History of Hijama Practice
This method of treatment has been around for many thousands of years. Even ancient Greece, Egypt and China used hijama for treatment.
In 1550 BC There is a mention of cupping therapy in the oldest medical textbook, the Ebers Papyrus.
From Arabic, the word “hajma” is translated as “to suck.” After all, the process involves “sucking” blood by creating a vacuum. First, small incisions are made on the skin with a sharp instrument, and then they begin to pump air out of the cans, causing blood to come out.
Fever and fashion for leeches
Since excess blood was considered the cause of overheating and intensification of the fiery principle, bloodletting was a way to “ventilate the veins” and “cool” the hot body. It was considered indispensable for fevers: these included many diseases accompanied by fever, rapid pulse and heartbeat - from colds to inflammation of internal organs. This connection between symptom and treatment was extremely stable. At the beginning of the 19th century, the French military doctor and physiologist Francois Broussais preached bloodletting as a panacea for fevers and inflammations FJV Broussais. Histoire des phlegmasies ou inflammations chroniques fondée sur de nouvelles observations de clinique et d'anatomie pathologique: avec leurs différentes méthodes de traitement. Paris, 1808., and Brousse attributed almost all diseases to inflammation, including scurvy and cholera, new to France. Making a concession to the sensitivity of his patients, instead of a painful lancet and cups, Brousse used leeches - a person almost does not feel their bite. This is how a 30-year-old fashion for leeches arose in Europe, the damage from which was compared by caustic contemporaries to the Napoleonic Wars. The leeches themselves also suffered: by the 1830s, the worms of the Hirudo medicinalis variety in Western Europe had practically run out, and they had to be imported.
Leeches. Illustration from the book “Physica sacra” by Johann Jacob Scheichzer. 1731–1733 Wellcome Library, London
Kinds
- Dry hijama. The procedure is carried out without making any incisions on the skin.
- Massage room. Similar to the first method, but also adds olive or black seed oil to make the jars slide easier.
- Bleeding. The oldest type of this procedure. The vessels are installed on specific areas of the body that have different functions for the body.
- Herbal. The herbal decoction or tincture is poured into a jar and applied to the skin.
- Water. The most ineffective type of hijama. Warm water is poured into the jar, the cotton wool is set on fire and the jar quickly sticks to the skin, ideally, without spilling a single drop.
Answers to questions about the medicine of the Prophet Muhammad
Did Prophet Muhammad bleed himself or invite a doctor?
He invited a doctor, both for himself and for others [16]. Bloodletting is a very difficult procedure. Carrying it out on your own is not only undesirable, but also dangerous. And the Holy Quran says: “Do not throw yourself into danger with your own hands!” (see Holy Quran, 2:195).
Is it possible to do bloodletting while fasting?
It is reliably known that the Prophet Muhammad performed bloodletting during fasting. In the collection of hadiths of Imam al-Bukhari, the following hadith from Ibn 'Abbas is given: “The Prophet (peace and blessings of Allaah be upon him) did bloodletting while fasting” [17].
Is it possible to do bloodletting, but the fast is not broken?
According to the overwhelming majority of Islamic theologians, no, it is not violated [18].
Do I need to wash after bloodletting?
No. Only a few scholars have stipulated the desirability of performing a complete ablution after bloodletting [19].
Is it possible to somehow thank the person who performed the bloodletting?
Can. The Prophet Muhammad always tried to thank the person who bloodletted him [20]. For example, when Abu Taiba bled the Prophet, he thanked him with approximately seven [21] kilograms of food [22]. Of course, the form of gratitude is not limited in any way [23].
At the same time, this fee is not mandatory. The doctor may refuse remuneration.
Are there any guidelines regarding the age of the person undergoing phlebotomy?
The older the person, the less frequently this medical procedure should be performed. For example, Imam at-Tabari [24] reported the following words of Ibn Sirin [25]: “After forty years a person does not need to do bloodletting.” At-Tabari explained: “After forty years, the human body begins to weaken. Therefore, performing this procedure becomes possible only under significant circumstances and taking into account how familiar bloodletting is for a given person.” Scientists also recommended completely abandoning this procedure by the age of eighty [26].
