Pathogenesis
In a healthy person, the pressure in the right ventricle and the artery that carries blood to the lungs is the same. The pulmonary artery valve has a tricuspid structure, and when contraction of the right ventricle occurs, all its valves open completely under the influence of blood flow and facilitate its free flow into the space of the pulmonary artery. Then the walls of the right ventricle relax and fill it with venous blood coming from the organs and tissues of the body, which causes the valve flaps to close and ensures complete closure for the reverse flow of blood and the impossibility of penetration of biological fluids in the opposite direction - from the pulmonary artery to the right ventricle.
Pathogenesis causing pulmonary valve stenosis
In the case of valve stenosis, due to partial fusion of the leaflets, their complete opening becomes impossible, valve stenosis and a difference in pressure occur - in the ventricle it is too high, and in the pulmonary artery it is low enough to form a pressure gradient. In some cases, valvular stenosis causes the deformed leaflets to bulge during systole into the lumen of the trunk into the pulmonary artery and accelerate the systolic flow.
Stenotic valve
As a result of pulmonary stenosis, to compensate for hemodynamic disturbances, the right ventricle is forced to work extra hard to push blood through the narrowed lumen. This can lead to stretching, rigidity and hypertrophy (thickening) of the walls, as a result of which its cavity increases, rhythm is disturbed and heart failure . The narrowing site reduces the volume of blood flow, and insufficient blood supply to the lungs causes frequent bronchopulmonary diseases.
Forecast
Children with successful balloon valve repair have a favorable prognosis for life. Patients with a dysplastic pulmonary valve, often found in Noonan syndrome, have less favorable outcomes. Patients with successful balloon repair rarely require reoperation, unlike patients with right ventricular hypoplasia. The survival rate for such children is 60%. Mild to moderate pulmonary stenosis usually does not progress, and children have a favorable prognosis. In patients with severe stenosis, the defect progresses with age. The average life expectancy in the natural course of the defect is 25 years. After surgery, restenosis and valvular insufficiency of the pulmonary artery are possible. Long-term good results after surgical treatment were recorded in 84.3% of patients.
Classification
Depending on the location of the narrowing, there are:
- valvular stenosis is the most common case when the pulmonary valve itself is subject to pathological changes; its valves can be underdeveloped, fused together by commissures, and even have the appearance of a membrane with a hole in the center, ranging in size from 1-1.5 mm to normal;
- supravalvular - in which the trunk of the pulmonary artery is narrowed above the location of the valve;
- subvalvular (infundibular) – in this case, excessive growth of muscle tissue or fibrous structures in the area of the outflow tract of the right ventricle has occurred, preventing the blood flow from entering the pulmonary artery;
- peripheral - caused by a narrowing of the branches of the pulmonary artery that bring blood to the right or left lung.
According to the nature of the severity, the disease can be mild (asymptomatic), moderate-severe and critical.
How does the treatment work?
Drug and therapeutic treatment may be prescribed if there are contraindications to surgery or to alleviate the child’s condition.
First, the patient is constantly monitored:
- perform echocardiography;
- preventive measures for endocarditis (infectious);
- use of antibiotic therapy for prophylactic purposes;
- identification of pathogenic carriers of infection.
Carrying out surgical treatment
This heart defect requires only surgical intervention. It is noteworthy that the operation is recommended even for the second and third stages. If a child has moderate stenosis, he will be observed for a long time without surgical treatment.
If the pathology requires urgent surgery, then there are several types of surgical intervention that eliminate heart defects.
| Name of surgical procedure | Short description |
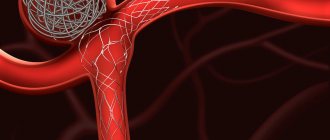
| Pulmonary valvuloplasty (closed type) | This type of surgery is very often used to treat SLA. Penetration to the heart muscle occurs through an anterolateral approach in the fourth hypochondrium |
| Pulmonary valvotomy | Surgical manipulation that is performed through catheterization |
| Open valvotomy | To perform this operation, it is necessary to connect artificial blood circulation, and after that, to gain access to the heart muscle, the chest is opened. At the same time, the use of this type of operation is considered one of the most effective |
Preventive actions
To prevent the development of intrauterine pathological defects, you should pay attention to the health of the mother and limit her from exposure to dangerous factors that adversely affect the course of pregnancy. If a person is suspected of having SLA, then he needs to have scheduled visits to a cardiologist and follow preventive measures to prevent infective endocarditis.
