Vasculitis ( angiitis, arteritis ) is a general name for a group of diseases associated with inflammation and destruction of the walls of blood vessels. Inflammation of blood vessels can occur in any organ.
The disease vasculitis leads to the fact that the vessels cease to properly perform their function (supplying blood to tissues and removing metabolic products), so the organs adjacent to them are affected.
Vasculitis has different classifications and may differ in localization, etiology and severity of the clinical picture. Some vasculitis affects only the skin, while others affect vital organs.
Left untreated, vasculitis can result in serious complications. Intestinal and pulmonary bleeding, thrombosis, renal failure, liver failure, heart attack - this is not a complete list of the dangerous consequences of the disease. Vasculitis can lead the patient to disability and even death.
1 Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
What is vasculitis?
Vasculitis is a group of diseases characterized by the development of inflammation of the walls of blood vessels. This inflammation begins due to an impaired immune response. The cause may be a past infection or allergy. Inflammation can affect small, medium, and large vessels. Because of it, blood circulation and blood supply to individual organs are disrupted, which can cause complications. Without treatment of vasculitis, necrosis of the vessel walls (death of their tissue), bleeding, and ischemia (impaired blood flow) begin. Both children and adults can get vasculitis. The disease can be primary (when inflammation of the walls of blood vessels is the only manifestation without an apparent cause) or secondary. With secondary vasculitis, the walls of blood vessels become inflamed due to other diseases (infectious, oncological, rheumatic).
General overview
Vasculitis can affect any of the body's blood vessels. These include arteries, veins and capillaries. Arteries carry blood from the heart to the organs of your body. Veins move blood from your organs and limbs back to your heart. Capillaries connect the small arteries and veins in your body.
When a blood vessel becomes inflamed, it narrows or becomes blocked, restricting or preventing the flow of blood to other vessels. In the process, the blood vessels stretch and weaken, creating bulges that cannot be seen with the naked eye on the skin. These bulges are called an aneurysm.
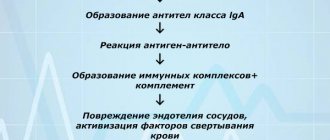
Pathogenesis of vasculitis
Vasculitis develops due to a failure of immune mechanisms, but the exact causes of the disease have not been identified. The main hypothesis assumes that the nature of the disease is multi-etiological, associated with many factors. These include:
- acute or chronic bacterial or viral infections;
- allergy. A severe allergic reaction to drug components or food can cause immune failure;
- complication of vaccination. If after vaccination the immune response is impaired, vasculitis may occur. Such complications are very rare;
- severe or prolonged effects of stress, hypothermia or overheating, injuries.
Under the influence of these factors, the production of pathogenic immune complexes begins. Normally, they attack the pathogen, but due to an immune failure, the attack is directed at the body’s cells. Immune complexes attach to the walls of blood vessels, damage them and provoke inflammation.
Figure 1. The difference between a healthy vessel and one affected by vasculitis. Source: sl.smithhealthcentre.com
Classification
Vasculitis is a large group of diseases, and two classifications are used for them. The first is by etiology - it takes into account the reasons for which the disease appears. The second is by localization, taking into account which vessels are affected.
By etiology
This classification takes into account the causes of vasculitis:
- primary. Inflammation of the walls of blood vessels is not associated with other diseases, is not their manifestation and develops as an independent disease. The exact causes of primary vasculitis have not been established, but it is known that hereditary predisposition plays an important role;
- secondary. The walls of blood vessels become inflamed due to other diseases, inflammation is one of their manifestations.
There are several types of secondary vasculitis based on the underlying disease or condition that caused inflammation of the vessel walls:
- hepatitis B and C viruses;
- syphilis;
- oncological diseases;
- reaction to taking medications.
By localization
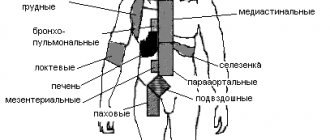
Division by localization takes into account which vessels are affected by vasculitis and where they are located. This determines the clinical picture, treatment approaches, prognosis and possible complications. The walls of small, medium and large blood vessels can become inflamed; inflammation can affect blood vessels of different sizes or vessels of individual organs.