Are there differences between blood donation, which is common today, and bloodletting?
There is a difference. At least in the fact that bloodletting is done for certain diseases and ailments, in certain parts of the body and preferably on certain days.
Advantages and disadvantages
With a large amount of blood taken, it begins:
- Immunity decreases;
- The volume of incoming oxygen decreases;
- Stimulate the bone marrow.
All this does not really affect the general condition of a person. The greatest harm is observed if the procedure is performed by an inexperienced specialist.
If everything is done according to the rules, the body will be freed from stagnant fluid with toxins, and the blood will be renewed. Thanks to irritation of nerve endings, the spinal cord receives signals that activate a certain segment.
When the body gets rid of some of the blood, a reserve mechanism is activated, which restores the desired level and cures various diseases and reduces pain. Hijama is also used for prevention. If everything is done correctly, then such training will be very useful for the body.
Blood
The human body contains several liters of blood: women have an average of about four liters, men - a little more than five. Some of the blood moves through blood vessels - arteries and veins, while some is found in tissues and hematopoietic organs. Blood is vital, and significant blood loss leads to weakness and anemia, followed by oxygen deprivation, hemorrhagic shock, deterioration of the heart and internal organs, and death. Therefore, there are a number of serious restrictions for blood donation, and the upper norm for one blood donation is limited to 8–10% of total volume (that is, no more than 400 ml). In general, a free lunch, a glass of wine and a day off for a donor are not without reason. In modern medicine, bloodletting, or, more precisely, phlebotomy - taking blood from a vein with a needle - is used only occasionally. Among the indications are hemochromatosis (a disorder of iron metabolism), polycythemia vera (an increase in the number of red blood cells, which increases blood viscosity and impairs its circulation) and skin porphyria tarda (a disorder of pigment metabolism, expressed, in particular, into intolerance to sunlight). Recent studies discuss the possible benefits of phlebotomy in sickle cell disease and Alzheimer's disease BE Dwyer, L. R. Zacharski, D. J. Balestra, A. J. Lerner, G. Perry, X. Zhu, M. A. Smith. Getting the Iron Out: Phlebotomy for Alzheimer's Disease? // Medical Hypotheses. Vol. 72. No. 5. 2009., but now not a single doctor will recommend restorative bloodletting for gout, flu or depression.
Contraindications
If they are not taken into account, side effects may occur. Hijama is strictly contraindicated for:
- Low hemoglobin;
- Hypotomy;
- Heart disease;
- Low concentration of red blood cells and platelets;
- Asthenia;
- Ages up to 20 and after 70 years;
- Severe mental illness;
- Pregnancy;
- Cerebral atherosclerosis;
- Arterial hypotension;
- Hepophilia;
- Cirrhosis of the liver.
Also, as temporary contraindications:
- Injury or surgery (less than 21 days ago);
- Poisoning;
- Viral or colds (less than 14 days ago);
- Menstruation.
Mesmerism or animal magnetism
A pseudoscientific medical theory developed in 1773 by Austrian physician Franz Mesmer claimed that all humans possess “animal magnetism.” Allegedly, there is some invisible fluid that permeates the entire universe and man, and in man it makes itself felt most clearly.
Franz Mesmer
Mesmer did not know how to present this theory, and settled on the formulation “magnetic fluid.” The human body is a magnet, and the magnetic force can be somehow directed in the human body and used for healing. The treatment sessions were something between hypnosis and magnetotherapy.
