–>
Blood pressure is the pressure of blood on the walls of blood vessels.
Blood pressure is the pressure of blood in the arteries.
Several factors influence blood pressure:
1. The amount of blood entering the vascular system per unit time.
2 . The intensity of blood outflow to the periphery .
3. Capacity of the arterial segment of the vascular bed.
4. Elastic resistance of the walls of the vascular bed.
5. The rate of blood flow during cardiac systole.
6. Blood viscosity
7. The ratio of the time of systole and diastole.
Blood pressure measurement
Blood pressure measurement can be carried out both at rest and during physical or psycho-emotional stress, as well as at intervals between various types of activity. Blood pressure is most often measured while sitting (your back should be supported, as any form of isometric exercise causes an immediate increase in blood pressure) or lying down.
Measuring blood pressure requires rest (no talking or making sudden movements).
Is it necessary to measure blood pressure in both arms?
Increased blood pressure
Hypertension (arterial hypertension) is a persistent increase in blood pressure in large arteries of more than 140/90 mm Hg. Increased blood pressure is the main risk factor for the development of vascular diseases of the brain, coronary heart disease, heart and kidney failure, and eye damage.
The main goal of treating hypertension is not to knock down, but to gradually reduce blood pressure, aiming to achieve a level of 120-130/80 mmHg. Art. For elderly patients, it is advisable to reduce blood pressure to higher values (140-145/85-90 mm Hg). An excessive decrease in blood pressure is dangerous for patients with arterial hypertension with left ventricular hypertrophy, coronary artery disease and cerebral vascular pathology, since this deteriorates the blood supply to the vessels of the heart and brain.
Is it possible to cure arterial hypertension? Is it necessary to reduce systolic blood pressure in old age?
Lowering blood pressure without drugs?
Upper and lower blood pressure
The tonometer shows two numerical values, one of which is slightly higher than the other. For example, 110/70 or 120/80. These numbers, SYS (systole, first value) and DIA (diastole, second value), indicate the work of the heart muscle in different states.
Systolic (upper) pressure
-
pressure
on the walls of blood vessels during contraction of the heart muscle (systole).
A high upper
reading with a normal lower reading is considered a manifestation of heart disease.
Diastolic (bottom) pressure
-
pressure
on the walls of blood vessels during relaxation of the heart muscle (diastole).
A high
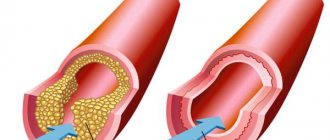
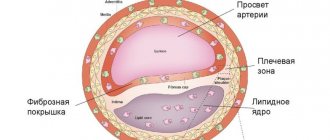
lower reading with a normal upper reading is a sign of atherosclerosis or kidney disease.
A mechanical tonometer is more accurate than an electronic one
A healthy person's blood pressure
decreases during sleep and increases with physical activity. Its norms gradually change with age. Adequate indicators in adolescence are 110/70, in adults - 120/80, in the elderly - no higher than 140/90.
Normal pressure readings
Low blood pressure
Hypotension (arterial hypotension) is a persistent decrease in blood pressure below normal, low blood pressure. The magnitude of this decrease varies from person to person, but is usually below 100/60 mmHg. Art. for men and 95/60 mm Hg. Art. for women.
The causes of low blood pressure can be different: dehydration, blood loss, heart failure, heart defects, poisoning, chronic infections (tuberculosis), tumors, hypovitaminosis, but the most common cause of hypotension is vegetative-vascular dystonia.
Low blood pressure is associated with impaired vascular tone. Normally, blood vessels can quickly narrow and expand when necessary, but in hypotensive patients this reaction is slow, which leads to insufficient blood flow to organs and tissues. As a result, the body's systems and organs experience oxygen starvation and are unable to function optimally.
If blood pressure tends to persistently deviate from the norm, both upward and downward, observation and examination by a general practitioner is necessary in order to select adequate comprehensive treatment using medicinal and non-medicinal methods of therapy.
Consultation with a general practitioner
Make an appointment with a therapist
The clinic provides appointments under a voluntary health insurance (VHI) policy. View the list of insurance companies.
