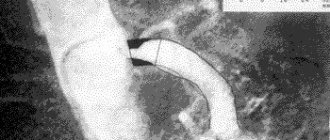
Angioplasty and stenting of the internal carotid artery (ICA) is an intervention that restores blood supply to the brain. Performed to treat, prevent and prevent stroke.
The carotid arteries are the main arteries that supply blood to your brain. They can become clogged with fatty deposits (plaques) that slow or block blood flow to the brain, a condition known as atherosclerotic carotid artery disease, which can lead to stroke.
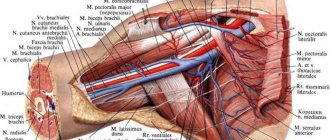
Endovascular intervention to restore full blood flow through the carotid artery is performed minimally invasively under local anesthesia through a small puncture in the common femoral artery (in the groin) or in the radial artery (in the wrist) and includes insertion, positioning and implantation of a stent at the site of narrowing of the internal carotid artery.
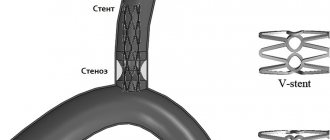
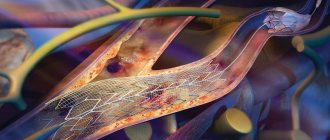
For such interventions, a trap filter (a modern device for protecting the brain from thromboembolism) is required. Then a stent is placed, which expands the artery from the inside and keeps it open (this is a self-expanding metal frame with a specially designed closed cell or double-layer stents that incorporate all the advantages of previous generations).
Angioplasty and stenting of the internal carotid artery are analogous to open surgery and can also be used when traditional carotid surgery (carotid endarterectomy) is impossible or too risky.
Indications for angioplasty and stenting of the internal carotid artery
Angioplasty and internal carotid artery (ICA) stenting may be necessary for the treatment or prevention of acute ischemic stroke if:
- Your internal carotid artery is narrowed by 70% or more, especially if you have had a stroke (then more than 50% narrowed) or stroke symptoms and are not in good enough health to have open surgery - for example, if you have severe heart disease or lungs or after radiation therapy;
- You have already had a carotid endarterectomy and are experiencing new narrowing after surgery (restenosis)
- Places of narrowing (stenosis) are difficult to reach during endarterectomy
In some cases, carotid endarterectomy may be a better choice than angioplasty and stenting to remove accumulations of fatty deposits blocking an artery. You and your doctor will discuss which procedure is safest for you.
What is coronary artery stenting?
More than 2 million stents are implanted annually. And this is understandable, because stents are used to treat one of the most common diseases - coronary heart disease.
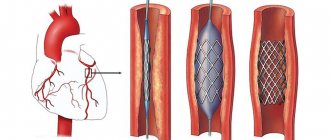
Coronary angioplasty and stenting is an intravascular treatment for coronary heart disease. The basis of coronary heart disease is the narrowing of the blood vessels that supply the heart (coronary arteries) by cholesterol plaques. Stenting allows narrowed arteries to widen. To do this, a special balloon is placed inside the artery and inflated, thus “flattening” the cholesterol plaque and restoring blood flow through the artery. After this, a metal frame—a stent—is implanted into the narrowing site to “fix” the result. In this case, there is no need to open the chest and all manipulations are carried out through a small puncture in the artery in the arm or groin.
How to prepare for the procedure
A patient preparing for surgery must inform the doctor about all medications he is taking. This also includes traditional medicine. The doctor must collect an allergy history from the patient and find out whether there is an allergy to medications, especially iodine. It is equally important to inform the specialist about any chronic or acute diseases you are suffering from.
On the eve of the operation, the patient is recommended to take antiplatelet agents and NSAIDs. If a woman is in the early stages of pregnancy, she must inform the surgeon about this. For pregnant women, manipulation is carried out only if there are strict indications. X-ray radiation can cause irreparable harm to the unborn baby. On the day of angioplasty, you should not eat or drink a lot of water.
Who is indicated for cardiac stenting?
Stenting of cardiac vessels is indicated for patients with severe angina pectoris, after myocardial infarction and pre-infarction conditions, patients with proven ischemia (lack of blood to the heart) based on the results of stress tests. In this case, the decision on stenting is made only based on the results of coronary angiography - a contrast study of the heart vessels. Coronary angiography, like stenting, is performed in the cath lab. Often coronary angiography “transitions” into vascular stenting because performed through the same puncture in the artery.