The doctor practiced in Vienna and was successful until a scandal erupted around his treatment and he was declared a charlatan. Mesmer did not give up, but moved his practice to France, where it gained amazing popularity. “Animal magnetism” was successfully integrated into the scientific and philosophical paradigm of the Enlightenment; in addition, it was promoted through Masonic lodges, and therefore was picked up by the social movement. Dr. Mesmer, with the support of Queen Marie Antoinette, founded the Institute of Magnetism, where he organized entire performances with collective therapy sessions. Patients were treated by immersion in magnetized water while their hands held wires leading to "magnetized" trees. All this took place to the accompaniment of a piano or harmonica. Mesmer had many high-ranking and respected patients, such as the banker Cornman and the Marquis de Lafayette, who spoke glowingly of his therapy.
Mesmerism successfully exploited the general interest in the recently discovered phenomena of electricity and magnetism, as well as esoteric practices, and therefore managed to leave a noticeable mark on the medical theory and practice of France during the Enlightenment.
Impressive, exalted patients often fell into a convulsive state during the sessions, which enhanced the impression of this show. The therapy sessions had more affinity with the occult than with medicine. Participants declared that they had discovered paranormal abilities. Religious philosopher Helena Blavatsky wrote: “Mesmerism, or animal magnetism, will become an accepted science, and history will publicly condemn generations of stubborn doctors who sacrificed millions of suffering contemporaries to their wild vanity and obstinacy.”
Still from the film "Mesmer", 1994
At the same time, mesmerism was severely criticized by the medical community, and Franz Mesmer himself began to wander around Europe, settling in the cantons of Switzerland and then returning to France, but his teaching gradually lost public support. Not for long, really. Inspired followers revived the doctrine of “magnetic fluids” at the beginning of the 19th century in the wake of romanticism, and it took the form of spiritualism and therapeutic hypnosis.
Despite all the obvious unscientificness of this medical theory, it is still popular. You can learn mesmerism for 90 thousand rubles. There are also more budget-friendly options - tutorials on mesmerism, magnetism and bioenergy.
Scheme of points on the body for the procedure
The areas where the banks are installed are located exactly where energy accumulates. Not many people know, but energy flows are located along the meridians. These channels can become clogged and, as a result, health will deteriorate. Pressing on certain points may cause pain.
Since ancient times, China has used massage of these points and areas to stimulate the proper functioning of energy flows. There is a certain “tsun” method - it is thanks to it that you can calculate the necessary points. Unfortunately, this procedure is quite complex and time-consuming. But since hijama jars are quite large in size, it is more likely to hit the right spot.
How often can this procedure be done?
It is best to initially conduct a course of detox and boost immunity. Since this method is used for both prevention and treatment, hijama should be used no more than 2-4 times a year, if health is good. If there are serious diseases, then the procedure should be performed more often.
Different techniques for certain diseases
Chinese technology is used for:
- Acne;
- Gastrointestinal disorders;
- Hearing loss;
- Conjunctivitis;
- Epilepsy;
- Convulsions;
- Asthenia;
- Hypertension;
- Migraines, etc.
Islamic methodology is effective for:
- Varicose veins;
- Allergies;
- Prostatitis;
- Do not lie;
- Insomnia;
- Hemorrhoids;
- Impotence;
- Depression, etc.
There is also the Tibetan system, which is very similar to the Chinese one. A small incision in the vein activates the hemostasis system. This technique is appropriate when:
- Edema;
- Lymphangioma;
- Infectious lesions;
- Wounds or injuries;
- Gout.
For stroke, European bloodletting is often used when there is intolerance to certain medications. This method eliminates death and pathology.
What tools are used for hijama?
Different techniques use different devices. Either needles or small blade-like knives are used to make the cut. For the Tibetan system, a special hatchet is used - hanuur, similar to a razor.
Jars for the procedure are cylindrical in shape. They are made of plastic and have a diameter of 2-7 cm. A special pump is also needed, which pumps out the air from the jars. All instruments are sold at the pharmacy.
Where exactly were the incisions made, and in what cases?
“The Prophet Muhammad did bloodletting in the upper back between the shoulder blades and on the neck” [11];
Al-Bukhari's collection of hadiths states that “The Prophet used to let blood on his head [12]” [13]. Another hadith clarifies that this was done to alleviate the condition of a severe headache [14].
