Why is fever dangerous in children, and how to deal with it?
advises a medical pediatrician. Fever is the most common sign of the development of infectious and some other diseases in children.
Many things can cause a child to have a fever, from common childhood illnesses such as chicken pox and tonsillitis to reactions to vaccinations. An increase in body temperature is an innate protective mechanism by which the body stimulates the functioning of the protective factors of the immune system. Also, the increased temperature of the internal environment of the body itself can lead to inactivation or death of pathogens of many diseases. Remember that everyone's body temperature normally fluctuates 1-2 degrees throughout the day and may vary depending on age, activity level and other factors.
So rising temperatures are not a “problem.” This is an indicator that some kind of attack by microbes, viruses or other factors has occurred on the body, and the body reacts to it, gives a “response”. It is much worse when bacteria or viruses attack, but the temperature does not rise (i.e. there is no immune response, or it is insufficient).
Modern approaches to the treatment of fever in children with infectious pathology
Fever is one of the most common symptoms of infectious diseases in children and one of the most common reasons why parents seek help from a pediatrician. Fever is the most common reason for the use of medications.
When measuring body temperature in the armpit, a body temperature of 37.0°C or higher is usually considered elevated. However, it should be borne in mind that values of 36.0–37.5 ° C can be considered normal. A child’s normal body temperature fluctuates during the day within 0.5–1.0°C, increasing in the evening. Axillary temperature is 0.5–0.6°C lower than rectal temperature.
Fever is a nonspecific protective-adaptive reaction of the body that occurs in response to exposure to various pathogenic stimuli and is characterized by a restructuring of thermoregulation processes, which leads to an increase in body temperature.
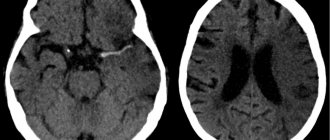
Elevated body temperature reduces the viability of some pathogenic microorganisms and enhances the specific and nonspecific components of immunity. However, an increase in temperature can play an adaptive role only when it rises to a certain limit. With high hyperthermia (40–41°C), an increase in the intensity of metabolic processes is observed. Despite the increased work of the respiratory and cardiovascular systems (for every degree the body temperature rises above 37 °C, the respiratory rate increases by 4 per 1 min, the heart rate (HR) increases by 10–20 per 1 min), increased oxygen delivery can fail to meet the growing tissue needs for it, which leads to the development of tissue hypoxia and disruption of the distribution of vascular tone. First of all, the functions of the central nervous system are affected, which is often manifested by the development of convulsive syndrome - febrile seizures (especially in young children with perinatal damage to the central nervous system). With hyperthermia, cerebral edema may develop, when the child’s condition sharply worsens and depression of the central nervous system occurs.
In children with malnutrition, respiratory failure, as well as with lesions of the central nervous system, adverse health consequences can develop with a relatively moderate degree of increase in body temperature (38.5–39°C).
Classification of fever
- by etiological factor:
- infectious;
- non-infectious;
- by duration:
- ephemeral (up to several days);
- acute (up to 2 weeks);
- subacute (up to 6 weeks);
- chronic (over 6 weeks);
- according to the presence of inflammation:
- inflammatory;
- non-inflammatory;
- according to the degree of temperature increase:
- low-grade fever (up to 38°C);
- febrile (38.1–39°C);
- febrile high (39.1–41°C);
- hyperthermic (over 41°C).
Mechanism of fever
An increase in body temperature of infectious origin develops in response to exposure to pyrogens of a viral or bacterial nature and is most common.
Fever is based on the ability of granulocytes and macrophages to synthesize and release endogenous protein pyrogens, interleukins (IL-1, IL-6), tumor necrosis factor (TNF) and interferons when activated. The target for the action of endogenous pyrogens is the thermoregulatory center, which regulates the mechanisms of heat production and heat transfer, thereby ensuring normal body temperature and its daily fluctuations.
