The “classical” operation for varicose veins under anesthesia with incisions in the groin area and along the legs, which was used to remove superficial varicose veins at the beginning of the last century, is an atavism of the past. The suffering of patients, long hospitalization and pain in the legs after such operations aimed at improving blood flow are completely unjustified. Severe varicose veins can be treated without resorting to “inquisition methods.” Today, treatment of advanced varicose veins can be carried out without anesthesia and hospitalization. The work of a phlebologist becomes office-based, without the attributes of major surgery.
Knowledge of what causes varicose veins in the legs allowed us to develop hemodynamic principles of treatment. Their implementation is possible by removing or switching off the vein from the blood circulation. Modern technologies are based on the principle of fusion of vein walls in the area of insufficient venous valves. The method of influencing venous circulation can be different, but its goal is the same - to stop the pathological discharge of blood through the affected vein (anti-reflux). At the Innovative Vascular Center, there are methods for effective treatment of varicose veins of the lower extremities without the slightest incisions or scars, eliminating both the causes and signs of venous pathology. Phlebologists at our center are pioneers in the introduction of modern technologies for varicose veins. Our clinics successfully treat more than 1,000 phlebological patients per year. We are responsible for the results of our operations for varicose veins of the lower extremities and provide written guarantees.
How can you cure varicose veins on the legs?
Understanding the cause of varicose veins allows you to choose the right method of treatment. The goal of modern treatment of varicose veins is to solve several problems:
- Termination of pathological discharge in a vertical position through the incompetent saphenous veins of the lower extremities.
- Elimination of reflux between deep and superficial veins - perforators - the main mechanism for the development of varicose trophic ulcers.
- Removal of varicose - degenerated superficial vessels (varixes).
- Compression therapy using special stockings and socks.
results
In order to exclude the phenomenon of orthostatic hypervolemia, conducting the study in the first half of the day was fundamental. Numerical characteristics of descriptive statistics in all groups are presented in the table . The histograms constructed on the basis of the obtained data are presented in Fig. 2 . A standard histogram of the range of data (medians with an interquartile range of the 25th–75th percentile) obtained in the comparison groups is presented in Fig. 3 . In Fig. 4, 5 show histograms of the range with analysis of data on the mathematical expectation and standard deviations in the comparison groups at critical values of –1.96 and ±1.96. Analysis of the statistical significance of the obtained mathematical characteristics in the comparison groups using a two-sample t-test for independent samples according to the Student's t-test calculated by the program showed a high statistical significance of the differences between all groups, since the p value in all cases was less than 0.0000 and only when comparing C2—C3 and C4-C6 was one order of magnitude greater - 0.004, which did not affect the statistical significance of the differences when testing hypotheses about the mathematical expectation.
Table . Numerical characteristics of descriptive statistics for comparison groups, according to the diameters of the intramuscular veins of the leg, obtained during ultrasound scanning*
| Numerical characteristic | Norm | C0—C1 | C2—C3 | C4—C6 |
| Sample size | 412 | 359 | 570 | 274 |
| Expected value | 0,351 | 0,454 | 0,796 | 0,808 |
| Standard deviation | 0,061 | 0,065 | 0,149 | 0,153 |
| Credibility —95,000% | 0,345 | 0,448 | 0,783 | 0,790 |
| Credibility ±95,000٪ | 0,357 | 0,461 | 0,808 | 0,827 |
| Standard error of mathematical expectation | 0,003 | 0,003 | 0,006 | 0,009 |
| The coefficient of variation, % | 17,4 | 14,3 | 18,7 | 18,9 |
| Median | 0,330 | 0,500 | 0,800 | 0,805 |
| Fashion | 0,300 | 0,500 | 0,900 | 0,900 |
| Mode frequency | 139 | 135 | 67 | 30 |
| Dispersion | 0,004 | 0,004 | 0,022 | 0,023 |
| Minimum value | 0,220 | 0,300 | 0,300 | 0,450 |
| Maximum value | 0,510 | 0,610 | 1,300 | 1,250 |
| Asymmetry | 0,725 | —0,683 | 0,051 | 0,011 |
| Standard error of skewness | 0,120 | 0,129 | 0,102 | 0,147 |
| Lower quartile | 0,300 | 0,400 | 0,700 | 0,700 |
| Upper quartile | 0,400 | 0,500 | 0,900 | 0,910 |
| Quartile range | 0,100 | 0,100 | 0,200 | 0,210 |
| Swipe options | 0,290 | 0,310 | 1,000 | 0,800 |
| 10,000 percentile | 0,300 | 0,350 | 0,600 | 0,600 |
| 90,000 percentile | 0,450 | 0,510 | 0,970 | 0,990 |
Note. *—variable value P (confidence probability) = 0.95; significance level p<0.05.
