Rendu-Osler-Weber disease is a disease with a clinical picture of hemorrhagic diathesis. The synonym “hereditary hemorrhagic telangiectasia” (HTH) fully reflects the essence of the disease, for which the most characteristic is a triad of signs: telangiectasia on the skin, mucous membranes and internal organs; tendency to bleed; autosomal dominant type of inheritance (A.A. Ponomarev, 1998; O.L. Ivanov et al., 2002).
The incidence of Randu-Osler-Weber disease is 1-2 cases per 1 million people. Anatomical and functional changes in blood vessels play a leading role in the pathogenesis of the disease. The anatomical essence of the disease lies in damage to blood vessels of various sizes with degeneration and hypoplasia of the muscular and elastic layers. As a result, focal thinning of the walls develops, followed by expansion of the lumen of microvessels. Bleeding is explained by the extremely slight vulnerability of the vascular wall at the site of angiectasia, as well as an increase in the fibrinolytic activity of the blood (V.B. Zolotarevsky et al., 1998; G.D. Babushkina et al., 2001).
Clinical signs of the disease are frequent nosebleeds, which occur spontaneously or after minor mechanical trauma. There are known cases of the onset of the disease with an attack of bloody vomiting and repeated gross hematuria. The development of telangiectasia in the liver can lead to the formation of chronic hepatitis and cirrhosis of the liver. There is only one report in the literature about the onset of the Randu-Osler-Weber disease, crying “tears of blood.”
Once started, bleeding is prone to recurrence, and the intensity and duration of bleeding varies from person to person (a single blood loss ranges from a few drops to 500 ml or more). In addition, the disease is also characterized by external manifestations in the form of multiple telangiectasias on the scalp, nasal mucosa, nasopharynx, larynx, digestive tract, genitourinary system, conjunctiva, bronchi, brain, liver, which can lead to serious complications - bleeding, iron deficiency anemia (E.V. Kazakevich et al., 1997; G.V. Banchenko et al., 2000).
In terms of the frequency of bleeding from internal organs during IGT, gastrointestinal bleeding comes first, followed by pulmonary and renal bleeding. Hemorrhages in the brain and spinal cord are observed in 2–3% of patients. Other neurological changes include headaches, epileptic seizures, paresis and visual disturbances (B. A. Berenbein et al., 1999; O. Braun-Falco et al. 1996; A. J. Keret, 2001).
As the disease progresses, chronic iron deficiency anemia develops due to repeated bleeding. In some cases, clear clinical manifestations of iron deficiency in the body develop (dry skin, brittle nails, hair). With generalized vascular damage, they speak of general varicose status.
Pathogenetic therapy for the disease has not been developed. For bleeding, conservative and surgical treatment methods are used.
In the literature, we have not found a description of combined lesions of the brain and spinal cord in Rendu-Osler-Weber disease, so this message will be of interest to practicing physicians. We present our own clinical observation.
Patient Shch., 48 years old, applied to the clinic of nervous diseases of Leningrad State Medical University on February 13, 2001 with complaints of rashes on the mucous membrane of the tongue, skin of the back, right foot and leg, frequent nosebleeds, dizziness, unsteadiness when walking, weakness in the upper and lower extremities, a feeling of numbness in the feet and legs, difficulty urinating in the form of frequent urges, decreased hearing in the right ear.
History of the disease.
Considers himself sick since preschool age, when short-term nosebleeds began to appear. At the age of 18 years, after another nosebleed, the patient consulted an otolaryngologist. An examination of the nasal mucosa revealed bleeding telangiectasias.
Family history.
Two sisters are sick with Randu-Osler-Weber disease; the eldest died at the age of 45 from profuse uterine bleeding, the youngest at the age of 44 developed profuse nosebleeds. Parents of the patient: mother, 72 years old, healthy; My father died at the age of 60 from a stomach tumor. There is no data on diseases in other generations. The patient has a daughter from her second pregnancy and is healthy. The first pregnancy ended in stillbirth at 7 months and was complicated by severe postpartum hemorrhage.
Anamnesis of life.
Denies sexually transmitted diseases, Botkin's disease, tuberculosis, malaria. There are no bad habits. Injuries and operations: concussion, resection of 2/3 of the stomach due to peptic ulcer. Somatic diseases include chronic pyelonephritis and chronic iron deficiency anemia.
Local status.