IL-1 is considered the main initiating mediator in the mechanism of fever development. It stimulates the secretion of prostaglandins, amyloids A and P, C-reactive protein, haptoglobin, α1-antitrypsin and ceruloplasmin. Under the influence of IL-1, the production of IL-2 by T lymphocytes is initiated and the expression of cellular Ig receptors increases, as well as increased proliferation of B lymphocytes and stimulation of antibody secretion. Disruption of immune homeostasis during infectious inflammation ensures the penetration of IL-1 through the blood-brain barrier, where it interacts with receptors of neurons of the thermoregulation center. In this case, cyclooxygenase (COX) is activated, which leads to an increase in the intracellular level of cyclic adenosine-3,5-monophosphate (cAMP) and a change in the intracellular Na/Ca ratio. These processes underlie changes in the sensitivity of neurons and a shift in the thermoregulatory balance towards increased heat production and decreased heat transfer. A new, higher level of temperature homeostasis is established, which leads to an increase in body temperature.
The most favorable form of the body's reaction to infectious diseases is an increase in body temperature to 38.0–39 ° C, while its absence or febrile high fever indicates a reduced reactivity of the body and is an indicator of the severity of the disease. When fever develops during the day, the maximum increase in body temperature is recorded at 18–19 hours, the minimum level is in the early morning. Information about the characteristics and dynamics of fever throughout the course of the disease has important diagnostic value. For different diseases, febrile reactions can occur in different ways, which is reflected in the shapes of temperature curves.
Clinical variants of fever
When analyzing the temperature reaction, it is very important to evaluate not only the magnitude of its rise, duration and daily fluctuations, but also to compare these data with the condition and well-being of the child, and the clinical manifestations of the disease. This is necessary to select the correct treatment tactics for the patient, as well as to conduct further diagnostic searches.
First of all, it is necessary to assess the clinical signs of compliance of heat transfer processes with an increased level of heat production, because Depending on the individual characteristics of the body, fever, even with the same degree of increase in body temperature in children, can occur differently.
If the child responds adequately to an increase in body temperature, heat transfer corresponds to increased heat production, which is clinically manifested by normal health, pink or moderately hyperemic skin color, moist and warm to the touch (the so-called “pink fever”). Tachycardia and increased respiration correspond to the level of body temperature, the rectal-digital gradient does not exceed 5–6 °C. This type of fever is considered prognostically favorable.
If the child’s response to an increase in body temperature is inadequate and heat transfer is significantly less than heat production, then clinically there is a pronounced disturbance in the child’s condition and well-being, chills, pale, marbled skin, nail beds and lips with a cyanotic tint, cold feet and palms (the so-called “pale fever” ). There is persistent persistence of hyperthermia, excessive tachycardia, shortness of breath, possible delirium, convulsions, and a rectal-digital gradient of more than 6 °C. This course of fever is prognostically unfavorable and is a direct indication for emergency care.
Among the clinical variants of the pathological course of fever, hyperthermic syndrome is distinguished, in which there is a rapid and inadequate increase in body temperature, accompanied by impaired microcirculation, metabolic disorders and progressively increasing dysfunction of vital organs and systems. The risk of developing such conditions is especially high in young children, as well as those with a burdened premorbid background. The younger the child is, the more dangerous a rapid and significant rise in body temperature is for him due to the possible development of progressive metabolic disorders, cerebral edema, and impairment of vital functions. If a child has serious diseases of the cardiovascular and respiratory systems, fever can lead to the development of their decompensation. In children with pathologies of the central nervous system (perinatal encephalopathy, epilepsy, etc.), seizures may develop against the background of elevated body temperature.
Febrile seizures occur in 2–4% of children, most often between 12–18 months of age. They usually occur with a rapid rise in temperature to 38–39 °C and higher at the very beginning of the disease. Repeated seizures can develop in a child at other temperatures. If a child experiences febrile seizures, it is necessary to first rule out meningitis. In infants with signs of rickets, a calcium level test is indicated to exclude spasmophilia. Electroencephalography is indicated after the first episode only for prolonged, repeated or focal seizures.
Tactics of management and treatment of children with fever
Fighting fever is one of the most important components of complex therapy of the underlying disease. It is carried out against the background of etiotropic (antimicrobial, antiviral, antiparasitic) and syndromic therapy.