Effective control of arterial hypertension is the key to a high quality of life
Hypertension (essential arterial hypertension) is a disease characterized by a persistent increase in blood pressure above 140/90 mmHg, a decrease in the adaptive capabilities of the cardiovascular system, disruption of the mechanisms regulating hemodynamics, acceleration of age-related vascular changes, and progressive complications. Hypertension (HT) is one of the most common diseases in economically developed countries, where it affects up to 25% of the population. In Russia, about 40 million people have high blood pressure (BP). The situation is aggravated by the fact that in our country only 59% of patients with arterial hypertension know about their disease, of which 22–47% receive treatment, and it is effective in only 5–17%. The lack of an effective system for organizing the prevention, diagnosis and treatment of arterial hypertension (AH) is the main reason that the incidence of strokes in Russia is 5 times higher than in the USA and Western European countries. How to measure blood pressure correctly? Certain rules must be strictly followed to avoid mistakes. Cuff. It is important that the blood pressure cuff matches the volume of the arm. Typically, blood pressure measuring devices come with a standard cuff; for people with excess body weight (upper arm circumference more than 36 cm) and children, there are special cuffs. Conditions Mode. It is recommended to measure blood pressure regularly, without focusing on how you feel. in case of exacerbation of hypertension - at least 2-3 times a day. If your health worsens, be sure to measure your blood pressure! It is advisable to record the measurement results in a diary in order to analyze the data obtained and adjust the therapy by the attending physician. What affects the prognosis of the disease? The higher the blood pressure, the greater the likelihood of developing cardiovascular complications. But the prognosis of the course of hypertension is also influenced by other risk factors for cardiovascular diseases (CVD): smoking, overweight, psycho-emotional stress, low physical activity, lipid metabolism disorders, as well as the presence of concomitant diseases: diabetes mellitus, target organ damage (heart, brain). Arterial hypertension itself is the most serious risk factor for the development of coronary heart disease, including myocardial infarction, angina pectoris and its other forms, and the main cause of vascular diseases of the brain, including stroke. Therefore, with any increase in blood pressure, it is necessary to determine the factors influencing the prognosis of the disease. The total risk of CVD consists of a combination of the listed diseases and risk factors. According to WHO recommendations, it is the magnitude of the total risk, and not just the level of increase in blood pressure, that determines the correct treatment tactics for high blood pressure.
Drug treatment of hypertension The goal of treatment of hypertension is to reduce the total risk of cardiovascular complications, which involves not only taking medications prescribed by a doctor to reduce blood pressure to the target level, but also eliminating risk factors. The target blood pressure level is the blood pressure value that should be achieved in all middle-aged patients (less than 140/90 mmHg). In patients with diabetes, it is necessary to reduce blood pressure below 130/80 mmHg. Requirements for modern antihypertensive drugs to ensure effective blood pressure control: – proven effectiveness in reducing the risk of CVD; – minimum side effects (well tolerated) with long-term use; – a uniform decrease in blood pressure throughout the day – long-acting (within 24 hours) drugs are preferable; – metabolic neutrality, that is, does not lead to undesirable deviations in metabolism; Hypertensive crisis. How to help yourself during a hypertensive crisis? Hypertensive crisis (HC) is a variant of exacerbation of hypertension, accompanied by a sharp rise in blood pressure (on average up to 180/100 - 220/120 mm Hg, depending on individual tolerance), deterioration of well-being and often leading to complications. HA can be caused by: – inadequately selected antihypertensive therapy; – irregular intake of medications prescribed by a doctor; – emotional stress; – physical overload; – weather sensitivity; – heavy smoking; – alcohol abuse; – overeating; A hypertensive crisis always requires immediate treatment! How to help yourself during a hypertensive crisis? If you feel a sharp, severe headache. palpitations, nausea, vomiting began, visual disturbances, convulsions appeared, then it is necessary: 1. Measure blood pressure. With a significant increase in blood pressure (on average DL 180/100 - 220/120 mm Hg: - take a quick-acting drug (tablet under the tongue): nifedipine (Corinfar 10 mg), captopril (Capoten 25-50 mg); - if chest pain appears (manifestation of angina) - nitroglycerin under the tongue or nitrospray; - do not use ineffective drugs - papazole, dibazole tablets. 2. If blood pressure does not begin to decrease within 15 - 20 minutes after taking the medication and your health does not improve, then it is necessary to call "emergency medical care" doctor. You need to know that you cannot sharply reduce blood pressure, especially in old age. The basic principles of effective control of hypertension are strict adherence to the doctor's recommendations; - self-monitoring of blood pressure at home; - the ability to eliminate unfavorable factors that provoke an increase in blood pressure and complicating treatment, follow recommendations for reducing risk factors; - continuity of drug treatment, consistency in taking prescribed medications; - ability to provide first aid during a crisis; – adherence to precautions when taking antihypertensive medications, in particular not to drink alcoholic beverages; – combined drug and non-drug treatment leads to less pronounced side effects; – to effectively control blood pressure, the doctor prescribes various drugs: those that lower blood pressure, lower cholesterol levels, normalize the lipid profile, affect blood clotting, sedatives, and others. Compliance with prescribed medication is important. Every patient with hypertension should have a clear understanding of their disease, meaningfully follow recommendations for normalization and lifestyle changes, adhere to proper treatment, and be able to independently control the course of the disease, which has already developed and will accompany the patient throughout his life. Make an appointment Violation of blood pressure is a dysfunction cardiovascular system, expressed as an imbalance between the magnitude of cardiac output and the resistance of blood vessels to it. Blood pressure disorders are one of the most common diseases in the world. Its two dysfunctions are hypertension
and
hypotension
.