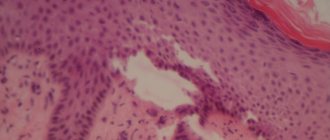
When examining the mucous membrane of the tongue, multiple telangiectasias are determined in the form of small irregularly shaped spots (Fig. 1), on the skin of the back, right leg and foot - many round and oval nodules with a diameter of 5–7 mm, protruding above the surface of the skin by 1–2 mm ( Fig. 2, 3), turning pale when pressed.
Somatic status.
Low nutrition, height 164 cm, weight 57 kg. When examining the back, there is a different position of the shoulder blades, a rib hump, and pronounced kyphoscoliosis of the thoracolumbar spine. There is vesicular breathing in the lungs, no wheezing, respiratory rate - 18 per minute. Heart sounds are muffled, heart rate is 80/min, blood pressure is 120/80 mm Hg. The abdomen is soft, painful in the epigastrium; the liver and spleen are not enlarged.
Neurological status.
Consciousness is clear. Percussion of the skull is painless. Palpebral fissures S > D, pupils S = D, single nystagmoid movements at extreme abductions of the eyes. The act of convergence on both sides is weakened. The right nasolabial fold is smoothed. Deviation of the tip of the tongue to the right. Hearing loss in the right ear. Tendon reflexes from the upper extremities are animated S>D, knee reflexes S>D, Achilles reflexes S>D, high polykinetic. Strength in the arms was reduced to 4 points, in the lower extremities - 3.5 points. The Jacobson-Weasel sign is positive on both sides. In the left lower limb, symptoms of ankylosing spondylitis, Rossolimo, Babinsky, and Poussep are detected. Articular-muscular sensation is clearly reduced in the left foot, slightly in the right. Left-sided hemihypalgesia. Decreased sensitivity of the polyneuritic type in the legs. Hyperesthesia of the radicular type D2–D8 on the right. Posterior ataxia in Romberg's position. The finger-nose test is satisfactory, the knee-heel test is more difficult on the left, pain in the occipital and cervical paravertebral points. Limitation of movements in the cervical spine. The gait is paretic-atactic with peroneal elements on the left.
1.General information
To the synonymous diagnoses listed in the title, you can add several more names that are often used to designate this disease, for example, Osler syndrome, Randu-Osler-Weber disease, hemorrhagic telangiectasia, etc.). All of them point to the most common type of hereditary vascular pathology: its essence lies in small-focal abnormal stretching and thinning of the capillary walls, which leads to the formation of multiple telangiectasia (vascular “stars”, dots, “meshes”, etc.) with a tendency to bleeding .
The epidemiological picture is characterized by extreme unevenness and territorial dependence. Thus, Randu-Osler disease is found in every two hundred of the inhabitants of the Netherlands Antilles, while in other regions of the world the incidence may not exceed 1:100,000.
What is known about the causes of the disease?
To date, the exact cause of the disease has not been clarified. A connection has been established with genetic mutations and the inheritance of altered genes according to the dominant type, if present in one of the parents. However, there are cases independent of inheritance; they are called sporadic.
Genetic studies have made it possible to identify 3 types of disorders:
- Type I - the gene responsible for collagen synthesis;
- Type II—defect of tumor growth factor receptors;
- Type III - has complex markings (600604, 12p11–p12; Â).
As a result, the main sources of bleeding are:
- foci of thinning of the walls of capillaries of the venous and arterial type;
- uncontrolled expansion of the diameter of microvessels;
- arteriovenous aneurysms.
The negative impact of infectious diseases suffered by the expectant mother in the first trimester of pregnancy and taking medications has been established.
Provoking factors for bleeding can be:
- lack of fortification of food, vegetarian diet;
- tight-fitting clothing that injures superficial vessels.
2. Reasons
To date, questions remain regarding pathogenesis. According to the most reasoned and generally accepted point of view, the characteristic clinical picture arises due to the abnormal, irregular structure of the tissues from which the walls of microvessels are formed at the stage of intrauterine development: they have practically no elastic muscle fibers, and the shell of the endothelial wall is connective tissue. With this composition, the vascular wall is fragile, vulnerable and unstable to stretching; it easily forms aneurysms and ruptures, which leads to bleeding.
Visit our Cardiovascular Surgery page
How does vascular deficiency manifest itself in internal organs?
Congenital defects in the structure of the walls of small vessels form characteristic arteriovenous aneurysms. Most often they are found in the lung tissue. Skin symptoms include:
- dyspnea;
- scleral injection;
- bluish-red complexion;
- polyglobulia - an increase in the number of red blood cells.