In case of febrile conditions in children, measures taken should include:
- half-bed or bed rest depending on the level of increase in body temperature and the child’s well-being;
- a gentle, dairy-vegetable diet, feeding depending on appetite. It is advisable to limit the intake of fresh milk due to possible hypolactasia at the height of the fever. Drink plenty of fluids (tea, fruit juice, compote, etc.) to ensure adequate heat transfer due to increased sweating.
Therapeutic tactics for increased body temperature depend on the clinical variant of the fever, the severity of the temperature reaction, and the presence or absence of risk factors for the development of complications.
The decrease in body temperature should not be critical; it is not necessary to achieve normal levels; it is enough to lower the temperature by 1–1.5°C. This leads to an improvement in the child’s well-being and allows him to better tolerate a feverish state.
In case of “pink fever”, it is necessary to undress the child, taking into account the air temperature in the room, put “cold” on large vessels (inguinal, axillary areas), if necessary, wipe with water at room temperature, which is sufficient to reduce body temperature or significantly reduces the amount of pharmacotherapy. Rubbing with cold water or vodka is not recommended, as it can lead to spasm of peripheral vessels and a decrease in heat transfer.
Indications for the use of antipyretic drugs. Considering the protective-adaptive mechanism of fever in children and its positive aspects, antipyretics should not be used for any temperature reaction. If the child does not have risk factors for developing complications of a febrile reaction (febrile convulsions, cerebral edema, etc.), there is no need to reduce body temperature below 38–38.5°C using antipyretic drugs. However, if, against the background of fever, regardless of its severity, there is a deterioration in the general condition and well-being of the child, chills, myalgia, pale skin, and other symptoms of toxicosis, antipyretics are prescribed immediately.
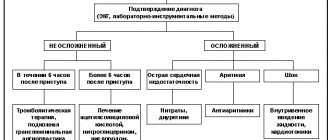
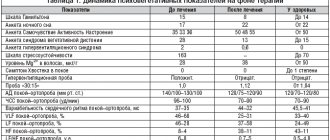
In children at risk with an unfavorable course of fever with severe intoxication, impaired peripheral circulation (“pale fever”), antipyretic drugs are prescribed even at low-grade fever (above 37.5 ° C), for “pink fever” - at a temperature exceeding 38, 0°C (Table 1).
Antipyretics are mandatory, along with other measures, for hyperthermic syndrome, when a rapid and inadequate increase in body temperature occurs, accompanied by impaired microcirculation, metabolic disorders and progressively increasing dysfunction of vital organs and systems.
It should be noted that medications to reduce fever should not be prescribed in a course, since this changes the temperature curve and makes diagnosing infectious diseases very difficult. The next dose of an antipyretic drug is needed only when the body temperature rises again to the appropriate level.
Principles for choosing antipyretic drugs in children. Antipyretics are most widely used in children compared to other drugs, so their choice is based primarily on safety rather than effectiveness. The drugs of choice for fever in children, according to WHO recommendations, are paracetamol and ibuprofen. Paracetamol and ibuprofen are approved in the Russian Federation for over-the-counter use and can be prescribed to children from the first months of life both in a hospital and at home.
It should be noted that paracetamol has an antipyretic, analgesic and very weak anti-inflammatory effect, because implements its mechanism primarily in the central nervous system and does not have a peripheral effect. Ibuprofen (Nurofen for children, Nurofen) has more pronounced antipyretic, analgesic and anti-inflammatory effects, which is determined by its peripheral and central mechanisms. In addition, the use of ibuprofen (Nurofen for children, Nurofen) is preferable if the child has a pain syndrome along with fever, for example, fever and sore throat with sore throat, fever and ear pain with otitis media, fever and joint pain with pseudotuberculosis, etc. The main problem with the use of paracetamol is the danger of overdose and associated hepatotoxicity in children over 10–12 years of age. This is due to the peculiarities of the metabolism of paracetamol in the child’s liver and the possibility of the formation of toxic metabolites of the drug. Ibuprofen can rarely cause undesirable effects from the gastrointestinal tract, respiratory system, extremely rarely from the kidneys, changes in the cellular composition of the blood.