Cost of the operation
The price of the operation depends on which clinic and in which country the patient chooses. Also, the pricing policy will be influenced by the degree of complexity of the upcoming intervention and the number of affected vessels. The main cost component of surgical vasodilation is the price of the dilation device, which will remain inside the patient's body.
In Russia, prices range from 85,000 to 200,000 rubles. This is how much the operation itself, the necessary medications, and hospital stay will cost. The stent itself will cost from 45,000 to 150,000 rubles. Treatment, for example, in Israel is somewhat more expensive. Additionally, the patient will have to pay for flights, food and accommodation.
What alternative methods to stenting exist?
- Drug therapy. You need to understand that it is tablets, and not stents, that primarily reduce the risk of myocardial infarction and determine the prognosis in patients with coronary artery disease. Therefore, in many patients with controlled angina pectoris, in the absence of objective evidence of severe myocardial ischemia (lack of blood), coronary stenting can be abandoned, despite significant narrowing in the coronary arteries.
- Coronary bypass surgery. Abdominal surgery, which is often performed using a heart-lung machine. During bypass surgery, bypasses (shunts) are constructed from the patient’s arteries and veins, allowing blood to be supplied to the heart, bypassing areas of the arteries affected by cholesterol plaques.
Life and rehabilitation after angiography
Before deciding to undergo surgery, it is necessary to understand that surgical vasodilation can eliminate the consequences of the disease. The disease itself cannot be cured using this method. To avoid complications in the form of repeated stenosis of the vascular lumen, it is necessary to adhere to a healthy lifestyle and normalize nutrition. As a rule, after surgical correction the prognosis for the patient’s life is favorable.
As for well-being after surgery, most patient reviews are positive. Patients note the disappearance of ischemic pain and improvement in general well-being.
How to choose between stenting, bypass surgery and drug therapy?
This is the task of your cardiologist, who takes into account the following data:
- The severity of symptoms, namely: the severity of angina pectoris, the severity of shortness of breath, in other words, how much ischemic disease “interferes with the life” of the patient.
- Objective evidence of myocardial ischemia (lack of blood). Most often this is a stress test, ideally stress echocardiography, which should be performed by qualified doctors in a center with a large number of such studies.
- Coronary angiography data. With widespread severe damage to all three coronary arteries, the results of bypass surgery are better.
- Accompanying illnesses. If a patient has diabetes mellitus and multivessel disease of the heart arteries, for example, coronary bypass surgery is usually indicated.
Rehabilitation period
After discharge from the clinic, it is recommended to avoid physical activity for several days. If a follow-up examination and consultation with a cardiologist does not show anything alarming, the patient will soon resume his usual lifestyle.
The result after coronary artery angioplasty depends on how carefully the patient follows the instructions of the attending physician:
- For 6-12 months after angioplasty, regular use of blood thinning medications is necessary.
- Lifestyle correction is no less important: quitting smoking, weight control, special diet.
- At the appointed time, the patient will have to come to see a cardiologist and undergo a preventive examination.
Technique for stenting coronary arteries (with professional jargon)
“We install the introducer”
To get to the heart vessels, the doctor needs to get into the patient’s arterial system. For this purpose, one of the peripheral arteries is used - the femoral (in the groin) or the radial (on the forearm). Under local anesthesia, a puncture is made in the artery and an introducer is installed - a special tube, which is the “entry gate” for all the necessary instruments.
"Let's put a guide"
Then a special thin-walled tube about a meter long - a guiding catheter (“guide”) is passed through the patient’s arteries and stops, slightly short of the heart, in the aorta. It is from the aorta that the coronary arteries that supply the heart depart. The tips of the catheters are curved in such a way that it is convenient for the doctor to enter one of the coronary arteries, right or left. By controlling the catheter, the doctor “enters” one of the coronary arteries. Half the job is done.