Symptoms
The clinical picture can vary significantly depending on the severity of the stenosis and can even be asymptomatic, for example, if the pressure gradient between the heart and artery does not exceed 25 mm Hg. I don’t even prescribe treatment for such people.
The symptom complex usually manifests itself in the form of an increasing and decreasing ejection noise, cyanosis of the skin, the development of a “heart hump” and various signs of heart failure, including:
- causeless fainting;
- swelling;
- liver enlargement;
- frequent chest pain and discomfort (“angina pectoris”);
- dyspnea.
General information about heart defects in children
Heart disease
- a violation of the anatomical structure of the walls or valves of the heart, as well as the blood vessels that enter or exit it. Cardiac function and hemodynamics in the entire circulatory system are impaired.
Depending on the reasons for development, there are congenital
and
acquired vices
.
It is believed that congenital ones appear during the first weeks of pregnancy during the “initial formation” of future life. The reasons for the development of defects have not been studied reliably, but they predispose to them:
- genetic diseases (50% of children with Down syndrome suffer from this disorder);
- diabetes mellitus in a pregnant woman;
- bad habits of the expectant mother (half of children with fetal alcohol syndrome (FAS) have heart defects);
- infections (a mother who has had rubella in the first trimester will almost always have a child with severe pathology);
- taking medications prohibited for pregnant women;
- phenylketonuria in an expectant mother.
However, heart disease does not always develop from birth. It can manifest itself as a complication of diseases suffered in childhood (rheumatism, influenza, tonsillitis) in severe forms. This disorder is called an acquired defect.
hearts.
Tests and diagnostics
In case of narrowing of the blood-expelling structures of the heart or pulmonary artery, you should consult a doctor - a cardiologist who can assess the scale and nature of the pathological changes. During examination, patients may be diagnosed with:
- hypertrophy on palpation;
- signs of systolic overload of the right ventricle on the electrocardiogram - deviation of the electrical axis of the heart to the right, displacement of the ST segment by 2-5 mm below the isoline and a negative deep T wave, although more often the data obtained are within normal limits;
- bifurcation of the second heart sound;
- a hard ejection noise, a click and a decreasing ejection noise are heard in the second intercostal space with valvular stenosis or the fourth intercostal space with subvalvular stenosis of the pulmonary trunk in patients in a forward leaning position when using a stethoscope;
- the noise becomes louder during the Valsalva maneuver and during inspiration, and can lengthen and intensify as the stenosis progresses;
- ECG usually reveals hypertrophy of the walls of the right ventricle;
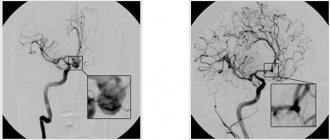
- using Doppler echocardiography, it is possible to detect pronounced turbulent blood flow at the level of the pulmonary valve and obtain an image of the narrowing, establish the severity of the patient’s condition and the pressure gradient - if it does not exceed 35 mm Hg, then the damage is considered mild, if within 35-65 mm Hg - moderate, over 65 mmHg - severe.
Patients may need periodic cardiac ultrasounds to monitor possible progression of stenosis (narrowing).
Diagnosis of heart defects in children
During the initial examination, a pediatrician, neonatologist or pediatric cardiologist conducts an examination and auscultation of possible heart murmurs. The presence of swelling, shortness of breath, heart rhythm disturbances, and problems with physical or intellectual development are checked. Based on the results of the inspection, the question of the necessary examination is decided.
Cardiac echocardiography (EchoCG) – combines cardiac ultrasound and cardiogram. The method determines the rhythmogram and structural changes in the heart. EchoCG is an informative method.
Radiology shows the actual size of the heart, its chambers and the relationship of the organ to the size of the chest.
Coronary angiography – a catheter is inserted through the veins or arteries in the arm, groin, or neck (vein only) and reaches the heart. Then a contrast agent is passed through it. This method determines the contractile function of the heart.
Medical equipment uses expert-class equipment from world-famous manufacturers.
The task of the Children's Medical Department is to provide a full range of medical care from prevention to treatment, when symptoms of a defect appear from birth to 18 years.