Hypertension or hypertension is the most common form of blood pressure disorder, although hypotension (hypotension) is similar in its formation mechanism and can take equally dangerous forms. Blood pressure depends on the work of the heart, the tone of the arteries and can change under the influence of various factors (physical activity, emotions, diseases). Arterial pathologies mean a long-term and stable failure of blood pressure to return to normal values. Short-term changes in blood pressure are considered to be hyper- or hypotensive reactions. Arterial hypertension
is a sustained increase in blood pressure up to 160/95 mm Hg.
Art. and higher. Hypertension is one of the most common diseases, affecting at least 20-30% of the population. With a sustained increase in blood pressure, the risk of stroke or myocardial infarction inevitably increases. Causes The causes of hypertension are often a violation of the neurohormonal functioning of the heart, leading to its excessive emission. Risk factors include excess weight, smoking, hereditary predisposition, unbalanced diet, lack of sleep and physical activity, and prolonged stressful situations. Hypertension can be primary or secondary, resulting from another disease. Such causes may include, in particular, various kidney diseases, tumors, as well as any other diseases that affect the kidneys. When the kidneys are weak, the excretion of sodium and water is delayed, which in turn affects the increase in blood pressure. In renal hypertension, there is a relationship between exacerbation of kidney disease and increased pressure, and diastolic pressure increases to a greater extent. As a result, signs of renal failure develop along with hypertension. Atherosclerotic hypertension is also widespread, usually developing in old age. It is characterized by high systolic pressure and low diastolic pressure. It develops due to damage to the arteries or blood vessels of the brain. Hypertension with problems with the endocrine system is much less common and can be caused by tumor processes. In addition, arterial hypertension can be caused by any disease leading to damage to the central nervous system. Symptoms: Dizziness, tinnitus, feeling of heaviness in the head, palpitations. Arterial hypotension
is a persistent decrease in blood pressure below 100/60 mmHg. Art. The main danger of hypotension is that it leads to insufficient blood supply, which results in oxygen starvation of many organs and the brain. Therefore, hypotension must be treated. Hypotension occurs most often in women. However, in 80% of them it is primary, or so-called neurocirculatory, caused by high fatigue. Causes: Causes of decreased blood pressure may include large blood loss, anemia, severe loss of body fluids, heart failure, or an overdose of certain drugs. Dysfunction can also be observed with decreased thyroid function, with diseases of the endocrine systems and adrenal glands, or with nervous exhaustion. Thus, changes in blood pressure can be caused by a variety of factors and problems. Accordingly, treatment must begin with a search for the cause of this dysfunction. To do this, as a rule, a thorough examination is prescribed, including tests, determination of cholesterol and sugar levels, ECG, ultrasound of the kidneys, heart and examination of the brain. Symptoms: Weakness, lethargy, drowsiness, apathy, dizziness. Treatment In the treatment of blood pressure disorders in Western medicine, in most cases, symptomatic (lowering or increasing blood pressure) is used, against the background of general treatment of the underlying pathological process. However, this may not be successful in all cases. Chinese medicine, in the case of any blood pressure disorder, also first of all looks for and works with the immediate cause of the disease, acting comprehensively on all the factors and dysfunctions that form it, thereby restoring the normal functioning of the cardiovascular system. Thus, for hypotension, the treatment process will be focused on increasing vascular tone, the patient’s level of vitality and activity, as well as stimulating the body’s own reserves. Modern medicine classifies hypertension as a problem that requires almost lifelong drug support. But despite the presence of a significant number of drugs that lower blood pressure, the use of these drugs still leads patients suffering from blood pressure to an extremely unpleasant outcome - myocardial infarction, or stroke. However, when you stop taking them, the disease inevitably progresses. In this sense, arterial hypertension is similar to drug addiction, and thus poses a serious problem for modern medicine. Chinese medicine first determines the type of hypertension. Depending on it, subsequent treatment is determined. Chinese medicine considers prolonged emotional stress, overwork, and slagging of the body to be the main causes of hypertension. Imbalance of the Yin-Yang of the Liver and Kidneys causes “Fullness above and Emptiness below.” Depending on the syndrome, arterial hypertension is divided into three forms in its course: excess Liver Yang - Yin Emptiness, Yang excess - Yin Emptiness and Yang Emptiness. And the main goals of treatment are filling the Emptiness, expelling Fullness (excess), harmonizing Yin and Yang (taking into account the possible stagnation of Wind and Phlegm). And the leading principle will be the removal of toxins from the body and restoration of a healthy balance in it. In its arsenal, Chinese medicine also has first aid “remedies” for a sharp increase in blood pressure. As with conventional treatment, a quick effect occurs with the help of acupuncture, tsubo therapy, and acupressure. Guasha massage, acupressure massage of the feet and vacuum massage also have good effectiveness in the general treatment of hypertension. All these natural treatments are non-addictive, non-toxic and have no side effects, which, without exaggeration, is vital in such a serious case as hypertension. Treatment methods of traditional Chinese medicine are cumulative in nature. But even one course completed by an experienced specialist will definitely give a lasting and confidently positive effect. Return to the “We treat” section
Why know your blood pressure?