I think the words of Ibn Qayyim al-Jawziya will be useful here: “The Prophet Muhammad (peace and blessings of God be upon him) performed bloodletting in different parts of the body. Everything depended on the circumstances, on necessity and need” [15].
Why might you feel unwell after hijama?
The person may feel weak, dizzy, or even lose consciousness. Most often this happens due to fear of the procedure itself and a large accumulation of toxins. This condition will definitely go away after some time.
There is also a high temperature, which may mean that the body has started recovery processes. Symptoms of diseases may worsen, but there is nothing to worry about - the body heals.
Most often, if a person’s condition has not changed in any way after hijama, it means that the points were chosen incorrectly and it is necessary to repeat the procedure.
From the history of blood transfusion to humans for therapeutic purposes
IN
The history of blood transfusion distinguishes two main periods. The first period is from ancient times until the discovery of the laws of isohemagglutination and group blood factors (erythrocyte antigens). In this period, two stages can be distinguished: the first - from ancient times to the discovery of blood circulation by W. Harvey (1628); the second lasted until the discovery of group blood factors by K. Landsteiner (1900). The ancient Roman physician and naturalist Galen put forward a theory of blood circulation, which had a great influence on the development of medicine in the Middle Ages. Hippocrates believed that blood could change the mental properties of a patient and therefore recommended drinking blood to patients suffering from a number of diseases with mental disorders. Ovid Naso writes in his Metamorphoses about the healing properties of blood. 15 centuries after Ovid, we find the same indications about the healing properties of blood from one Medici court physician in Florence.
Dispensary in the time of Galen
In 1498, a blood transfusion was performed on the decrepit and sick Pope Innocent. “The doctor took the blood of three ten-year-old boys who died soon after, prepared a medicine from this blood chemically and gave it to the pontiff to drink for his health.” Dad's treatment ended in complete failure. Dad died despite the fact that three children were sacrificed to him. The doctor escaped.
In the Middle Ages, bloodletting was widely used in Europe, the victim of which, for example, was the brilliant Italian artist Raphael Santi. Only in 1527 did Paracelsus decisively speak out against the “misconceptions of bloodletting calendars.” A.A. Bogomolets wrote: “The idea of restoring the fading forces of the body by transfusing the blood of a healthy person, which came to us from ancient times and was discredited by unsuccessful attempts at practical application at the end of the 18th century, has recently acquired absolutely exceptional interest.”
Medical procedure in the Middle Ages
In the writings of Hippocrates there is a mention of the use of the blood of healthy people to treat the sick. In the Middle Ages and at the dawn of the Renaissance, blood transfusions into human vessels were not used. Based on the ideas about the movement of blood in the body that existed before the discovery of W. Harvey, blood transfusion could not receive a correct theoretical justification and rational practical application, although doctors in Italy and France spoke about the possibility of intravascular infusion of blood to a person. W. Harvey's discovery marked the beginning of a scientific approach to the problem of blood transfusion. About the significance of this discovery I.P. Pavlov wrote: “...Among the deep darkness and now difficult to imagine confusion that reigned in ideas about the activities of animal and human organisms, but sanctified by the inviolable authority of the scientific classical heritage, the doctor William Harvey spied one of the most important functions of the body - blood circulation and thereby laid the foundation for a new department of precision human knowledge – animal physiology.” Harvey first outlined his views on blood circulation in a lecture he gave in 1615 in London. In 1628, he published the work “An Anatomical Study on the Movement of the Heart and Blood in Animals,” in which he refuted Galen’s teaching about the movement of blood in the body that had existed for 1500 years and formulated new ideas about blood circulation. These ideas were supplemented by the outstanding Italian biologist and physician Marcello Malpighi, one of the founders of microscopic anatomy. Malpighi's most important achievement was the discovery of capillary circulation in 1661. Harvey had one weak spot in his teaching - the “Achilles heel” of his entire theory: he could not show how blood from the artery enters the veins.