“Starting a conductor”
But how to get to the point of maximum narrowing in the artery? To do this, we need a “rail” along which all our tools will “ride”. This rail is the coronary guidewire - a thin (0.014 inch = 0.35 mm) metal “lint” with a soft tip (so as not to “scratch” the artery during the operation). Sometimes it is quite difficult to place a guidewire behind the site of narrowing; the tortuosity of the artery, the angle of departure of the branches of the artery, or pronounced narrowing due to the presence of plaques interfere. You can take a “harder” or “slipperier” conductor. Well, or just a favorite, because every doctor has his own preferences. One way or another, the guide ends up behind the site of narrowing on the periphery of the artery that we want to stent.
"Ballooning"
The first instrument that gets to the site of narrowing of the artery is a coronary balloon with a diameter most often from 1 to 3.5 mm and a length of 10-20 mm. The balloon is put on the conductor and moves along it to the point of maximum narrowing where it inflates. The pressure inside the cylinder reaches 15-20 A
Next, along the conductor, to the place that was narrowed before the balloon was inflated, the same balloon is inserted, on the surface of which a stent is fixed in a folded state. The balloon is inflated, the stent is expanded and “pressed” into the artery wall. The stent does not always expand perfectly and then the final stage of the procedure is needed - postdilatation (in simple terms - re-inflation).
"Let's blow it out"
A rigid balloon is placed inside the implanted stent and inflated with high pressure (up to 25 atmospheres). Most often, after this, the stent straightens and adheres well to the walls of the artery.
Features of angioplasty
Angioplasty is one of the methods of endovascular treatment. The advantage of angioplasty is that it is less traumatic for the patient and does not require general anesthesia or a long hospital stay. Angioplasty is considered a minimally invasive type of intervention on a vessel, since reconstruction is carried out from the inside. Angioplasty is usually combined with a stenting procedure. During stenting, a stent is implanted into the vessel, which subsequently keeps the vascular walls from narrowing.
Hemostasis
What to do with a hole in an artery?
If the intervention was carried out through the radial artery (on the arm), a special bracelet with a cushion (hemostatic cuff) is put on the wrist, which will put pressure on the injection site and prevent bleeding. Depending on the situation, the cuff will remain on the arm from 3 to 12 hours.
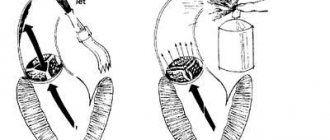
In case of femoral access, there are 2 main options:
- Manual (manual) hemostasis. After the introducer is removed, the doctor presses with his hands on the injection site for 15 minutes. Then apply a pressure bandage for 6-8 hours. The patient should lie on his back with his leg straight.
- Closure devices are special “plugs” that allow you to close the artery from the inside. In this case, there is no need to put pressure on the leg and a pressure bandage is not needed. A special patch is applied to the injection site and several hours of bed rest are recommended.
Stenting is completed.
Literature
- DORMANDY JA, MAHIR MS. The natural history of peripheral atheromatous disease of legs. In: Greenhalgh RM, Jamieson CW, Nicolaides AN, (ed.), Vascular surgery. Issues in current practice. London, Grune & Stratton, 1986 pp 3-17.
- MARTY-ANE C, ALAUZEN M, MARY H. L'expectative medicale dans les lesions obstructives isolees de l'art e re femorale superficielle. In: B ranche reau A, Jausseran JM, (eds), Traitement des lesions obstructives de l'artere femorale superficielle. Marseille, CVN, 1992 pp. 13-17.
- JOFFRE F, ROUSSEAU H, MEITES G, CHEMALI R. Resultats a long terme des angioplasties femoro-poplitees. In: Branchereau A, Jausseran JM, (eds), Traitement des lesions obtructives de l'artere femorale superficielle.Marseille, CVN, 1992 pp 39-51.
- JOHNSTON KW. Femoral and popliteal arteries: reanalysis of results of balloon angioplasty. Radiology 1992; 183: 767-771.
- HUNINK MGM, DONALDSON MC, MEYEROVITZ MF et al. Risks and benefits of femoropopliteal percutaneous balloon angioplasty. J Vasc Surg 1993; 17: 183-194.
- BECQUEMIN JP, CAVILLON A, HAIDUC F. Surgical transluminal femoropopliteal angioplasty: multivariate analysis outcome. J Vasc Surg 1994; 19: 495-502.
- MATSI PJ, MANNINEN HI. Impact of different patency criteria on long-term results of femoropopliteal angioplasty: analysis of 106 consecutive patients with claudication. J Vasc Interv Radiol 1995; 6: 159-163.