Increase in pressure for every 10 mm Hg. increases the risk of developing cardiovascular diseases by 30%. People with high blood pressure are 7 times more likely to develop cerebrovascular accidents (stroke), 4 times more likely to develop coronary heart disease, and 2 times more likely to develop vascular damage to the legs. It is by measuring blood pressure that it is necessary to begin the search for the cause of such frequent manifestations of discomfort as headache, weakness, and dizziness. In many cases, blood pressure requires constant monitoring, and measurements should be taken several times a day.
What methods are used to measure blood pressure?
There are 2 methods currently widely used to measure blood pressure:
Korotkoff method
This method, developed by the Russian surgeon N. S. Korotkov in 1905, uses a very simple device for measuring blood pressure, consisting of a mechanical pressure gauge, a cuff with a bulb and a phonendoscope. The method is based on complete compression of the brachial artery with a cuff and listening to sounds while slowly releasing air from the cuff.
Advantages:
– recognized as the official standard for non-invasive blood pressure measurement for diagnostic purposes and for verification of automatic blood pressure meters;
– high resistance to hand movements.
Flaws:
– depends on the individual characteristics of the person making the measurements (good vision, hearing, coordination of the “hands-vision-hearing” system);
– sensitive to noise in the room, the accuracy of the location of the phonendoscope head relative to the artery;
– requires direct contact of the cuff and microphone head with the patient’s skin;
– technically complex (increases the likelihood of erroneous indicators during measurement) and requires special training.
Arterial hypertension in children and adolescents with endocrine pathology
Part 1
Arterial hypertension (AH) is one of the types of cardiovascular pathology that significantly affects morbidity and mortality. There are primary (essential) and secondary (symptomatic) arterial hypertension. Essential hypertension is a heterogeneous disease with progressive damage to organs and systems with different development mechanisms at the initial stages. It is of primary importance among middle-aged and elderly people. Secondary hypertension, which includes endocrine hypertension, accounts for 15% of cases in the population. Moreover, in children they occur much more often than in adults, and at primary school age, secondary hypertension predominates [1]. This article discusses one of the common types of secondary arterial hypertension - hypertension caused by endocrine diseases.
Physiological mechanisms of blood pressure regulation
Blood pressure is created due to the fact that the heart throws blood into the vessels, overcoming great resistance to its movement. Vascular tone is determined mainly by the state of their smooth muscles.
In arterial vessels, blood pressure fluctuates significantly depending on the phase of the cardiac cycle - systole, diastole. Systolic blood pressure (SBP) is formed due to the energy of ventricular systole during the period of expulsion of blood from them. Diastolic blood pressure (DBP) is determined by the elasticity of the walls of arterial vessels.
In a healthy body, maintaining a normal blood pressure level is carried out by a multicomponent system, which is represented by neurogenic, humoral and local factors. They act in inextricable connection with each other and are complementary.
The control of pressor and depressor reactions is associated with the activity of the bulbar vasomotor center. It is controlled by hypothalamic structures and the cerebral cortex and is realized through changes in the activity of sympathetic and parasympathetic nerves.
The activity of the autonomic nervous system is influenced by both genetic factors and environmental factors (stress, physical activity, body weight). Increased activity of the sympathetic nervous system (SNS) leads to increased contractile activity of the myocardium and increased tone of vascular smooth muscles. The hypertensive effect of the sympathetic nervous system is also realized through the suppression of the synthesis of nitric oxide (NO), which has a vasodilating effect. In addition to its direct influence, the hypothalamus coordinates vascular tone through the endocrine system (neurohypophysis and adenohypophysis).
Rapid regulation of blood pressure is carried out by the release of adrenaline and norepinephrine from the adrenal medulla. Both hormones have different effects on blood pressure. Adrenaline increases blood pressure mainly due to increased heart function, minute volume, and pulse rate. Norepinephrine produced in neurons has a direct effect on vascular tone. The pressor effect of adrenaline is much stronger. By directly acting on adrenergic receptors, which cause vasoconstriction, norepinephrine increases both systolic and diastolic blood pressure [2].