If aneurysmal dilatations of the capillary bed appear in the liver, kidneys or spleen, they are very difficult to diagnose. Most often, the disease is mistaken for tumors, tuberculosis of internal organs, erythremia, and congenital defects.
Long-term course of angiomatosis leads to:
- progressive pulmonary heart failure;
- chronic uremia;
- severe posthemorrhagic anemia;
- heart failure.
The changes are irreversible.
3. Symptoms and diagnosis
Despite the fact that the disease is genetically determined, it usually begins to manifest itself only after 6-8 years of life. The first visible telangiectatic lesions are usually localized on the lips, gums, wings of the nose, cheeks, and earlobes. Over the years, telangiectasias become more numerous, they appear in new areas and, in addition, their morphology changes: from small red dots to “cobwebs” and noticeably protruding bright red nodules. The hemorrhagic tendency also worsens with age.
A typical and one of the first symptoms of Randu-Osler disease is nosebleeds. Their intensity varies in different cases: from relatively short and meager to persistent and very long. In the history of medicine, cases of death from blood loss due to hemorrhagic telangiectasia have been recorded.
As vascular-wall incompetence progresses, telangiectatic foci can form not only on the mucous membranes and skin, but also on internal organs (brain, gastrointestinal tract, lungs, kidneys, etc.). Accordingly, even minor aneurysms or bleeding in this case become very dangerous: there is a high risk of developing severe anemia and fatal cardiovascular failure.
Diagnosis is based on studying the medical history (one of the key signs is frequent persistent bleeding) and family history (hereditary factor), as well as identifying characteristic telangiectasias. As a rule, they are visualized on the skin or mucous membranes during examination and leave no doubt, however, the likelihood of latent internal bleeding creates indications for prescribing endoscopic examinations. A general clinical blood test and a coagulogram are also required.
About our clinic Chistye Prudy metro station Medintercom page!
Intestinal angiodysplasia is the least studied intestinal disease, manifested by bleeding. This term combines a number of diseases that are based on the pathological development of blood vessels in different parts of the intestine. Possessing growth potential, angiodysplasia can turn into clusters of vessels or large vascular tumors such as cavernous angiomas at any period of life.
Histological examination of the surgical material makes it possible to detect conglomerates of thin-walled dilated veins filled with blood in the submucosal layer of the intestine, and multi-chamber cavernous vascular conglomerates in the subserous layer. Phleboliths are detected in the lumen of single dilated veins. Morphologically, cavernous, capillary and mixed forms of angiodysplasia are distinguished.
The occurrence of angiodysplasia is the result of a complex violation of embryogenesis of the vascular system. Injuries, infections, and hormonal disorders are secondary morphogenetic factors that contribute to their development during the intrauterine life of the fetus. The histogenesis of angiodysplasia is based on the excessive proliferation of endothelial cells while maintaining their main function - the lining of vascular tubes and cavities.
In accordance with the data of the State Research Center of Coloproctology (1995), three types of vascular lesions are distinguished [1]:
- Type I is a congenital form of angiodysplasia (hemangioma, or vascular hamartoma).
- Type II – acquired form (vascular ectasia).
- Type III – hereditary telangiectasia (Randu-Weber-Osler disease).
Congenital intestinal angiodysplasia is a rare disease [1, 3]. According to world literature, a little more than 500 cases of this pathology, confirmed histologically, are known. The age at which intestinal bleeding begins, its type, frequency, severity depend on the size, quantity and extent of vascular damage in the intestine [2, 4]. Most often, the first episodes of intestinal bleeding occur in childhood. However, isolated cases of manifestation of this disease at the age of 50–60 years have been described. The main clinical manifestation of intestinal angiodysplasia (up to 85% of cases) is frequently recurring painless intestinal bleeding at the time of defecation with a tendency to intensify in each subsequent case. Pain in the lumbar region, sacral region and lower extremities is also characteristic. Due to damage to the deep muscle layers of the intestinal wall, pain in the rectum may occur. In 10–15% of cases, intestinal bleeding with angiodysplasia is combined with complete or partial intestinal obstruction, caused either by obstruction of the intestinal lumen by conglomerates of affected vessels, or by intussusception [2, 11].
By location, the pathological process can be localized only in the large or small intestine or in the small and large intestine simultaneously. Very often, such vascular changes can be found on the skin in the form of hemangiomas of various sizes, but there are cases where there is no damage to the skin. The generalized form of cavernous hemangiomatosis belongs to the category of a rare pathology, and the combined lesion of the left half of the colon, rectum, left gluteal region with angiomatosis of the left lower limb (thigh, leg, foot), scrotum, penis - to the category of unique (Klippel syndrome - Trinone) [1, 3].