- STANLEY B, TEAGUE B, RAPTIS S et al. Efficacy of balloon angioplasty of the superficial femoral artery and popliteal artery in the relief of leg ischemia. J Vasc Surg 1996; 23: 679-685.
- COURBIER R. Le traitement des lesions de l'artere femorale superficielle. In: Branchereau A, Jausseran JM, (eds), Traitement des lesions obtructives de l'artere femorale superficielle. Marseille, CVN, 1992 pp XIII-XIV.
- DIETHRICH EB, PAPAZOGLOU K. Endoluminal grafting for aneurysmal and occlusive disease in the superficial femoral artery: early experience. J Endovasc Surg 1995; 2: 225-239.
- BERGERON P, PINOT JJ, POYEN V et al. Long-term results with the Palmaz stent in the superficial femoral artery. J Endovasc Surg 1995; 2: 161-167.
- AHN SS, RUTHERFORD RB, BECKER GJ et al. Reporting standards for lower extremity arterial endovascular procedures. J Vasc Surg 1993; 17: 1103 -1107.
- BRAY AE, LIU WG, LEWIS WA et al. Strecker stents in the femoral arteries: value of Duplex ultrasonography in restenosis assessment. J Endovasc Surg 1995; 2: 150-160.
- BECKER GJ, KATZEN BT, DAKE MD. Noncoronary angioplasty. Radiology 1989; 170: 921-940.
- MATSI PJ, MANNINEN HI, VANNINEN RL et al. Femoropopliteal angioplasty in patients with claudication: primary and secondary patency in 140 limbs with 1-3 year follow-up. Radiology 1994; 191: 727733.
- Guidelines for percutaneous transluminal angioplasty. Standards of Practice Committee of the Society for Cardiovascular and Interventional Radiology. Radiology 1990; 177: 619-626.
- MURRAY RR Jr, HEWES RC, WHITE RI Jr et al. Long-segment femoropopliteal stenoses: is angioplasty a boom or a bust ? Radiology 1987; 162: 473-476.
- CURRIE IC, WAKELEY CJ, COLE SE et al. Femoropopliteal angioplasty for severe limb ischemia. Br J Surg 1994; 81: 191-193.
- SIVANANTHAN UM, BROWNE TF, THORLEY PJ, REES MR Percutaneous transluminal angioplasty of the tibial arteries. Br J Surg 1994; 81: 1282-1285.
- BLAIR JM, GEWERTS BL, MOOSA Hetal. Percutaneous transluminal angioplasty versus surgery for limb-threatening ischemia. J Vasc Surg 1989; 9: 698-703.
- SEEGER JM. Laser angioplasty. A vascular surgeon's view. Circulation 1991; 83 (I): 97-98.
- SATIANI B, DAS BM, VACCARO PS, GAWRON D. Angiographic follow-up after laser-assisted balloon angioplasty. J Vasc Surg 1993; 17: 960-966.
- FISHER CM, FLETCHER JP, MAY Jetal. No additional benefit from laser in balloon angioplasty of the superficial femoral arter y. Eur J Vasc Endovasc Surg 1996; 11: 349-352.
- DALSING MC, HARRIS VF. Intravascular Stent. In: White RA, Fogarty TJ, (eds), Peripheral endovascular interventions. St Louis, Mosby, 1996 pp 315-339.
- HENRY M, AMOR M, HENRY I et al. Placement of Palmaz stent in femoropopliteal art eries: a six year experience. Factors influencing restenosis and longterm results. In: Abstract Book 6° International course on peripheral vascular intervention. Oct 1995, Nancy, France.
- WHITE GH, LIEW SCC, WAUGH RC et al. Early outcome and intermediate follow-up of vascular stents in the femoral and popliteal arteries without long-term anticoagulation. J Vasc Surg 1995; 21: 270-281.
- DO-DAI-DO, TRILLER J, WALPOTH BH et al. A comparison study of self-expandable stents vs balloon angioplasty alone in femoropopliteal artery occlusions. Cardiovasc Intervent Radiol 1992; 15: 306-312.
- HENRY M, AMOR M, HENRY I et al. Endoluminal bypass grafting in leg arteries with the Cragg Endopro System 1. A series of 105 patients. In Abstract book 6° International course on peripheral vascular intervention. Oct 1995, Nancy, France.
- G. Agrifiglio et al.1999