The renin-angiotensin-aldosterone system (RAAS) forms the foundation of modern ideas about the regulation of blood pressure.
Renin is a proteolytic enzyme synthesized in the juxtaglomerular apparatus of the kidneys. It is one of the renal pressor factors. Its effect on vascular tone is mediated through angiotensin. Once in the blood, renin converts angiotensinogen into angiotensin I. The release of renin is controlled by three main mechanisms: baroreceptors in the walls of the afferent renal artery, which are stimulated when perfusion pressure decreases; receptors of the heart and large arteries, which activate the sympathetic nervous system, leading to an increase in the level of catecholamines in the blood and direct stimulation of the juxtaglomerular apparatus (via β-adrenergic receptors); the content of sodium ions in the distal tubules of the nephrons. Renin release inhibitors include angiotensin II, thromboxane, endothelin, NO, and atrial natriuretic peptide (ANP).
Angiotensinogen is a peptide synthesized in the liver. Glucocorticoids, estrogens, insulin, and thyroid hormones increase the production of this protein. With a decrease in sodium content in the body, accompanied by an increase in renin levels, the rate of angiotensinogen metabolism increases sharply. The mechanism of increased hepatic production of angiotensinogen is unclear, although angiotensin II is known to stimulate the production of the former.
Angiotensinogen, which does not have pressor activity, is hydrolyzed to form angiotensin I, a biologically inactive substance. Under the action of angiotensin-converting enzyme (ACE), angiotensin I is converted to angiotensin II, which is a highly active endogenous pressor factor. ACE also inhibits bradykinin, i.e. it itself is a key element in the regulation of blood pressure.
Angiotensin II is the main hormone in the RAAS chain, causing a rapid increase in blood pressure and total peripheral vascular resistance (TPVR). It stimulates the synthesis and secretion of aldosterone in the adrenal glands and the secretion of antidiuretic hormone, excites the sympathetic system (by facilitating the secretion of norepinephrine by nerve endings and increasing the sensitivity of smooth muscle fibers to this transmitter). Under the influence of angiotensin II, the secretion of adrenaline increases and cardiac output increases.
A similar renin-angiotensin-aldosterone system was found in various organs and tissues (heart, kidneys, brain, blood vessels). It has been shown that the activity of tissue RAAS depends largely not on ACE, but on other enzymes (chymases, cathepsin G, etc.). Increased activity of tissue RAAS causes long-term effects of angiotensin II, which are manifested by structural and functional changes in target organs.
The physiological effects of angiotensin II are realized through specific angiotensin receptors. There are two classes of angiotensin II receptors - AT1 and AT2. The cardiovascular, renal, and adrenal effects of angiotensin II are realized through AT1 receptors.
Acting directly on the adrenal cortex, angiotensin II stimulates the secretion of aldosterone, as well as its precursors - less active mineralocorticoids - deoxycorticosterone, 18-hydroxycortisone, 18-hydroxydeoxycorticosterone. The main stimulator of aldosterone production is renin. Its secretion is partly dependent on adrenocorticotropic hormone (ACTH).
Aldosterone plays a key role in regulating sodium and potassium balance. The synthesis and secretion of aldosterone is regulated in two ways. The slow mechanism depends on the K+/Na+ balance and maintains basal secretion. An increase in serum potassium levels stimulates the synthesis of aldosterone in the zona glomerulosa of the adrenal cortex. The fast regulatory pathway depends on circulating blood volume (CBV) and is controlled by the renin-angiotensin system. Aldosterone exerts its specific effect through the mineralocorticoid receptor, which is located in epithelial cells (distal parts of the nephron and other organs) that transport sodium. The direct effect of aldosterone is carried out by increasing the entry of sodium into the cell and activating the Na+/K+ pump, not only in the renal tubules, but also in the intestines, sweat and salivary glands. Aldosterone is also involved in the processes of vascular remodeling and myocardial fibrosis.
Vasopressin is an antidiuretic hormone (ADH) of the hypothalamus, accumulates in the posterior lobe of the pituitary gland and is then secreted into the blood. Vasopressin increases blood volume, increases vascular tone, increasing peripheral resistance. The development of hypertension is facilitated by an increase in the sensitivity of the vascular wall to the constrictor effect of catecholamines, under the influence of ADH.
Estrogens and glucocorticoids increase serum aldosterone concentrations indirectly through an increase in the production of angiotensinogen in the liver and an increase in the formation of angiotensin II. The pressor effect of glucocorticoids is also achieved by increasing the sensitivity of the vascular wall to the effects of catecholamines.