Vasculitis of large blood vessels
When the walls of large blood vessels become inflamed, there are several common symptoms. These are large deviations from the norm when blood pressure changes and anomalies in the propagation of pulse waves. With each such wave after the heart contracts, the pressure in the arteries increases. If the wave is asymmetrical or absent on the arms or legs, this may be a sign of vasculitis. The disease is also indicated by the development of ischemia (decreased blood flow in a particular area), intermittent claudication (pain that occurs when walking and goes away after rest). Each type of vasculitis of large blood vessels has its own additional symptoms.
Giant cell arteritis. Inflammation affects the thoracic aorta, as well as the large arteries running from it to the neck, and the extracranial section of the carotid artery. Polymyalgia rheumatica is often the cause of giant cell arteritis. Symptoms include: headaches, blurred vision, fever, weight loss, fatigue, and general malaise.
Takayasu arteritis. Inflammation of the walls of the aorta and its branches, the walls of the pulmonary arteries, most often develops in young women. The first signs of the disease are weakness, spastic pain in the limbs, periodic visual disturbances, hypertension, differences in pulse or blood pressure values on different legs or arms or on an arm and leg on the same side.
Vasculitis of medium-sized vessels
The general manifestation is symptoms of infarction of the tissues of the affected organs: their necrosis occurs due to insufficient blood supply. On the skin this is manifested by the formation of nodules, ulcers, and livedo reticularis (discoloration). With a muscle tissue infarction, severe pain appears. It is possible to develop multiple neuropathy (damage to several nerves), kidney damage (increased pressure in the renal arteries), and mesenteric ischemia, which disrupts blood flow in the intestinal vessels. The exact symptoms depend on where exactly the affected vessels are located.
Cutaneous vasculitis. It affects the vessels of the subcutaneous tissue, which is why ulcers, purpura (hemorrhages in or under the skin, look like scatterings of small red dots), petechiae (bright red rash) appear on the skin.
Polyarteritis nodosa. With this disease, the walls of the muscle arteries become inflamed, causing secondary tissue ischemia to develop. With nodular arteritis, damage to the skin, kidneys, peripheral nerves, gastrointestinal tract, and any other organs is possible. Lung damage is not typical. First, general symptoms appear: fatigue, fever. Other manifestations depend on which organ is affected.
Vasculitis of small vessels
When the walls of small vessels become inflamed, symptoms of tissue infarction develop in the affected area. Often these manifestations are similar to the symptoms of vasculitis of medium vessels.
Cryoglobulinemic vasculitis. It is systemic and affects mainly small vessels. Blood serum analysis reveals cryoglobulins. Symptoms are varied and are determined by the location of the inflammation. Damage to the kidneys and peripheral nervous system often develops, and vascular purpura appears. General manifestations are weakness, slight increase in temperature, fatigue. In 90% of cases, purpura appears, most often it forms on the skin of the legs. When the kidneys are damaged, peripheral edema and increased pressure in the renal artery develop. It is also possible to experience muscle and joint pain and enlarged lymph nodes.
Wegener's granulomatosis. The lesion can affect any organs, but most often it is the respiratory organs or kidneys. If the respiratory organs are affected, the first symptoms are cough and runny nose, after which swelling develops, increased pressure, and symptoms of damage to several organs at once appear.
Hemorrhagic vasculitis. More often children get it. There are four forms of the disease: cutaneous (cutaneous-articular), abdominal (with damage to the digestive organs), renal, mixed. Accordingly, characteristic symptoms are identified, including palpable purpura, abdominal or joint pain, renal syndrome, vomiting, and nausea.
Microscopic polyangiitis. A rare disease that most often affects the kidneys. In about a third of cases, additional purpura appears on the skin. Possible damage to the respiratory system with the rapid development of shortness of breath, hemoptysis, and anemia. If alveolar bleeding develops against this background, the patient needs emergency help. Abdominal pain, vomiting and nausea, and damage to the nervous system are also possible.
Vasculitides that can affect blood vessels of varying sizes
Behçet's disease. Inflammation develops on the walls of small or medium-sized vessels. Symptoms depend on location. The disease can affect the lungs, kidneys, stomach, and brain. A peculiarity is the frequent appearance of ulcers on the mucous membranes of the mouth, in the genital area, and other mucous membranes.
