker galectin-3 for the prognosis of patients with diastolic heart failure is likely to be very promising.
And finally, our study demonstrated that lower the pressure with something, lower it to normal values, to the values that are given to us by recommendations. But still, the use of ACE inhibitors, and in particular amprilan, in our study suggested a better effect on endothelial function and a better effect on the function of vascular resistance in patients with arterial hypertension and diastolic heart failure. Thank you for your attention.