Impaired hemostasis and increased bleeding in this pathology are caused by platelet deficiency and a decrease in the level of serum fibrinogen [6]. A decrease in the number of circulating platelets may be the result of their increased destruction or pronounced aggregation in the vessels of the intestinal area affected by angiodysplasia. In addition, local coagulation in abnormal vessels causes fragmentation of red blood cells and can lead to microangiopathic hemolytic anemia with a large associated area of damage. At the same time, a decrease in the serum concentrations of coagulation factors V and VIII, responsible for the formation of thromboplastin, as well as fibrin, is often accompanied by increased fibrinolytic activity, which in turn can give rise to the development of consumption coagulopathy (disseminated intravascular coagulation - DIC syndrome) [ 7]. Daily blood loss is one of the criteria when developing indications for surgical treatment [5, 7]. If it exceeds 500 ml, it is an absolute indication for surgical intervention [1].
The acquired form of angioectasia is characterized by localization of lesions in the cecum and ascending colon. The causative factor in the development of this pathology is the adhesive process in the pelvis as a consequence of a previous inflammatory process or surgery on the pelvic organs [5, 9].
Rendu-Weber-Osler disease is a familial hereditary telangiectasia (hereditary hemorrhagic telangiectasia, or hemorrhagic angiomatosis), refers to hereditary diseases and is characterized by local dilation of small vessels, including venules and capillaries, as a result of their structural inferiority [5]. The disease manifests itself as hemorrhages, but coagulation and platelet hemostasis is not impaired.
This pathology was first described by HG Sutton (1864), and subsequently the information was supplemented by HJ Rendu (1896), W. Osler (1901) and FP Weber (1907). The etiology and pathogenesis of the disease have not been sufficiently studied; there are indications that the disease is transmitted in an autosomal dominant manner. Most patients have a heterozygous form; the homozygous variant is extremely rare. There are indications that local vasodilation occurs as a result of hereditary inferiority of the mesenchyme and disturbances in serotonin metabolism, but other researchers believe that telangiectasia are vessels newly formed from the remains of embryonic tissue. The generalized form of the disease is characterized by the location of telangiectasias on the mucous and serous membranes, skin, internal organs (lungs, liver, spleen, kidneys), and bones. Histological examination reveals sinus-shaped dilations of irregularly shaped vessels, the thinned walls of which are formed by endothelial cells and loose connective tissue.
The clinical picture is dominated by frequent profuse nosebleeds not associated with external causes, observed in 80% of patients. Less common are bleeding from the gastrointestinal tract, lungs, kidneys, urinary tract, hemorrhages in the brain, meninges, and retina. Telangiectasia can be detected in patients of any age, but most clearly manifests itself at the age of 40–50 years. They look like small (1–3 mm) flat, non-pulsating purple-violet formations that turn pale when pressed, often bleeding with minor mechanical damage. Telangiectasia can be localized on the mucous membrane of the nose, lips, gums, tongue, cheeks, on the skin of the scalp, face (especially on the wings of the nose and earlobes), limbs, trunk, as well as the conjunctiva and under the nails. Hypochromic microcytic iron deficiency anemia is characteristic, and after heavy blood loss - hypoplasia of erythroid elements of the bone marrow, reticulo- and thrombocytosis. Tests reflecting the state of coagulation and platelet hemostasis were not changed.
The disease is often combined with other vascular anomalies (aneurysms and angiomas in the lungs), leading to the formation of pulmonary arteriovenous anastomoses, which are radiologically detected in 15% of patients and their family members. The uniqueness of the clinical picture is the combination of symptoms of blood loss (anemia) and hypoxemia (cyanosis) due to the mixing of arterial and venous blood. When hypoxemia predominates, secondary erythrocytosis often develops. Cases have been described in which the disease was combined with arteriovenous anastomoses in the brain, retina, as well as with aneurysms of the hepatic and splenic arteries and aorta. Hepatomegaly with signs of liver cirrhosis (Osler cirrhosis) is detected in patients with extensive hemangiomatous lesions of the hepatic vessels.
Differential diagnosis of the above-described forms of intestinal lesions is carried out with inflammatory bowel diseases (ulcerative colitis, Crohn's disease), colon cancer, adenomatous polyps of the colon, and specific intestinal lesions.
We present data from our own observations of a patient with congenital intestinal angiodysplasia and a patient with Randu-Weber-Osler disease.