Cogan's syndrome. A rare disease in which blood vessels of different sizes become inflamed. The disease is often accompanied by fever, joint pain, neurological disorders, decreased vision, hearing loss (may be irreversible).
Systemic vasculitis
This group includes vasculitis associated with systemic diseases:
- systemic lupus erythematosus. The immune system begins to produce antibodies that damage healthy cells. Because of this, the walls of blood vessels become inflamed and lupus vasculitis develops;
- rheumatoid arthritis. This is a systemic inflammatory disease affecting small joints. May be accompanied by rheumatoid vasculitis;
- sarcoidosis The disease is accompanied by the formation of granulomas (nodules) in inflamed tissues. Foci of inflammation in sarcoidosis form in the lymph nodes, lungs, liver, spleen, skin, and bones. Sarcoidosis may be accompanied by sarcoid vasculitis.
Vasculitis of individual organs
Inflammation of blood vessels can affect only one, separate organ. Such diseases include:
- cutaneous vasculitis. Affects small and medium-sized vessels in the skin and subcutaneous tissue, manifested by the formation of ulcers, purpura, petechiae;
- cutaneous leukocytclastic angiitis. Inflammation of blood vessels in the skin is isolated and is not accompanied by systemic vasculitis or other associated conditions;
- primary angiitis of the central nervous system. It affects the vessels of the spinal cord, brain, and pia mater. There are no signs of systemic inflammation;
- isolated aortitis. A form of vasculitis with limited localization of inflammation of the vessel walls.
TREATMENT FOR VASCULITIS IS AVAILABLE AT BRANCHES:
Treatment of vasculitis in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of vasculitis in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
The disease is usually accompanied by complications. Intestinal bleeding may occur from the gastrointestinal tract. Vasculitis can also cause liver damage. In the cardiovascular system, disorders such as cardiomyopathy and disruption of the heart valves can form. The most dangerous consequence of vasculitis is stroke. In the excretory system, a possible complication is glomerulonephritis.
Causes
Inflammation of the walls of blood vessels begins due to autoimmune disorders, in which antibodies are produced against the cells of one’s own body. The exact causes of primary vasculitis have not been established. Secondary vasculitis develops against the background of infectious or oncological diseases, as a rare complication of vaccination, after overheating or hypothermia, or sunburn.
Other possible causes include allergies to medications. More than 150 drugs have been identified that can provoke the disease. These include some antibiotics, analgesics, radiopaque agents, serums, vaccines, as well as iodine preparations, B vitamins and other drugs. Allergies, autoimmune failure and the development of vasculitis do not always occur after taking them. The risk of such complications is determined by the individual reaction to the components of the drug. Therefore, it is important that all medications are selected by a doctor. You do not need to choose your own antibiotics or antihistamines.
Symptoms of vasculitis
The manifestations of vasculitis are determined by the type of disease, location and size of the affected vessels. The most common symptoms that appear are:
- increased body temperature;
- weakness, malaise, fatigue;
- decreased appetite, nausea and vomiting;
- rapid weight loss;
- pain: headaches, muscles, joints;
- dizziness, loss of consciousness;
- pallor of the skin, the appearance of rashes on it (ulcers, purpura, petechiae);
- if there are cardiovascular diseases, they worsen;
- Possible decreased vision;
- change in skin sensitivity (from weak, almost absent to too strong);
- symptoms associated with organs whose functioning is impaired due to insufficient blood circulation (this may be decreased vision, symptoms of kidney failure, problems with the digestive system).
Figure 2. Skin rash due to vasculitis.
Source: CC0 Public Domain Symptoms of inflammation are the first to appear, regardless of the size of the affected vessels. Fever occurs, general malaise occurs, weight begins to decrease, joint pain appears, and sweating increases at night. If the walls of small and medium-sized vessels become inflamed, skin lesions appear almost immediately: rash (palpable purpura, urticaria, and others), the formation of ulcers, nodules, livedo reticularis.
Figure 3. Reticular erythema pattern typical of livedo reticularis in cutaneous vasculitis. Source: Springer Science/Business Media
Some of the symptoms of vasculitis can be life-threatening and require immediate treatment. These are alveolar hemorrhage, mesenteric ischemia, a sharp decrease in vision, glomerulonephritis (kidney damage).