So, hormones are directly involved in the regulation of vascular tone. With pathology of the endocrine organs, this can form severe and persistent hypertension.
The feedback mechanism is provided by the function of baroreceptors, which are located in the aortic arch, sinocarotid zone and renal arteries. With an increase in blood pressure through these reflexogenic zones, the depressor effect on the vasomotor center increases, which leads to inhibition of sympathetic and increased parasympathetic activity with a decrease in the formation of hypertensive factors. This reduces heart rate and force and peripheral resistance.
A powerful vasodilator that lowers blood pressure is atrial natriuretic peptide, which is synthesized by atrial cardiomyocytes. It is actively released during atrial stretching caused by hypervolemia, stimulation of β-adrenergic receptors, exposure to angiotensin II, endothelin and hypernatremia. This peptide increases sodium excretion by the kidneys, suppresses the RAAS, SNS, and vasoconstrictor factors of the vascular endothelium.
The endothelin system corrects the basic regulation of blood pressure. Endothelins are peptides synthesized in endothelial cells that cause vasoconstriction by acting on type A endothelin receptors. A smaller part of endothelin, interacting with type B endothelin receptors, stimulates the synthesis of nitric oxide (NO) and causes vasodilation. NO synthesis also increases under the influence of moderate physical activity, angiotensin II, vasopressin, and catecholamines.
Other endothelial factors that significantly influence vasodilation are kinins. Representatives of this group are bradykinin and kallidin. Kinins have a vasodilatory effect by activating prostaglandins and nitric oxide; have natriuretic and diuretic effects. These vasoactive factors of the vascular endothelium are realized through their effect on vascular smooth muscle [3].
The development of hypertension in some endocrine diseases is based on the excessive production and secretion of hormones that have a direct or indirect effect on vasospasm. Timely diagnosis of endocrine pathology allows you to correctly interpret the cause of increased blood pressure and exclude essential hypertension.
Hypothyroidism and thyrotoxicosis
Thyroid hormones have a direct effect on cardiac function and vascular tone. Arterial hypertension occurs in both hypothyroidism and thyrotoxicosis.
In hypothyroidism, DBP mainly increases. This is due to bradycardia, weakening of myocardial contractility. The speed of blood flow decreases and the volume of circulating blood decreases. The secretion of natriuretic hormone is disrupted, which causes sodium and water retention in the body. The secretion of renin and aldosterone does not change. The sensitivity of vascular receptors to circulating catecholamines increases. Vascular resistance is increased by more than 50%, diastolic filling time is increased. Hyperlipidemia (64%) contributes to the development of hypertension, accelerating the formation of the atherosclerotic process. In this case, it is similar to essential hypertension.
Increased blood pressure is a common symptom of thyrotoxicosis. The pathogenesis of hypertension in thyrotoxicosis is associated with an increase in cardiac output, an increase in cardiac output, activation of the kallikrein-kinin system, hypersecretion of adrenomedullin, and functional hypercortisolism.
Thyroid hormones directly bind to cardiomyocytes, exerting a positive inotropic effect. They increase the sensitivity and expression of adrenergic receptors and, as a result, increase sensitivity to catecholamines. The heart rate increases and blood flow accelerates. Systolic pressure increases. Hypertension in thyrotoxicosis is called high-output syndrome, but there is no left ventricular hypertrophy. The latter is explained by a decrease in diastolic blood pressure.
Skin vessels dilate compensatoryly (reaction to release heat). They feel warm and moist to the touch. General and peripheral resistance are reduced. It has been shown that in thyrotoxicosis the kinin-kallikrein system is activated. In recent years, the participation of adrenomedullin in reducing DBP in patients with thyrotoxicosis has been proven. The peptide adrenomedullin has very pronounced vasodilator activity.
An increase in systolic blood pressure and a tendency towards a decrease in diastolic blood pressure is accompanied by an increase in pulse blood pressure. Patients may feel a pulsation in the head with each systole. The pulse is characterized by a rapid rise and sudden decline of the pulse wave (pulsus celer et altus). In addition, thyrotoxicosis is accompanied by an increase in blood volume and erythrocyte mass. A persistent increase in blood pressure is detected in patients with a history of the disease of more than 3 years. Patients with thyrotoxicosis develop hypertension much more often than the general population [4, 5, 7].