Rice. 2. Standard histograms of variation series in the compared groups.
a - group 1 (norm); b - 2nd group (C0-C1); c - 3rd group (C2-C3); d - 4th group (C4-C6). The Y axis shows percentages, the X axis shows the diameter of the veins in centimeters.
Rice. 3. Histogram of analysis of median data with interquartile range 25-75th percentile obtained in the compared groups.
Rice. 4. Histogram of data analysis of mathematical expectation and standard deviations in the compared groups.
a - in the 1st (normal) and 2nd (C0-C1); b — in the 1st (normal) and 3rd (C2-C3); c - in the 1st (normal) and 4th (C4-C6).
Rice. 5. Histogram of data analysis of mathematical expectation and standard deviations in groups C0-C1 and C4-C6 (a) and C2-C3 and C4-C6 (b).
Taking into account the established fact, the null hypothesis H0, representing the statement that when clinical classes on CEAP change, there is no change in the diameter of intramuscular veins, was rejected, and the alternative hypothesis H1 was accepted as the main one, stating that when clinical classes on CEAP change in patients, increase in the diameter of the intramuscular veins of the leg.
Opportunities of the Innovative Vascular Center
- Thermal methods for treating varicose veins are endovenous laser coagulation (EVLC) and radiofrequency obliteration (RFO) of the veins of the lower extremities.
Endovenous laser coagulation is an effective treatment for varicose veins, the principle of which is based on the thermal effect of laser energy. This treatment was introduced in 2001 and is still the best method. With laser coagulation, the damaged vein is heated by a laser beam, which provides a strong effect of damaging the collagen of the venous wall, causing an inflammatory process in the vein and its overgrowth. Advanced varicose veins on the legs, which are treated with this method, regress completely and without a trace, and its main symptoms disappear: swelling, heaviness in the legs, hyperpigmentation of the skin. Varicose veins have been treated at the Innovative Vascular Center in Moscow using lasers since 2005, since the advent of this technology in Russia.
EVLT begins with the installation of a laser fiber into the lumen of a varicose vessel through a skin puncture, which is guided along the affected vein to the site of the incompetent valve. For the patient, this method is a safe, painless and reliable way to prevent further development of the disease and its complications. Complete elimination of varicose veins is observed in 98% of patients with proper use of the EVLT method. The capabilities of this method make it possible to both treat varicose veins on the legs in women and correct venous outflow in case of trophic ulcers.
Radiofrequency obliteration (RFO)
Treatment of varicose veins using the radiofrequency obliteration (RFO) method is a similar thermal method, but heating of the tissue of the venous wall occurs according to different physical principles due to radio wave energy. Radiofrequency obliteration allows you to remove varicose veins and eliminate its symptoms; such treatment in its immediate and long-term results does not differ from EVLT, but is more painstaking for a phlebologist.
Other thermal methods
When deciding how to treat varicose veins, phlebologists often used exotic methods. Varicose veins were treated with thermal effects using superheated steam and bipolar electrocoagulation. However, modern thermal methods are more effective and they allow the doctor to prevent further development of varicose veins, and the patient to be treated on an outpatient basis without disturbing his lifestyle. In the hands of a novice phlebologist, thermal ablation methods can cause unpleasant complications: decreased sensitivity, burns, seals. The effectiveness of this method in the hands of an experienced phlebologist is more than 98%, and the laser method and RFO make it possible to get rid of not only the initial form but also severely pronounced varicose veins on the legs without incisions. In the photographs from the “Treatment Results” section you can see the view before and after minimally invasive treatment.