The exact symptoms of vasculitis depend on its form:
- cutaneous - an itchy rash appears on the skin as a result of pinpoint hemorrhages. At first, its color is red, but then the rashes darken, disappear, and pigmented areas remain in their place. More often, such rashes form on the skin of the buttocks and legs;
- articular - manifested by swelling, impaired mobility of large joints, pain;
- abdominal - abdominal pain, nausea, vomiting, loss of appetite;
- renal - change in the color of urine and a decrease in its volume. The urine turns red or pink. Clinical analysis reveals protein levels indicating glomerulonephritis. Without treatment, kidney failure develops.
Vasculitis in children
Vasculitis rarely appears in children. Almost always this is either hemorrhagic vasculitis or Kawasaki syndrome.
Kawasaki syndrome. Yonsei medical journal / Open-i (Attribution-NonCommercial 3.0 Unported)
Kawasaki syndrome is dangerous due to damage to the lymph nodes, heart vessels, and respiratory mucosa. The disease develops in an acute form with the sequential appearance of the following symptoms:
- severe fever with a rapid increase in temperature to 38-41 degrees;
- the appearance of a rash, erythematous spots on the skin;
- damage to the mucous membranes of the eyes, upper respiratory tract, nose;
- redness and then thickening of the skin on the palms and soles of the feet;
- inflammation, enlargement of lymph nodes in the neck;
- redness of the tongue;
- dryness and flaking of the skin on the phalanges of the fingers and toes, around the nails.
Kawasaki syndrome is dangerous due to damage to the cardiovascular system and the risk of aneurysm formation, but with timely diagnosis and treatment, the prognosis is favorable.
Hemorrhagic vasculitis in children can occur in several forms, including cutaneous, abdominal, skin-articular, and renal. Symptoms for each form vary:
- skin - the appearance of rash, swelling;
- abdominal - abdominal pain, nausea and vomiting, loss of appetite, weight loss;
- renal - decrease in urine volume, change in its color, appearance of protein in the analysis;
- articular - the appearance of joint pain, limited mobility of large joints.
Vasculitis in adults
Vasculitis in adults develops as a result of disturbances in the functioning of the immune system. The main risk factors are severe infections, untimely or improper treatment of infectious diseases, taking medications without a doctor’s prescription, allergies to food or medications, and the use of certain medications.
Vasculitis occurs as a chronic, progressive disease, and in this case, its treatment requires complex and long-term therapy. The earlier the diagnosis is made and treatment started, the better the prognosis. In adults, inflammation of the walls of blood vessels can provoke life-threatening conditions, so it is important to consult a doctor promptly. Inflammation of the walls of blood vessels may be indicated by ongoing fever, symptoms associated with poor circulation, muscle, headaches, and joint pain.
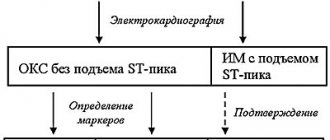
Tests and diagnostics
Vasculitis can occur in several forms, and the symptoms for each of them will be different. Often they are “masked” as other diseases, and therefore a detailed diagnosis is needed. It starts with contacting a rheumatologist. He can refer you to a dermatologist, cardiologist, immunologist, nephrologist and other specialists.
Diagnosis begins with the following studies:
- clinical blood test. Allows you to identify inflammation, signs of allergies, immune reactions;
- general urine analysis. Evaluates the condition and function of the kidneys. With a high protein content, it indicates glomerulonephritis associated with kidney damage;
- coagulogram. Evaluates blood clotting. With vasculitis, it decreases, which increases the risk of hemorrhage.
Additionally, tests can be performed for antibodies to hepatitis B and C (often detected with vasculitis), a biopsy of the affected tissue, followed by histology (the study of cells). Some laboratory tests are used to determine the type of vasculitis, its etiology, and the degree of organ damage.
During diagnosis, an ECG is also prescribed to assess the condition of the heart, identify circulatory disorders, radiography, CT or MRI of affected organs or large blood vessels.
Diagnostics
It is necessary to try to diagnose vasculitis even in the presence of the very first signs. The disease is serious and dangerous and requires immediate treatment.
If you suspect an illness, you must perform a series of examinations and tests. Appointed:
- angiography;
- general blood and urine tests;
- ECHO-cardiography;
- blood biochemistry;
- Ultrasound of the heart, abdominal organs and kidneys;
- X-rays of light.