However, with short-term use of recommended doses (Table 2), the drugs are well tolerated and do not cause complications. The overall incidence of adverse events associated with the use of paracetamol and ibuprofen as antipyretics is approximately the same (8–9%).
Prescription of Analgin (metamizole sodium) is possible only in case of intolerance to other antipyretic drugs or if parenteral administration is necessary. This is associated with the risk of adverse reactions such as anaphylactic shock, agranulocytosis (with a frequency of 1:500,000), prolonged collapsing state with hypothermia.
It should be remembered that drugs with a strong anti-inflammatory effect are more toxic. It is irrational to use powerful anti-inflammatory drugs - nimesulide, diclofenac - to reduce body temperature in children; they are approved only for prescription use.
Acetylsalicylic acid is not recommended as an antipyretic for children, as it can cause Reye's syndrome (severe encephalopathy with liver failure) in case of influenza and other acute respiratory viral infections and chicken pox. You should not use amidopyrine and phenacetin, which are excluded from the list of antipyretic drugs due to high toxicity (development of seizures, nephrotoxicity).
When choosing medications to reduce fever in children, it is necessary to take into account, along with safety, the convenience of their use, i.e., the availability of children's dosage forms (syrup, suspension), as well as cost.
Therapeutic tactics for various clinical types of fever in children. The choice of starting antipyretic drug is primarily determined by the clinical type of fever. If a child tolerates an increase in temperature well, his health suffers slightly, the skin is pink or moderately hyperemic, warm, moist (“pink fever”), the use of physical cooling methods allows one to reduce body temperature and, in some cases, avoid pharmacotherapy. When the effect of using physical methods is insufficient, paracetamol is prescribed in a single dose of 15 mg per kg of body weight or ibuprofen in a dose of 5-10 mg per kg of body weight taken orally in suspension (Nurofen for children) or tablet form (Nurofen) depending on age child.
For “pale fever,” antipyretics should be used only in combination with vasodilators. It is possible to use Papaverine, No-shpa, Dibazol. In case of persistent hyperthermia with a violation of the general condition, the presence of symptoms of toxicosis, there is a need for parenteral administration of vasodilators, antipyretics and antihistamines. In such cases, use a lytic mixture:
- 2% Papaverine solution intramuscularly in a single dose of 0.1–0.2 ml for children under 1 year of age; 0.2 ml per year of life for children over one year of age;
- 50% solution of Analgin (metamizole sodium) intramuscularly, in a single dose of 0.1–0.2 ml per 10 kg of body weight for children under 1 year of age; 0.1 ml per year of life for children over 1 year of age
- 2.5% solution of Pipolfen (or Diprazine) intramuscularly in a single dose of 0.5 or 1.0 ml.
Children with intractable fever should be hospitalized.
Hyperthermic syndrome, in which there is a rapid and inadequate increase in body temperature, accompanied by impaired microcirculation, metabolic disorders and progressively increasing dysfunction of vital organs and systems, requires immediate parenteral administration of antipyretics, vasodilators, antihistamines, followed by hospitalization and emergency syndromic therapy.
Thus, when treating a child with fever, the pediatrician should remember:
- antipyretic drugs should not be prescribed to all children with elevated body temperature; they are indicated only in cases of infectious-inflammatory fever when it has an adverse effect on the child’s condition and threatens the development of serious complications;
- drugs to reduce fever should not be prescribed in a course; repeated administration of an antipyretic drug is indicated only when the temperature next rises to a level requiring drug correction;
- Among antipyretic drugs, preference should be given to ibuprofen (Nurofen for children, Nurofen), which has the lowest risk of unwanted effects;
- the appointment of Analgin (metamizole sodium) is possible only in case of intolerance to other antipyretic drugs or if their parenteral administration is necessary.
For questions regarding literature, please contact the editor.
What is a fever?
The normal temperature for babies and children is around 36.4°C, but this may vary slightly from child to child.
- Low-grade fever is an increase in temperature from 36.7 to 38 degrees.