Hyperparathyroidism
Hypertension in hyperparathyroidism is caused by the effect of an excess amount of ionized calcium on vascular tone. To contract vascular smooth muscle cells, calcium ions are required, which enter the cytoplasm of the cells and interact with the protein calmodulin. The resulting complex (calcium + calmodulin) activates myosin light chain kinase, resulting in contraction of smooth muscle fibers. Calcium in high concentrations can excessively enhance cellular metabolic processes. Transmembrane transport of calcium ions occurs through special calcium channels. Since the concentration of calcium ions in the blood is closely related to the contractility of smooth muscles, hypercalcemia leads to increased resistance to blood flow in the peripheral arteries. On the other hand, excess calcium, irritating the sympathetic nervous system, indirectly stimulates the release of catecholamines. Experimental data have shown that the calcium-induced increase in peripheral vascular resistance is sharply reduced after adrenalectomy. Long-term excess calcium can lead to calcification of blood vessels and increased blood pressure [6, 7].
Diabetes
Diabetes mellitus (DM) is recognized as a worldwide non-infectious pathology. The increase in life expectancy of patients with diabetes has brought to the fore the problem of late vascular complications. Diabetes mellitus and arterial hypertension are two interrelated pathologies that have a powerful mutually reinforcing damaging effect aimed at several target organs at once: the heart, brain vessels, and retina.
The mechanisms of development of hypertension in type 1 and type 2 diabetes differ. In type 1 diabetes, hypertension in 90% of cases is formed as a result of diabetic nephropathy (DN). Microalbuminuria (early stage of DN) is detected in patients with type 1 diabetes with a disease duration of less than 5 years, and increased blood pressure usually develops 10–15 years after the onset of type 1 diabetes.
Hyperglycemia is the main cause of damage to the microvasculature, including glomerular vessels. Chronic hyperglycemia activates the processes of non-enzymatic protein glycosylation, the polyol pathway of glucose metabolism and direct glucose toxicity.
Since vascular endothelial cells are insulin-independent, glucose freely penetrates into the cells, causing their dysfunction. Non-enzymatic glycosylation of proteins, the conversion of glucose into sorbitol with the participation of the enzyme aldoreductase, the long-term and uncontrolled effect of glucose on the structure of cells in type 1 diabetes, associated with the activation of the enzyme protein kinase C, leads to an increase in the permeability of vascular walls and cell proliferation, accelerating the processes of tissue sclerosis, disruption of intraorgan hemodynamics [8].
Hyperlipidemia, which develops in type 1 diabetes, also contributes to the development of diabetic nephropathy. In type 1 diabetes, atherogenic low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL) cholesterol and triglycerides accumulate in the blood. Hyperlipidemia causes damage to the endothelium, glomerular basement membrane, and mesangial proliferation.
The formation of hypertension in type 1 diabetes is based on a sustained increase in intraglomerular pressure, which many authors associate with impaired tone of glomerular arterioles as a result of endothelial dysfunction. The effectiveness of NO decreases due to a decrease in its formation and an increase in its destruction, a decrease in the density of muscarinic-like receptors, the activation of which leads to the synthesis of NO, an increase in ACE activity on the surface of endothelial cells, which catalyzes the conversion of angiotensin I to angiotensin II, as well as the production of endothelin I and other vasoconstrictor substances . An increase in the formation of angiotensin II leads to spasm of effector arterioles and an increase in the ratio of the diameter of the afferent and efferent arterioles.
Angiotensin II plays a key role in the development of hypertension and renal failure. It has been established that the local renal concentration of angiotensin II is 1000 times higher than its content in plasma. The mechanisms of the pathogenic action of angiotensin II are due not only to its powerful vasoconstrictor effect, but also to proliferative, prooxidant and prothrombin activity. At the same time, angiotensin II has a damaging effect on other tissues in which its activity is high (heart, vascular endothelium), maintaining high blood pressure.
Prevention and treatment of hypertension in patients with type 1 diabetes consists of achieving optimal compensation of carbohydrate metabolism and correction of intrarenal hemodynamics. For this purpose, ACE inhibitors are used. These drugs are recommended to be prescribed at the stage of microalbuminuria (captopril, enalapril, ramipril, etc.) [9].
Metabolic syndrome
Metabolic syndrome (MS) unites a group of different diseases closely associated with type 2 diabetes. MetS is based on insulin resistance (IR) and hyperinsulinemia (HI). The most frequently combined components of MS are abdominal obesity, arterial hypertension and atherogenic dyslipidemia (increased triglyceride levels and decreased high-density lipoprotein cholesterol (HDL). According to some data, metabolic syndrome is detected in adolescents with up to 50% obesity.
Unlike subcutaneous fat, which makes up 75% of the body's total adipose tissue and is the main storage of lipids, abdominal fat is currently considered an independent endocrine organ. Its adipocytes synthesize a significant amount of various biologically active substances involved in the metabolism of glucose, fats, inflammation, coagulation, eating behavior, and regulation of vascular tone.