The problem is that it is very difficult to diagnose vasculitis in the early stages. But more striking signs of the disease and a reason to sound the alarm appear even when several organs are affected at once.
In severe and rapid progression of the disease, an additional biopsy is performed, followed by a detailed study of tissue samples.
Treatment
The approach to treating vasculitis is determined by the location of the affected vessels, the presence of concomitant diseases, the severity of the condition, and a number of other factors. Most often, complex therapy is used, which involves taking medications, physiotherapy, diet, and preventing exacerbations. In severe forms of the disease, if thrombosis of large arteries or stenosis of the great arteries develops, surgical treatment is indicated.
Drug treatment of vasculitis
Approaches to treating vasculitis vary in each case. The rheumatologist will prescribe medications to reduce the production of antibodies and reduce tissue sensitivity. In some cases, antibiotics are needed, in others, antiallergic drugs.
Photo: lucky7trader / freepik.com
The attending rheumatologist should draw up a drug treatment program. Additionally, he can attract other doctors of a more narrow specialization. You cannot try to cure the disease on your own. It is dangerous due to severe complications and requires systemic and complex therapy.
Medicines for vasculitis
Prescribed in order to achieve stable remission and reduce the risk of complications. With secondary vasculitis, therapy is aimed at treating the underlying disease that caused vascular inflammation.
The following drugs are used for treatment:
- glucocorticosteroids or steroid hormones. Prescribed in almost all cases, they have anti-inflammatory and immunosuppressive effects. Doses of drugs are selected individually, creating a dosage schedule. Typically the dosage is high at first and then gradually reduced;
- cytostatics. They suppress the activity of the immune system, which allows for the correction of autoimmune mechanisms. Cytostatics are used in combination with glucocorticosteroids for severe forms of vasculitis. The drugs are prescribed as part of pulse therapy. It involves taking medications in short courses to avoid side effects;
- antitumor drugs, in particular Rituximab. These are monoclonal antibodies that are produced by immune cells, have immunosuppressive properties and are used in the treatment of systemic vasculitis if the use of cytostatics is undesirable. They are not prescribed for hepatitis B virus, neutropenia, low IgC levels in the blood and a positive tuberculin test.
Immunosuppressants (suppress the activity of the immune system), normal human immunoglobulin (used for infectious complications, severe kidney damage, development of hemorrhagic alveolitis), antibacterial, non-steroidal anti-inflammatory drugs, anticoagulants (prevent the formation of blood clots in blood vessels), antiallergic drugs can also be prescribed.
Physiotherapeutic methods for treating vasculitis
To treat vasculitis, plasmapheresis is used, in which blood is taken, purified and returned to the bloodstream. The technique is used as part of combination therapy if the disease is severe or acute and progresses rapidly. Plasmapheresis is prescribed in courses for severe kidney damage, as well as in cases where the use of cytostatics is contraindicated.
Treatment with folk remedies
Folk remedies are ineffective in treating vasculitis, and their use can be dangerous. If the disease progresses rapidly or becomes severe, you should immediately consult a doctor. Attempts to be treated with traditional methods will lead to a loss of time and can provoke complications.
Valeria Korol – general practitioner, rheumatologist, Member of the Expert Council of MedPortal
“Who is admitted to the hospital for vasculitis?
— All patients with newly diagnosed signs of systemic vasculitis. Special indications for hospitalization of patients with an established diagnosis of SV:
- Rapidly progressive deterioration of kidney function
- The appearance of protein in the urine - more than 3 g/day
- Recurring abdominal pain
- Damage to the organ of vision
- Signs of central nervous system damage"
Prevention
The causes of primary vasculitis are unknown, so special prevention is not carried out. Prevention of secondary vasculitis is carried out in several directions and involves restoration and maintenance of normal health:
- reducing the risk of contracting hepatitis B virus, hepatitis C virus, and other infections;
- timely and correct treatment of any diseases and especially infectious ones;
- taking medications only as prescribed by a doctor;
- maintaining a healthy lifestyle: maintaining a normal weight, giving up bad habits, proper nutrition and sufficient physical activity;
- allergy control. If they exist, it is important to exclude allergic reactions to food and medicines.
Angiitis of the skin: Etiology and pathogenesis.