Patient O., 18 years old, was admitted to the gastroenterology department of MONIKI on 04/03/02 with complaints of increased bowel movements up to 5–7 times a day (daily volume up to 400 ml) mixed with blood and mucus, pressing pain in the lower abdomen, more pronounced in the right ileal region, worse before defecation, weakness, loss of appetite, rise in body temperature to subfebrile levels in the evening, weight loss of 17 kg over the past 2 months.
He became acutely ill on January 26, 2002, when, for no apparent reason, bowel movements became more frequent up to 6 times a day. I did not go to the doctors, I took chloramphenicol with furazolidone on my own for seven days. However, the patient's condition continued to deteriorate: blood appeared in the stool, and low-grade fever appeared in the evening. I contacted a therapist at my place of residence. To exclude the infectious nature of the disease, he was sent to the infectious diseases department of the district hospital, where the infectious etiology was rejected. With a diagnosis of “nonspecific ulcerative colitis,” on 02/14/02 the patient was transferred to the therapeutic department of the district hospital, where on 03/01/02 he underwent a colonoscopy (examination was carried out only up to the splenic angle): “The mucous membrane is pale, atrophic, the vessels are injected. Against the background of a pale mucous membrane, shallow ulcerative defects (single and in the form of clusters of 2-3-4), covered with fibrin, are found throughout the sigmoid colon and descending colon. Moderate hyperemia of the rectal mucosa.” The final diagnosis is “ulcerative colitis,” although the described changes in the mucous membrane of the colon are not entirely characteristic of this disease.
Treatment was prescribed: prednisolone 20 mg/day, sulfasalazine 3 g/day, gentamicin 240 mg/day, enzyme preparations, infusion therapy with solutions of electrolytes and proteins. During the treatment, the condition improved somewhat, but the frequency of bowel movements remained up to 5-7 times a day, and in the evening the body temperature continued to rise to subfebrile levels. To clarify the diagnosis and develop further management tactics, he was hospitalized in the gastroenterology department of MONIKI.
The condition upon admission was severe. Correct physique, sharply reduced nutrition. Height – 181 cm, weight – 48 kg. The skin and visible mucous membranes are pale and clean. Peripheral lymph nodes are not enlarged. There is no swelling. In the lungs there is vesicular breathing, no wheezing. The heart area is not changed, tachycardia is up to 95 beats/min, blood pressure is 100/60 mm Hg. Art. The tongue is moist with a slight white coating at the root. The abdomen is moderately swollen, painful on palpation in the lower parts, more in the right iliac region. The liver and spleen are not enlarged. Stool up to 3-4 times a day, volume up to 300 ml, mixed with blood and mucus. The urinary system is unremarkable.
In blood tests: hemoglobin – 110 g/l, erythrocytes – 3.75 × 1012/l, color index – 0.87, leukocytes – 33.5 × 109/l (band cells – 24.5%, segmented cells – 38%, eosinophils – 0.5%, basophils – 2%, lymphocytes – 20%, monocytes – 14.5%), ESR – 40 mm/h, slight anisocytosis and poikilocytosis. Bilirubin – 8 µmol/l, cholesterol – 3.0 mmol/l, total protein – 70 g/l, thymol test – 1.8 units/l, glucose – 3.4 mmol/l, potassium – 3.2 mmol/ l, sodium – 134 mmol/l, ALT – 8 units/l, AST – 14 units/l, alkaline phosphatase – 318 units/l,
gamma-GPT – 39 U/L, serum iron – 3.5 µmol/L.
Coagulogram: prothrombin index - 94 (normal - 100%), thrombin time - 27 (normal - 28-30 seconds), fibrinogen - 3.8 g/l, factor XIII activity - 97%, fibrinolytic activity - more than 200 minutes, ethanol and betanaphthol tests are weakly positive.
Coprogram: stool of mushy consistency, creative rhea.
A general urine analysis revealed no pathology. Urine amylase – 30 (normal – 0–350 units/l).
Sigmoidoscopy: The perianal area is not changed, the examination was carried out at 12 cm. The mucous membrane is pale, the vascular pattern is clearly visible, there is no contact bleeding. In the lower ampullary section there are 2 linear ulcers up to 0.8 cm long, covered with fibrin. There is a fissure in the anal sphincter covered with fibrin. The sphincter is hyperemic, two hemorrhoids are purple in color.