Abdominal obesity associated with MS is a key mechanism in the formation of hypertension. It turned out that adipose tissue ranks second after the liver in the formation of angiotensinogen. In obesity, adipocytes have increased renin content, ACE activity, significantly increased angiotensin II content, and increased expression of angiotensin II type 1 receptors (AT1 receptors). The activity of the tissue renin-angiotensin system is closely related to the production of adipokines by adipose tissue.
Impaired lipid metabolism leads to excessive fat deposition in tissues and decreased activity of enzymes involved in glucose metabolism. In the vascular endothelium, a protein kinase is activated, which inhibits the synthesis of nitric oxide.
On the other hand, IR leads to the development of compensatory hyperinsulinemia, which can maintain normal carbohydrate metabolism for a long time. The relationship between GI and hypertension is so strong that if a patient has a high concentration of plasma insulin, it is possible to predict the development of hypertension in the near future.
At high concentrations, insulin increases the activity of the sympathoadrenal system, the reabsorption of sodium and water in the proximal tubules of the kidneys, increases the proliferation of vascular smooth muscle cells, blocks the activity of Na+/K+-ATPase and Ca2+/Mg2+-ATPase, increasing the intracellular content of Na+ and Ca2+, which increases the sensitivity of blood vessels to the effects of vasoconstrictors.
Increased activity of the sympathetic nervous system with excess fat mass leads to an increase in cardiac output and heart rate, increased sodium reabsorption, and, in general, an increase in intravascular blood volume.
The reason for the development of IR is not clear. It is assumed that the development of peripheral IR is based on hyperactivity of the renin-angiotensin system. Angiotensin II in high concentrations competes with insulin at the level of insulin receptors (IRS 1 and 2), thereby preventing its action at the cellular level. On the other hand, the existing IR and GI activates the AT1 receptors of angiotensin II, leading to the implementation of the mechanisms for the development of hypertension.
So, in MS, the main role in the development of hypertension, cardiovascular complications and the progression of atherosclerosis is played by the high activity of the renin-angiotensin system. The treatment of MS is based on reducing body weight (see treatment of obesity) and increasing the sensitivity of receptors to insulin. For this purpose, biguanides are recommended (metformin (Siofor, Glucophage, etc.)), which inhibit the absorption of glucose in the intestine, inhibit the rate of its formation in the liver, and increase the number of glucose transporters in target cells [10].
Obesity
Hypertension is closely associated with overweight and obesity. In adolescents, this combination occurs in 30% of cases. The main reason for the increasing prevalence of obesity and its complications is the energy imbalance between excess energy intake in the form of foods and its expenditure as a result of reduced physical activity.
Primary obesity (constitutional-exogenous) is an independent neuroendocrine disease, depending on the disruption of the adipose-hypothalamic relationship. In this form, there is relative or absolute leptin deficiency on an alimentary-hypodynamic background.
The most common form of secondary obesity in adolescents is hypothalamic syndrome of puberty (pubertal-adolescent dyspituitarism). The essence of the disease is caused by dysregulation of hormones (liberins) by the hypothalamus, mainly by increased secretion of corticoliberin during puberty. At the clinic, patients complain of headaches, thirst, fatigue, and excess body weight. More common in females. Obesity with uniform distribution of fat. The skin has stretch marks of different colors. In girls, the menstrual cycle is often disrupted. The boys' faces are effeminate and their hair is sparse. Gynecomastia and stretch marks are often detected.
Hypertension in these forms of the disease is associated with hemodynamic changes: an increase in circulating blood volume, stroke and cardiac output with “inadequately normal” peripheral resistance. In the secondary form, it is aggravated by hyperproduction of ACTH and cortisol. Clinically, hypertension can manifest itself as a moderate increase in blood pressure; in some it increases to hypertensive crises.
The effect of treating obesity, metabolic syndrome and associated hypertension depends on the patient's motivation to change lifestyle, which involves increased physical activity and a reduced-calorie diet. Physical exercise has a positive effect on the emotional and psychological health of the individual. Physical activity promotes the consumption of large amounts of carbohydrates, the release of neutral fats from the depot, their breakdown and transformation. It must correspond to the age and individual characteristics of patients, providing increased energy consumption. These are morning exercises, walks, swimming, dancing, skiing and cycling, massage, etc. Physical activity should be of medium intensity, promoting increased consumption of carbohydrates and fats. It is recommended to limit the intake of salt, animal fats, and quickly digestible carbohydrates in food. To correct hypothalamic-pituitary disorders, drugs are prescribed that improve trophism and microcirculation (Cavinton, Nootropil, etc.). Of the antihypertensive drugs in this group of patients, it is preferable to use ACE inhibitors, since they have an organoprotective effect, as well as diuretics in small doses [9].
Read the end of the article in the next issue.
V. V. Smirnov1, Doctor of Medical Sciences, Professor M. D. Utev A. I. Morozkina
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information