In recent years, the theory of the immune complex genesis of angiitis has become increasingly widespread, linking its occurrence with the damaging effect on the vascular wall of immune complexes deposited from the blood. Among the etiological factors leading to inflammation of the vascular wall, focal (less often general) infection caused by staphylococcus or streptococcus, mycobacterium tuberculosis, enterococci, yeast and other fungi, and influenza virus is most often called. Among exogenous sensitizing factors for angiitis, a special place is currently given to drugs, primarily antibiotics and sulfonamides. Chronic intoxication, endocrinopathies, various types of metabolic disorders, as well as repeated cooling, mental and physical stress, photosensitivity, arterial hypertension, and venous congestion can play a significant role in the pathogenesis of angiitis
Diet for vasculitis
The diet for vasculitis is designed to eliminate food allergies, normalize weight, and provide the daily requirement for calories, vitamins, minerals, etc. When forming a diet, they take into account the causes that provoked vasculitis and which organs were affected due to inflammation of the walls of blood vessels and poor circulation. For example, if the stomach or intestines are damaged, a special nutrition plan is needed.
General recommendations involve organizing a healthy diet: excluding foods that cause an allergic reaction, eating enough fresh vegetables and fruits, dairy products, cereals, excluding fatty, spicy, fried foods. In each individual case, you can contact a nutritionist for help in creating a diet.
Consequences and complications
Without treatment, vasculitis becomes a life-threatening disease. It can cause pulmonary, intestinal and intracranial bleeding, thrombosis, renal or liver failure, myocardial infarction, and aneurysms. Possible complications include:
- intestinal obstruction;
- peritonitis;
- pancreatitis;
- heart attacks, thrombosis, ischemia of tissues and organs;
- perforation of intestinal and stomach ulcers;
- neuritis, cerebral disorders.
Even with timely treatment of vasculitis and persistent remission of the disease, consequences are possible, including chronic diseases of the kidneys, liver, digestive organs, breathing, hearing loss, vision loss and others. In order to most effectively restore normal health and quality of life, long-term systemic therapy is carried out.
List of sources
- Dunaeva N.V., Nikitina O.E., Stukov B.V., Karev V.E., Mazing A.V., Lerner M.Yu., Lapin S.V., Totolyan A. Cryoglobulinemic vasculitis associated with chronic hepatitis B: clinical observations and literature review.
- Nasonov E.L., Baranov A.A., Shilkina N.P. Hemorrhagic vasculitis (Henoch-Schönlein disease) // Vasculitis and vasculopathies. - Yaroslavl: Upper Volga, 1999. - 616 p.
- Handbook of a practicing physician. Under. ed. Vorobyova A.I. “Medicine”, 1981.
- Shostak N.A., Klimenko A.A. Systemic vasculitis: new in classification, diagnosis and treatment. Clinician. 2015;9(2):8-12
- Shilkina N.P., Dryazhenkova I.V. Systemic vasculitis and atherosclerosis. Ter. Arch. 2007; 3: 84-92.
Forecast
Depends on the form, localization of vasculitis, severity of the disease. In some cases, primary vasculitis goes away without treatment and leaves no consequences at all. In others, the disease develops rapidly and is life-threatening. It is important to consult a general practitioner or rheumatologist in time, immediately after the first symptoms appear. The main danger with most forms of vasculitis is possible complications:
- severe cardiovascular diseases, heart attacks with polyarteritis nodosa;
- development of infections and pulmonary hemorrhages with microscopic polyarteritis;
- infections, renal, respiratory failure, cardiovascular accidents with Wegener's granulomatosis;
- partial or complete loss of vision with giant cell arteritis (but overall the prognosis is favorable);
- strokes, heart attacks with Takayasu arteritis.
To improve the prognosis, it is important to strictly follow the recommendations of the attending physician, try to prolong the remission of the disease, and eliminate factors that provoke relapses.
Valeria Korol – general practitioner, rheumatologist, Member of the expert council of MedPortal “How to avoid recurrent vasculitis?
— Avoid factors that can provoke an exacerbation of the disease:
- Infections
- Stress
- Exposure to direct sunlight
- Unmotivated medication use
- To give up smoking
- Normalization of body weight
- Valeria Korol
- general practitioner, rheumatologist"