Following Harvey's discovery, new methods of drug administration appeared - injections and infusions, which played an important role in practical attempts at blood transfusion. The technique of infusion into the bloodstream was developed experimentally by Harvey's students. They also came up with the scientifically based idea of blood transfusion.
Experimental work on blood transfusion in the 17th century. were carried out by English naturalists: K. Potter (1638), J. Clark (1657), F. Cox (1665), B. Lower (1666), French - A. Burdelot (1667), R. Gabe (1667), J. Denis (1667), Italian – G. Casini (1668), I. Magnani (1668), German – D. Major (1667), M. Etmuller (1682), B. Kaufmann (1683), M. Purmann (1684) .
London anatomist Richard Lower experimented with blood transfusion on animals. In 1666, he transfused blood to a dog: he released blood from its jugular vein, brought the dog into convulsions, and infused it with the blood of another dog. A few hours later the dog came to life and behaved as usual.
The first blood transfusion was performed by Jean Baptiste Denis. Having become acquainted with Lower's materials, in the same 1666, with the help of the surgeon Emerlen, he repeated the experiments on dogs, and a year later, in 1667, he transfused the blood of a lamb to several patients. On June 15, 1667, he infused a feverish patient with 9 ounces of lamb's blood directly from the carotid artery into a vein in his arm. The experience ended successfully.
Bloodletting in the 16th century
The results of the first blood transfusions were encouraging. However, the fourth transfusion to another patient ended 2 months later with his death. Human blood transfusions were stopped for almost a century.
In 1795, the German clinician Christoph Hufeland wrote in his work “The Art of Prolonging Human Life, or Macrobiotics”: “There was a time when blood was so little valued in France that King Louis XIII was bled 47 times in the last 10 months of his life... Meanwhile, through the opposite process, through the infusion of fresh young blood into the veins, they wanted to rejuvenate and prolong a person’s life and heal from diseases. This method is called blood transfusion..."
The failures of heterogeneous blood transfusions led to the idea of transfusions of only human blood. In 1819, the English physiologist and obstetrician J. Blundell performed the first human-to-human blood transfusion and proposed a special apparatus for blood transfusions. Soon the French parliament banned blood transfusions altogether. But despite this, at the end of the 17th and beginning of the 18th centuries, scientists energetically sought ways to scientifically substantiate blood transfusions from person to person. For the period from 1820 to 1870. In the world literature, a total of 75 cases of blood transfusion were reported.
One of the most striking pages in the history of blood transfusion was written by Russian medical scientists.
In Russian literature, the first proposals for blood transfusions for patients appeared in the works of Professor of the Kronstadt Medical School Matvey Peken (1787) and Professor of the Medical and Surgical Academy in St. Petersburg S.F. Khotovitsky (1830). In 1832, G. Wolf transfused blood to a woman who was dying after childbirth from uterine bleeding, which led to the patient’s complete recovery. But in the remaining 4 cases, the patients died from complications. Wolf was not a theorist. The first theoretical justification for blood transfusion belongs to the professor of the Medical and Surgical Academy, Stepan Fomich Khotovitsky. In 1830, Khotovitsky wrote: “In case of severe bleeding, when all the signs of approaching death are already evident... there is no other means of salvation than a blood transfusion.” He describes the technique of this operation as follows: “The pump must be blown inside and not at all smeared with oil, all equipment must be heated hot; special attention must be paid to ensure that no air gets in.”
In 1846, an article by I.V. appeared in the Military Medical Journal. Buyalsky about the importance of blood transfusion. I.V. Buyalsky (1846) insisted on the use of blood transfusions in the treatment of the wounded. In 1847, the prosector of Moscow University I.M. Sokolov was the first to transfuse human blood serum into a cholera patient.