Based on complaints of frequent stools up to 6–7 times a day mixed with blood, pain in the lower abdomen, more pronounced in the right iliac region, evening low-grade fever, acute onset of the disease, and examination of the rectal mucosa, a diagnosis was made: “Crohn’s disease.” , 1st attack, severe course with possible localization in the ileum, colon or combined localization (small and large intestine).
In accordance with the diagnosis, treatment was prescribed: methylprednisolone 500 mg/day intravenously, 0.5% metronidazole 300 ml/day intravenously, cefazolin 3 g/day intramuscularly; infusion therapy: 400 ml of 5% glucose solution intravenously by drip with simultaneous administration of potassium preparations (panangin 10 ml, 4% KCl solution), ascorbic acid 10 ml, co-carboxylase 100 mg, hemodez 400 ml/day, albumin 100 ml/day; enzyme preparations (Creon 6 drops/day); drug for parenteral nutrition.
On the 3rd day (04/05/02) of the patient’s hospital stay, an objective examination revealed intestinal obstruction. Radiologically it was confirmed by the presence of small-colic obstruction. From this moment until the patient was transferred to the surgical department, intermittent intestinal obstruction persisted. The first intestinal bleeding occurred on 04/07/02 – on the 4th day of the patient’s hospital stay, when the stool took on the appearance of “raspberry jelly” in a daily volume of about 400 ml. The patient is examined by a surgeon. It was decided to intensify infusion therapy with the introduction of electrolyte-protein mixtures and fresh frozen plasma with a total volume of up to 3 liters. The daily stool volume ranged from 350 at the time of admission to 700–800 ml in the form of “raspberry jelly” with repeated intestinal bleeding. Due to the severity of the condition, it was not possible to conduct an examination of the large and small intestines. An esophagogastroduodenoscopy was performed, which revealed an ulcer of the upper wall of the duodenum with severe perifocal edema and an inflammatory shaft. Ultrasound examination of the abdominal organs revealed uneven dilation of the intestinal loops; no pathology was detected in the parenchymal organs.
On April 22, 2002, the patient developed hemorrhagic rashes on the skin of the legs, in the area of the knees, and on the anterior wall of the abdominal cavity. In the general blood test: hemoglobin – 180 g/l, erythrocytes – 5.66 × 1012/l, leukocytes – 6.6 × 106/l, ESR – 1 mm/h. From that moment on, the patient's condition was regarded as extremely serious. With a diagnosis of Crohn's disease, a hormonally resistant form, the first attack, complicated by recurrent intestinal bleeding, partial small-colic obstruction and disseminated intravascular coagulation, the patient was urgently transferred to the abdominal surgery department.
After intensive preoperative preparation (glucose-electrolyte-protein mixtures in a total volume of up to 3.5 l, pefloxacin 800 mg/day, methylprednisolone 250 mg intravenously, famotidine 40 mg/day, nadroparin 0.3 ml subcutaneously), the patient underwent a subtotal colectomy within apparently changed section of the intestine - 29 cm of the ileum and the entire colon to the lower ampullary part of the rectum were removed with the application of an ileostomy according to Brooke.
On macroscopic examination: the large intestine is 80 cm long with a segment of the ileum 18 cm long. The small intestine is 3 cm in diameter, the relief of the mucous membrane is not changed. Colon diameter ranged from 5 to 7 cm; over a large area, the intestinal wall is thickened, compacted, the mucous membrane is lumpy with multiple ulcerative defects of irregular shape, in places merging with each other, and areas of a dark red color. Resection was performed within the unchanged mucous membrane (Fig. 1).
Microscopic examination: the changes correspond to diffuse angiodysplasia of the colon with the presence of multiple angioectasia and cavernous microhemangiomas in the submucosal layer, extending in places to the muscular plate propria (Fig. 2).
Changes in the mucous membrane are secondary in nature, localized over clusters of well-formed vessels: multiple subacute and chronic erosions, flat ulcers, dysregenerative restructuring of the crypts (Fig. 3 and 4).
The postoperative period was uneventful, but the patient's condition remained severe due to persistent signs of disseminated intravascular coagulation. General blood test in the postoperative period: hemoglobin – 74 g/l, erythrocytes – 2.55 × 1012/l, color index – 0.87, leukocytes – 7.8 × 109/l (band cells – 12%, segmented cells – 57% , lymphocytes – 25%, monocytes – 6%, platelets – 170.8 × 109/l), ESR – 22 mm/h. Indicators of the coagulation system: coagulation time - 65 (normal - 70-80 seconds), tolerance to plasma heparin - 35 seconds (normal - 5-8 minutes), prothrombin index - 88 (normal - 90-105%), plasma fibrinogen - 2 .6 (norm – 2–4 g/l).