Non-thermal methods for eliminating stem reflux
For many years, phlebologists have been thinking about how to cure varicose veins of the lower extremities without incisions and pain. The disappearance of the saphenous veins in the arms after frequent injections prompted the idea that certain substances can cause inflammation of the vein walls - thrombophlebitis and subsequent gluing of them with the disappearance of the lumen of the vein. After the advent of the Fegan method, when treatment began to be carried out based on the cause of varicose veins, the development of non-thermal scleroobliteration methods began. Since then, varicose veins on the legs, especially in women, are treated not only with a scalpel, but also with a syringe.
- Sclerotherapy
Sclerotherapy appeared in the practice of doctors at the end of the 19th century. In recent years, the method of treating varicose veins using injections of a special substance (sclerosant) has reached perfection. The main point of sclerotherapy is to inject a drug into a varicose vein, which causes inflammation and subsequent gluing of the varicose vein. Sclerotherapy does not involve eliminating the cause of venous insufficiency and is more suitable for certain forms of varicose veins or in the initial stages of the disease. Advanced varicose veins of the lower extremities are treated with more complex methods; damage to the trunk of the great or small saphenous vein does not allow one to count on a long-term effect of sclerotherapy, since a relapse is sure to occur due to reflux.
Sclerotherapy can be done if you are not allergic to tetradecyl sulfate or polidocanol. These substances are the main sclerosants. During sclerosing treatment, manifestations of thrombophlebitis may occur, especially if liquid forms of the drug are used. Sclerotherapy of perforating veins is highly effective in the treatment of venous trophic ulcers. It is possible to eliminate the manifestations of varicose veins of the lower extremities at any stage with the help of sclerotherapy, but the relapse rate is about 40% over the next 5 years.
The advantage of sclerotherapy is a good immediate effect and low cost of treatment. Injections of sclerosant lead to the gluing of veins and the cessation of the pathological process - reflux of blood through the saphenous veins. The drug is usually injected in the form of foam (Foam-Form) into varicose veins. A spasm of dilated subcutaneous vessels is formed, prolonged contact of the foam form of sclerosant with the vein wall and their subsequent inflammation and gluing. This process occurs unevenly and the degree of obliteration of the vein is not the same, so 40% of patients after sclerotherapy have relapses of varicose veins. After sclerotherapy, the affected area of the veins of the lower extremities closes and over time completely heals, and the blood flow in the opposite direction stops. To prevent the occurrence of skin necrosis due to the penetration of the foam form of sclerosant into the subcutaneous tissue, administration is carried out strictly under ultrasound control.
Foam sclerotherapy can be used as a stand-alone method or in combination with laser treatment to eliminate varicose veins. The number of sessions to eliminate varicose veins using sclerotherapy depends on the stage of varicose veins and the condition of the veins. The course of treatment usually consists of 2-3 procedures. The area of skin over the sclerotic vessel may take on a dark shade for 2-3 months (hyperpigmentation appears). It can ruin a woman's legs for several months, so this treatment is best done in the winter months. Drug treatment and ultrasound-guided vascular punctures can speed up the process of resorption of intravascular fluid accumulations (coaguls), the risk of which is about 10%. Coaguli form when there is insufficient compression, but will certainly go away over time. Many patients know that within a month after sclerotherapy, the signs of varicose veins of the lower extremities go away for many years, which is why sclerotherapy is still one of the most popular treatment methods.
- Using special glue (VenaSeal)
Since its inception, this method has aroused great interest among phlebologists. It involves gluing the trunk of the great saphenous vein with a special cyanoacrylate glue. In the lumen of the vessel, this glue polymerizes and fills the lumen of the dilated vessel. According to the developers, this method does not require any anesthesia, and a “plug” appears in the vessel, which reliably blocks blood flow. Taking this into account, half an hour is enough for the procedure to eliminate varicose veins on the legs. Venasil is the only technology for the treatment of varicose veins that does not require wearing compression stockings.
Most women can return to normal activities immediately. Symptoms of chronic venous insufficiency are relieved shortly after the procedure. The process of active promotion of this glue to the phlebological market should begin in the near future. However, there are certain disadvantages: The presence of a foreign body in the human body. The curdled glue remains in the vessel forever and can cause chronic allergies; sometimes there is inflammation of the vessel wall or rejection of the polymer with suppuration. Acute thrombophlebitis of the glued vessel may occur.