In Russia, the first fundamental work on blood transfusion was the book by A.M. Philomafitsky “Treatise on blood transfusion as the only means in many cases to save a dying life, compiled in historical, physiological and surgical terms...” (1848). In 1865 V.V. Sutugin, in his doctoral dissertation “On Blood Transfusion,” came to important conclusions: the transfused blood must be deprived of the ability to clot; Only human blood is suitable for a person; It is best to transfuse slowly to avoid negative reactions. The dissertation was the first to propose the idea of preserving blood. Following Sutugin’s work, Rauschenberg’s interesting dissertation “On Blood Transfusion” appeared. The author suggested adding potassium carbonate to it to avoid blood clotting. Here the question about donors was raised: “This person - man or woman - should be no older than 40 years old, should not be affected by syphilis, scurvy, anemia or other diseases affecting the blood.”
In 1887, from the clinic N.V. Sklifosovsky published Dr. Tabure’s dissertation “On Blood Transfusion,” which substantiated the enormous role of blood transfusion in military field surgery. In the 60s - 80s. XIX century In Russia, three important discoveries were made in the field of blood transfusion: S.P. Kolomnin introduced the method of intra-arterial transfusion, V.V. Sutugin - a method of preservation and V. Rautenberg - a method of chemical stabilization of blood. N.I. Pirogov emphasized the benefits of blood transfusion for some wounds in the field.
At the end of the 19th century. A. Schmidt conducted experiments to study the mechanism of blood coagulation, and P. Ehrlich, I.I. Mechnikov, E.S. London, L.A. Tarasovich observed hemolysis of erythrocytes when they were mixed with the blood serum of various animals.
The second period in the history of blood transfusion is associated with the development of the doctrine of immunity. During this period, in 1900, K. Landsteiner discovered three blood groups. In 1907 Y. Yansky and in 1910 V.L. Moss was diagnosed with blood type IV. The American surgeon J. Crile (1907) was the first to apply the doctrine of blood groups in the practice of blood transfusion (he performed 61 transfusions of compatible blood).
An important event of the beginning of the 20th century. should be considered the proposal of V.A. Yurevich and N.K. Rosengrat (1910), A. Justen (1914), R. Levinson (1915), L. Agote (1915) use sodium citrate to prevent blood clotting during transfusion - the so-called citrate method of blood transfusion has received universal recognition.
Major discoveries in the twentieth century were made in our country. In 1919 V.N. Shamov, N.N. Elansky, I.R. Petrov received the first standard serum to determine blood group. V.N. Shamov was the first to perform a blood transfusion taking into account group factors. The experience of blood transfusion was summarized in the monograph by N.N. Elansky “Blood Transfusion” (1926). V.N. Shamov (1929) and S.S. Yudin (1930) developed methods of blood transfusion of the dead.
In 1926, the world's first Institute of Blood Transfusion was created in Moscow.
How to prepare for bloodletting?
The most important thing is the attitude. A person must make sure that the treatment will bear fruit and the illness will go away. You need to turn to Allah for help and believe that he will help.
The procedure must be carried out by an experienced hajjam specialist. It is important that the procedure is performed by a person of the same gender as you.
It is better if hijama is done on an empty stomach, but you can drink water and juices.
Be sure to notify the hajjam about your illnesses, including HIV, hepatitis and syphilis, to avoid infecting the specialist.
How to behave correctly after hijama?
In the first 24 hours, it is recommended to refrain from heavy labor, as the procedure takes a lot of effort. Also, you should not take a lot of heavy foods that are difficult to digest. It also includes salty, fried, spicy food.
Rest, don't be nervous, avoid increasing blood pressure. Smokers are advised to abstain from cigarettes for 24 hours.
Be sure to cover the area where the procedure was performed and do not cool it. After your condition improves, thank Allah.
This technique is very non-standard and has many contraindications. Whether to use it or not is everyone’s choice. If you decide to undergo hijama, be sure to consult your doctor and study all the information. Be healthy!