- Fever is a high temperature of 38 C or more.
The following symptoms appear when you have a fever:
- Your baby's forehead, back, or stomach feels hotter than usual.
- The surface of the skin becomes sweaty (moist) and sticky.
- The baby's cheeks and sometimes forehead turn red.
To measure temperature, it is best to use a safe digital thermometer without mercury filling.
How to measure a child's temperature:
- The child's armpit should be clean and dry! If it is wet, the thermometer will show an inflated result!
- Move your child's arm to the side and place the thermometer in the upper armpit.
- Gently place your hand against your body and keep it pressed while taking the temperature.
- Leave the thermometer in place for as long as indicated in the instructions. Some digital thermometers beep when the temperature measurement is complete.
- Take out the thermometer. The display will show the baby's body temperature.
- If your child has just had a bath or has been wrapped tightly in a blanket, wait 10 minutes before taking their temperature.
- Professional infrared thermometers allow you to instantly measure body temperature. If there is a need to measure the temperature as accurately as possible, but there is no professional thermometer at hand, the most accurate results are obtained by measuring the temperature rectally.
What to do if your child has a high temperature
The child must be kept at home and supervised. The temperature should drop within 3 or 4 days.
After vaccination, the temperature can remain normal for up to 48 hours.
What do we have to do:
- if the child is less than 6 months old, call a doctor immediately
- Give your baby plenty of fluids to drink (or continue breastfeeding)
- monitor signs of dehydration
- feed if the baby wants to eat
- Regularly monitor your child's condition at night
- give the child antipyretics prescribed by the doctor
Medium form
Moderate severity of COVID-19 is characterized by a significant deterioration in well-being. In this case, pneumonia always develops, so hospitalization is indicated. After the first symptoms associated with fever and severe weakness appear, shortness of breath develops and pain in the muscle joints appears.
In the days following coronavirus infection, the following manifestations are observed:
- 1 day. Body temperature rises to 37.5°C. Headaches and discomfort in joints and muscles occur. There is nasal congestion.
- 2-4 days. The general condition worsens significantly, dyspeptic disorders and dizziness occur. Body temperature can rise to 38.5°C, so you need to lower it with special medications. There is a constant sore throat and bouts of prolonged non-productive cough, which indicates the spread of infection to the lungs. Almost always, a sick person ceases to smell.
- 5-6 day. The patient's condition worsens. Additionally, compressive pain appears in the chest. The body temperature does not fall below 38°C and must be constantly brought down with antipyretic drugs. These symptoms are evidence of the development of viral pneumonia, which requires a full examination and appropriate treatment.
- 7-14 days. With the correct course of treatment, the patient's condition improves. Cough and nasal congestion disappear, body temperature normalizes.
After the condition has stabilized, testing is carried out. If the result is negative, the person is considered recovered. But it may take another couple of weeks for complete recovery.
What not to do when the temperature rises
- Do not undress your child or cool him or her with blows or rubs; fever is a natural and healthy response to infection. Hypothermia can lead to complications from the infection.
- Do not cover your baby with a warm blanket or wrap him up, as this may cause heat stroke. Just cover your baby with a sheet or light blanket.
- Do not give aspirin to children under 16 years of age. Absolutely never! This may be due to a rare but dangerous disease called Reye's syndrome.
- In children under one year of age, medications available in the form of rectal suppositories are recommended to reduce fever.
- Do not self-medicate. For young children, the dose of drugs and the frequency of their use should be calculated individually; the prescription can only be made by a doctor after diagnosis.
Stopping blood circulation and breathing
Call an ambulance (resuscitation) immediately!
- Ensuring airway patency:
- if a cervical spine injury is suspected, the neck is immobilized
- clean the oropharynx (pear, finger)
- eliminate obstruction caused by retraction of the tongue or compression by soft tissues of the neck, push the lower jaw forward or raise the chin.
- improving airway patency. The head is positioned along the midline. Children, unlike adults, should not throw their heads back too much, because in children this can lead to airway obstruction. A towel folded several times is placed under the back of the head (for adults, a cushion under the shoulders).