The use of glue in the trunk of the great saphenous vein does not eliminate the need to eliminate varicose tributaries, which is why doctors will have to remove signs of subcutaneous varicose veins with sclerotherapy or miniphlebectomy. The visible effect of using glue appears only when combined with other methods of eliminating varicose veins. The patient has to pay more. The unreasonably high cost of the gluing kit makes this procedure significantly more expensive than the modern laser or radio frequency method.
In our clinic, preference is given to thermal methods. We believe that it is better to give good local anesthesia than to treat varicose veins of the saphenous veins on the legs with an expensive and untested method. Moreover, the result is the same at best. If a relapse occurs, the patient will have to undergo a complex operation to remove the sealed vessel, since other methods will no longer be applicable.
- ClariVein mechano-chemical obliteration technology
The modern method of combined treatment of reflux along the subcutaneous venous trunks adds extra weight to conventional sclerotherapy. Mechano-chemical procedures mean a combination of mechanical damage to the inner surface of the venous wall and the introduction of a sclerosing drug. A catheter is inserted into the main saphenous vein through a puncture under ultrasound guidance. After installing the catheter in the desired location, the device is connected. The rotating sharp head of the catheter makes up to 3.5 thousand revolutions per minute, causing severe damage to the inner layer of the venous wall. At the same time, a sclerosing drug is injected through the catheter, which “mixes” in the lumen of the vessel and, using the rotating part of the catheter, acts on the vascular wall, causing its inflammation and gluing.
To date, the only advantage of this technology is the absence of the need for tumescent anesthesia. Mechano-chemical obliteration should, according to its inventors, trigger a stronger obliteration effect than foam sclerotherapy, although for some reason convincing data have not yet been presented. It is clear that such varicose veins can be treated with other minimally invasive methods, so its advantages are not obvious. The introduction of such therapy in Russia will begin in 2021, but statistical data on its advantages over EVLT and sclerotherapy do not yet exist. We have to wait for further studies from Europe or the USA in order to accurately determine the place of this technology.
- Miniphlebectomy
This is a modern microsurgical aesthetic method for removing varicose veins. It involves a delicate technique of puncturing and pulling out varicose veins using special tools. This operation is not for a novice phlebologist; you need to have the skills of delicate surgery. Miniphlebectomy is an operation without the use of a scalpel and is performed under local anesthesia. The punctures are carried out in the direction of the skin lines, so after 2 months they are practically invisible.
Miniphlebectomy has replaced the classical operation for varicose veins, which involves the use of 1-3 cm incisions, as it is aesthetically flawless, painless and very effective. By assuming how varicose veins manifest, the doctor can clearly plan micro-punctures and get by with minimal intervention. The patient can go home on his own feet immediately after the operation. Miniphlebectomy can be an independent effective method of treating varicose veins, or used in combination after laser coagulation of varicose veins. Removal of varicose veins is carried out using a special technique developed by Professor Varadi. This technique has been perfectly mastered by our phlebologists and allows for the removal of varicose veins on the legs - an effective treatment regardless of its cause.
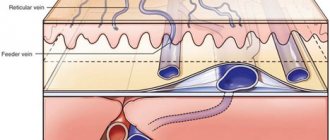
Main Difference – Veins vs Arteries
Veins and arteries are two types of blood vessels in a closed circulatory system. The main function of blood vessels is to carry blood throughout the body. But arteries and veins differ in their structure and function. Veins are made up of a thin, elastic layer of muscle in their wall, while arteries are made up of a thick, elastic layer of muscle. A thick artery wall is important when dealing with high pressure blood released by the heart. Veins carry oxygen-depleted blood to the heart, while arteries carry oxygenated blood away from the heart. The main difference between veins and arteries is that veins are involved in removing cellular waste from the extracellular environment, whereas arteries are involved in providing nutrients and oxygen to the body's cells .
Key areas covered
1. What are veins - definition, features, functions 2. What are arteries - definition, features, functions 3. What are the similarities between veins and arteries - Brief description of the common features 4. What is the difference between veins and arteries - Comparison of the main differences
- The veins behind the knee hurt
Key words: aorta, arteries, arterioles, blood capillaries, blood pressure, closed circulatory system, veins, venules