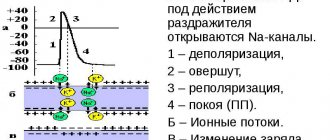
Humor theory
In the European tradition, the idea of the benefits of bloodletting goes back to the ancient doctrine of humors and temperaments. According to Hippocrates, the human body was governed by the ratio of four vital juices (humors) - blood, phlegm, yellow and black bile. Humors, in turn, correlated with the four elements (fire, water, earth and air) and the movement of the heavenly bodies. Thus, a correspondence was established between the macrocosm and the microcosm, the Universe and the human body, and order and health were understood as the balance of the elements. In the human body this balance was expressed as the balance of humors. An imbalance entailed illness, excess and passion - and, conversely, a bad regime and vices caused an imbalance. Diseases were explained by acute, chronic or hereditary excess of one humor and deficiency of others.
Of the four humors, the greatest attention was paid to the quantity and quality of blood, in which all four elements were combined and balanced. The blood should not be too hot (this indicated an excess of the fiery principle) or too cold (excess water), too viscous (excess earth) or too liquid (excess air). According to the ideas of doctors of Antiquity, blood was created by the body from food and served as a building material for meat and bones. Hence the diet was based on the consumption of meat and neglected greens and vegetables, which were considered useless.. A lack of blood was harmful, but an excess was much more dangerous, and bloodletting became a way eliminate this excess.
Miasm
Until the 19th century, doctors assumed that infectious and colds arose from putrefactive, unhealthy fumes. There are certain “contagious principles” that cause typhoid fever, malaria, and cholera. They tried to study and classify them until pathogens were discovered. In official medicine, the term is outdated, but it arose again in homeopathic theory.
Samuel Hahnemann
In 1830, the “father of homeopathy,” Samuel Hahnemann, published Chronic Diseases, in which he outlined the theory that the vast majority of chronic diseases are caused by an infectious agent (“miasm”). In particular, he looked at the “psoric miasm” that causes scabies and dermatitis. It is characteristic that in his essay of 1803 he associated the occurrence of these same diseases with the consumption of coffee. Thanks to Hahnemann, the idea of miasms became firmly established in homeopathic theory.
Subsequently, homeopaths proposed their own classification of miasms. According to homeopathic physician, obstetrician and gynecologist Victor Linde, there are three options for their occurrence. The first is miasm as an attribute of the entire species Homo Sapiens, the result of the confrontation between the individual and society. In this case, the cause of the chronic disease lies outside human physiology. The second is miasm as an attribute of a particular society. The third is the miasma that manifests itself in individuals.
The Austrian homeopathic physician Matthias Dortsche considered miasms as a consequence of errors accumulated by previous generations in the work of various functional systems, by analogy with accumulated genetic mutations.
Supporters of homeopathy still do not write off the theory of miasms and study it not in the context of the history of medical errors, but as a basis for diagnosing and treating patients. Here is an example of a lecture on this topic from a candidate of medical sciences.
Homeopathy
Homeopathy itself, as a type of alternative medicine, is based on outdated ideas that the active molecules of a drug, when diluted and shaken, “increase vitality,” which allows them to be used in ultra-small doses, and diseases can be treated with small doses of those substances that in large volumes cause the symptoms of this diseases. Hahnemann's ideas in the 19th century have been repeatedly challenged by the scientific community, but today there is a huge industry of homeopathic medicines.
In itself, taking “cakes with nothing” tablets does not harm the body, since they consist almost entirely of excipients - sugars or chalk. But if a person suffers from a certain disease, then treatment with homeopathy is equivalent to no treatment at all.
The declared effect of substances in large dilutions cannot be scientifically verified, but supporters are trying to convince that the drugs are much more effective compared to traditional medicine, in particular because they are selected individually for each patient.
In 2021, the Commission for Combating Pseudoscience under the Presidium of the Russian Academy of Sciences published a memorandum “On the pseudoscience of homeopathy,” in which it stated that the principles of homeopathy contradict known chemical, physical and biological laws. It emphasizes that there is no convincing evidence of its effectiveness, and also puts forward recommendations for health organizations, pharmacists and individual doctors offering this dubious treatment. The memorandum caused a scandal in the scientific community, but could not overcome the problem of pseudoscience in medicine.