In our children's department, appointments are conducted by doctors who have undergone special training to identify health problems in children and infants, taking into account all age-related characteristics.
Pediatric doctors at the Paracelsus Clinic work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Parents play a big role in the early diagnosis of heart defects in children. The direction in which the preliminary examination will be carried out depends on how closely the parents monitor the health of their child and how correctly they can describe his condition to the doctor.
Pulmonary stenosis in newborns
In newborns, a severe (critical) form of stenosis causes heart failure and a bluish tint to the skin, and a pronounced heart murmur raises suspicion.
The pressure gradient can disappear over time and be compensated by the internal forces of the body, however, the condition of the resulting post-stenotic aneurysmal dilatations of small vessels can be complicated by thrombosis and arteritis , causing pulmonary hemorrhages. Severe stenoses can lead to death, both in infancy and in subsequent periods of life.
Total anomalous pulmonary venous drainage
The word "abnormal" means "wrong." With this defect, the pulmonary veins (and there are four of them), which should flow into the left atrium
, do not fall into it, i.e. don't connect with him. There are a lot of options for their wrong fit.
There is “partial” anomalous drainage - this is when one or two of the four veins flow into the right atrium (the most common option), and in the vast majority of cases it is combined with atrial septal defects, and we talked about this in the chapter on ASD.
Complete or total anomalous pulmonary venous drainage (TAPVD) is a completely different matter. With this defect, all four pulmonary veins from both lungs are connected into one wide collector vessel. This collector of arterial blood oxidized in the lungs does not fuse with the left atrium, as it should, but connects to the venous system of the body, usually through a large vein. Arterial blood thus bypasses the heart and enters the great veins and the right atrium. Only here, having passed through the atrial septal defect, will it end up where it should be initially - in the left atrium, and then makes its usual journey through the systemic circulation. It is difficult to imagine that this could even happen. But children with this defect are born full-term, and the heart copes with this situation for some time. However, this time may be very short.
Firstly, the life of a child depends on the size of the interatrial communication - the smaller it is, the more difficult it is for arterial blood to reach its destination in the left half of the heart.
Secondly, in this left half of the heart, a significant part of the blood is simply venous, i.e. unoxidized, and it will again be pumped into the large circle. Thus, partially venous blood begins to circulate in the child’s arteries, and he becomes “blue”, i.e. the color of the skin, and especially the tips of the fingers and mucous membranes (lips, mouth) is bluish. This is cyanosis, and we’ll talk about its causes, manifestations and consequences later.
With complete anomalous drainage, the cyanosis may not be very pronounced, but it is there, and it is usually noticeable soon after birth.
In most cases, the condition of children with complete anomalous pulmonary venous drainage is “critical” from the very beginning of life. If nothing is done, they will die within a few days or months.
Surgical treatment exists, and the results today are quite encouraging. The operation is quite complex, it is performed on an open heart and consists in the fact that the common collector of the pulmonary veins is sutured to the left atrium, and the hole in the atrial septum is closed with a patch. Thus, after the operation, normal blood circulation is restored in two separated circles.
Sometimes an emergency option is acceptable - widening the defect during probing as the first, life-saving stage, which allows you to somewhat delay the main intervention.
We will not touch here on many details associated with various types of vice and methods for correcting it. But we only want to emphasize that children with this defect need immediate specialized
help, which is completely real today.
The long-term results of the operation are quite good - after all, the main defect has been eliminated. However, children should be under the supervision of cardiologists because complications such as rhythm disturbances or narrowing of the pulmonary veins at the suture sites are possible (this occurs because the heart continues to grow after such a major operation). And again we want to emphasize: this child is not disabled. He must lead an absolutely normal life, and the sooner the operation is performed, the faster everything will be forgotten.
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
Diet for pulmonary stenosis
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Pulmonary artery stenosis requires a special diet, most often prescribed number 10 with a significant reduction in salt content, which ensures normal functioning of the cardiovascular system. In addition, it spares the gastric and urinary systems. Typically the following products are preferred:
- unhealthy and whole grain bread;
- various types of dietary soups;
- obligatory vegetable side dishes;
- eggs;
- fruit sauces and salads;
- low-fat dairy products.
Spicy, salty, spicy and smoked foods, as well as animal fats, are prohibited. Drinks that contain caffeine and alcohol. It is recommended to limit fats, even of vegetable origin.