The patient received massive infusion therapy (glucose-potassium mixture 400 ml, etamsylate 800 mg dissolved in 200 ml of physiological solution, rheopolyglucin 400 ml, aminosteril 500 ml, pefloxacin 400 mg × 2 times a day intravenously). On the 12th day, the wound healed by primary intention, the sutures were removed, and the ileostomy functioned normally.
On the 34th day after the operation, the patient was discharged in a stable condition of moderate severity for follow-up treatment on an outpatient basis under the supervision of a surgeon at the place of residence with recommendations for frequent fractional meals. Additionally, enzyme preparations (Creon, pancitrate) are recommended, 1-2 capsules with meals, taking iron supplements, limiting physical activity.
The presented observation indicates the difficulty of diagnosing colon angiodysplasia due to the similarity of some of its clinical and morphological manifestations with inflammatory and tumor diseases. Characteristic signs of the disease are most often detected during fibrocolonoscopy [11], the effectiveness of which is determined by the qualifications and experience of the endoscopist. Areas of the affected intestinal walls appear as polypoid dark purple formations, often with a bluish tint, protruding into the intestinal lumen. This picture corresponds to the cavernous type of angiodysplasia. Upon surface contact, slight bleeding occurs. In the capillary form, these signs are less pronounced. In the affected area, smoothness of the mucous membrane is noted [8]. It is bluish in color or slightly hyperemic with areas of thickening or sharply contoured, dilated, tortuous vessels. Almost always there is a clear border with the unchanged mucous membrane of the colon. Biopsy is not recommended in patients with congenital angiodysplasia of the colon due to the risk of significant bleeding. When irrigoscopy using the double contrast method, multiple filling defects, eroded contours with obligatory distortion of the submucosal layer of the intestine, as well as multiple atypically located pelvic phleboliths are detected [10].
Our other observation also relates to a rare pathology of the development of the vascular system of the intestinal wall, such as the Randu-Weber-Osler syndrome.
Patient Z., 18 years old, was admitted to the gastroenterology department of MONIKI on July 10, 2001 with complaints of progressive weakness, dizziness, rapid heartbeat, shortness of breath, loose stools mixed with a large amount of dark blood.
She became acutely ill on 07/04/01, when severe weakness, nausea, vomiting of eaten food appeared, then profuse loose stools mixed with dark blood. Body temperature did not significantly increase. She was hospitalized in the infectious diseases department at her place of residence by ambulance, where on 07/05/01 vomiting and loose stool mixed with blood reappeared. The diagnosis of intestinal infection was rejected, and anemia was detected (hemoglobin - 44 g/l). The patient was transferred to the intensive care unit of the surgical department at her place of residence, where sigmoidoscopy revealed a rectal ulcer at a distance of 7–10 cm from the anus. Hemostatic (erythrocyte mass, protein), antibacterial and steroid therapy was carried out. The patient's condition progressively worsened. Anemia persisted. There were no bowel movements for the next four days. To exclude ulcerative colitis, the patient was transferred to the gastroenterology department of MONIKI.
Upon admission, the patient's condition was assessed as extremely serious. Increased nutrition, puffy face, pasty lower extremities. Pronounced pallor of the skin. Peripheral lymph nodes accessible to palpation are not enlarged. Tachycardia up to 110 beats/min was noted, blood pressure was 130/60 mmHg. Art. The abdomen is soft and painless on palpation, there are no symptoms of peritoneal irritation. The liver and spleen are not enlarged. No pathological changes in the lungs or urinary system were detected.
The patient's heredity is not burdened; there are no indications of vascular pathology in close relatives.
A study of peripheral blood revealed anemia (hemoglobin - 35 g/l, red blood cells - 1.45 × 1012/l), thrombocytopenia (87 × 109/l), leukocytosis (12 × 109/l), accelerated ESR (70 mm/h ), shift of the leukocyte formula to metamyelocytes (1%), anisocytosis, poikilocytosis, anisochromia, erythronormoblasts were detected - 4: 100. ECG - metabolic changes in the myocardium of the left ventricle.
The patient was examined by a hematologist, hemolytic anemia and crisis were diagnosed; Consulted by a neurologist - hypoxic encephalopathy due to severe anemia. An intravenous infusion of 200 ml of red blood cells was performed, and 100 mg of metronidazole was administered. During sigmoidoscopy, dark, pasty fecal contents were found in the ampulla of the rectum.