Homeopathy is still taught in universities, and dissertations on pharmaceuticals are even defended, studying release-active (homeopathic) drugs.
Hijama - indications for use
The benefits of such a procedure are great. Bloodletting treatment is recommended in the following cases:
- diseases of the urinary system;
- diabetes;
- pleurisy;
- diseases of the musculoskeletal system;
- hypertension;
- chronic heart failure;
- sinusitis;
- meningitis;
- hyperemia;
- problems with blood clotting;
- difficulty breathing.
Some experts believe that hijama is unnecessary for girls and women who regularly menstruate. They recommend performing this procedure only after menopause. However, there are also those specialists who approve of bloodletting. They argue that hijama is not like menstruation, since it involves a different type of cleansing. With this procedure, stagnant capillary blood is removed from the body. Hijama helps to get rid of the following problems:
- low immunity;
- vein problems;
- muscle colic;
- female infertility;
- numbness of the limbs;
- pathologies of the gynecological system.
It is important to understand hijama - what it is, and for men. With the help of bloodletting you can get rid of the following problems:
- prostatitis;
- decreased libido;
- hemorrhoidal condition;
- impotence;
- pulmonary edema;
- poisoning by poisons.
In addition, cosmetic hijama is practiced. It has an amazing effect on the skin:
- evens out turgor;
- increases blood flow;
- due to the destruction of melanin, it removes pigment spots;
- enhances the production of elastin and collagen.
Hijama is used effectively for weight loss. Often the reason for gaining excess weight is metabolic disorders. Bloodletting helps normalize all this. Due to blood clots, lymph stagnation occurs, which slows down vital processes in the body. As a result, a variety of complications can arise. Bloodletting removes stagnant fluid, improves metabolism, which promotes weight loss.
Lobotomy
In addition to false beliefs, there have been real crimes in the history of medicine. One of them is lobotomy. In psychiatry in the 1930s, it was believed that schizophrenia and other psychiatric problems could be treated by excision or complete removal of the frontal lobes. Such a neurosurgical operation gave, to put it mildly, questionable results. Some patients actually felt improvement, but much more often the “improvement” was associated with severe impairment of cognitive functions and the patient’s transition to a “vegetative” state.
The operation was performed through the eye socket or airway. As a result of the lobotomy, the neural connections of the neocortex were destroyed in the area where disturbances occurred, leading to manic and psychotic states. Along the way, the zones responsible for emotions and making logical decisions were destroyed, and the patient became incapable of independent existence.
Egas Moniz
The worst thing was not that mutilation instantly became popular in the USA and other countries and at least 50 thousand people were subjected to it. And it’s not that during the heyday of lobotomy, the kitchen knife for chopping ice became the most suitable tool for the operation. And the fact that the doctor Egas Moniz, who developed this procedure, received the Nobel Prize in Physiology or Medicine in 1949 “for the discovery of the therapeutic effect of leucotomy in certain mental illnesses.” The Nobel Committee did not revoke the award even after numerous appeals from relatives of victims of barbaric treatment.
In the USSR, psychiatrists also practiced “excision of white matter,” but did this through craniotomy. This was thought to be the best way to target painful nerve connections without harming other areas of the brain. Improvement was observed in an encouraging number of patients (about 60%), but experiments with brain invasion were stopped in the 1950s.
Rosemary Kennedy, daughter of US President John Kennedy
In the United States, on the contrary, patients with psychiatric diagnoses were maimed for more than twenty years. The most striking story is about Rosemary Kennedy, daughter of US President John F. Kennedy. The girl suffered from mental disorders and became a threat to the family's reputation. Her father sent her for surgery. The lobotomy not only did not help solve the girl’s mental problems, but also brought her profound disability, with which she lived until she was 87 years old.