Examined by an abdominal surgeon. Gastrointestinal bleeding was diagnosed. Transferred to the abdominal surgery department.
Colonoscopy was performed on July 11, 2001 (examination up to the upper third of the sigmoid colon, but it was not possible to go further due to the large amount of unremovable hemorrhagic contents). Linear ulcers of the mucous membrane up to 6–7 cm in length and up to 1 cm in width with fibrin overlay were found. The ulcers are superficial with diapedetic bleeding from the edges. A detailed examination is not possible due to ongoing bleeding. Conclusion: Ulcerative colitis? Crohn's disease?
At the consultation, a fulminant form of nonspecific ulcerative colitis was diagnosed, complicated by intestinal bleeding and toxic dilatation; a decision was made on urgent surgical intervention.
Laparotomy was performed on July 11, 2001. During revision of the abdominal cavity, a pronounced dilatation of the proximal colon to the middle third of the sigmoid colon was noted, in the lumen of which there were blood clots. The loops of the colon are bluish in color, the serous layer is not shiny. The mesentery of the colon is slightly edematous, with multiple enlarged soft lymph nodes. The small intestine is not changed, there is no blood in its lumen. No other abdominal pathology was found. A subtotal colectomy was performed to the level of the lower third of the sigmoid colon with resection of the ileum (15 cm) and the appendicular process. An ileostomy was performed.
Esophagogastroduodenoscopy from 07/12/01 – secondary anemia of the mucous membrane of the esophagus, stomach and duodenum. Repeated examination on July 19, 2001 – hemorrhagic duodenitis due to anemia of the mucous membrane.
Morphological examination of the intestine: on the section, the intestinal lumen is filled with bloody masses, the appendix is thickened, deformed, the intestinal wall is deformed, areas of narrowing alternate with those of expansion and thinning. In the narrowing zone there are deep recesses like ulcers. There is no histological evidence for nonspecific ulcerative colitis. Noteworthy is the abundance of clusters of malformed vessels of the sinusoidal type (angiectasia), as in Randu-Weber-Osler disease. These formations are located in the submucosal layer of the large and small intestines, and in some places in the lamina propria of the mucous membrane. Conclusion: pathology of the development of the vascular bed of the intestinal wall according to the type of Randu-Weber-Osler syndrome.
Coagulogram: increased fibrinogen content to 5.3 (normal – 2–4 seconds), positive betanaphthol test.
In the postoperative period, an increase in body temperature to 38 °C and relapses of intestinal bleeding (discharge from the ileostomy up to 1600 ml/day) were noted on the 3rd, 8th and 12th days after surgery.
Intensive infusion therapy was carried out, including blood transfusions: 6.53 liters of single-group blood, 2 liters of red blood cells, 3 liters of plasma, 150 ml of cryoprecipitate. The following were administered intravenously: methylprednisolone 500 mg/day, famotidine 40 mg/day, metronidazole 300 mg/day, cefaxone 4 ml/day. The volume of injected fluid is up to 3 l/day.
During therapy, the condition stabilized, no relapses of bleeding were observed, peripheral blood parameters normalized: hemoglobin - 116 g/l, erythrocytes - 3.99 × 1012/l, leukocytes - 9.8 × 109/l, ESR - 16 mm/h. On the 37th day, the patient was discharged in relatively satisfactory condition for outpatient follow-up treatment at her place of residence.
Despite the differences in the etiological factors that led to the development of these diseases, morphological changes in the affected parts of the intestine, the treatment approaches in these two cases turned out to be identical - radical excision of the affected areas of the intestine with preservation (where possible) and restoration of the function of the altered organ. In the future, the prognosis for life in most cases is favorable. However, it should be noted the possibility of repeated bleeding from parts of the intestine that were intact during the operation (spread of the pathological process). Deaths from rebleeding are rare.
4.Treatment
The primary goals are to prevent dangerous hemorrhages and relieve anemia; in some cases, blood transfusions are prescribed for this purpose. For a long time, nasal tamponade was considered the therapeutic standard for Randu-Osler disease, but now more and more specialists are abandoning this method, finding a lot of shortcomings in it and low efficiency. Today, among the therapeutic agents used are irrigation with a solution of aminocaproic acid, various coagulation techniques (cryo-, electro-, laser) and artificial embolization of the most problematic arteries. The presence of large aneurysms often forces them to resort to surgical removal.
Patients with hereditary hemorrhagic telangiectasia have to follow a special diet and take all precautions to avoid injury to bleeding and potentially dangerous lesions.