- Ventilation is started using the mouth-to-mouth method (mouth to mouth and nose) and indirect chest massage. The effectiveness of ventilation is assessed by chest excursion.
Ventilation is performed so that each breath lasts 1.0-1.5 s. The frequency of compressions on the chest of a newborn is at least 120 per minute, the ratio of the frequency of insufflations and compressions is 1:3. In older children, the frequency of pressure is at least 100 per minute. The child is placed on a hard surface and chest compressions are immediately started. The ratio of the frequency of inflation to the frequency of chest compressions is 1:5.
In infants, indirect massage is carried out in two ways: pressing on the chest with the middle and index fingers of one hand, or clasping the child with both hands so that the thumbs are located on the middle third of the sternum, and the rest support the back.
In both cases, pressure is applied to the lower third of the sternum (about a finger's width below the nipples). In children 1-2 years old, I press on the sternum with the protrusion of the palm of one hand. Older children and adults use two hands. In both cases, pressure is applied to the lower third of the sternum (approximately two finger widths above the xiphoid process). Depth of descent of the sternum: children under one year old: 1.5-2.5 cm, up to 7-8 years old - 3-5 cm, older - 4-6 cm. The effectiveness of indirect massage is assessed by the pulse in the carotid and femoral arteries. Resuscitation measures must be continued until doctors arrive!
When should you seek emergency medical help?
It is necessary to call a doctor or ambulance in the following cases:
- The child is less than 3 months old and has a temperature of 38°C or higher
- The baby is between 3 and 6 months old and has a temperature of 39°C or higher
- Against the background of fever, rash, vomiting, and diarrhea appeared
- Fever lasts for 5 days or more
- The child refuses the breast, does not eat, behaves unnaturally
- The child has signs of dehydration: dry diapers, sunken eyes, crying without tears.
Still have questions?
Get an online consultation from leading pediatricians in St. Petersburg!
A professional and experienced pediatrician will answer your questions.
Medical care for a child without leaving home at a convenient time.
sign up for a consultation
A Skype consultation lasts 45 minutes.
First aid for choking
- Foreign bodies in the respiratory tract
Most often, toys and food (candies, chewing gum, nuts) get into the respiratory tract. Inflatable toys are dangerous for young children; after biting through such a toy and being frightened by the cotton, the child can inhale parts of it.
- Signs: the child is suffocating and cannot scream, makes whistling noises, tries in vain to cough, the face begins to turn blue.
- What to do: Call emergency services as quickly as possible. Then proceed with first aid.
Place your baby face down on your arm so that his chest is in your palm, and cup his lower jaw with your thumb and forefinger. Sit down and rest your baby's hand on your thigh or knee. Lower the child's head below his body. Within 5 seconds, with the palm of your free hand, apply 4 sharp blows to the back between the shoulder blades. Place your baby face up on your other arm. Place your hand on your thigh or knee. Keep the baby's head lower than his body. Within 5 seconds, press your fingers sharply 4 times on the chest just below the nipples. Place the child face down on the other hand again and give him 4 more blows to the back. In children older than one year, sharp thrusts are performed in the upper abdomen. Continue alternating the two techniques (4 blows to the back, 4 pressures to the chest) until the foreign body is pushed out. If the child is unconscious, hold the child's head and neck firmly with your hand and without bending the child's back, place the child face up on a hard surface and expose the child's chest. Use your thumb and forefinger to open your child's mouth and press down on the tongue with your thumb.
If you notice a foreign body in your throat and see that it can be removed, do so. Look closely and listen to see if the child is breathing. To prevent your tongue from closing your windpipe, lift your chin and move your head back. The child's mouth should remain open. Place your ear toward your baby's mouth to hear his breathing and see if his chest moves. Look closely and listen for no more than 5 seconds. If the child is not breathing, begin artificial respiration and cardiopulmonary resuscitation. Even if you managed to clear the child’s airways from the foreign body and the child seems completely healthy to you, consult a doctor.
What not to do: Do not try to grab an object stuck in your child's throat with your fingers: you can push it even deeper. If the child stops breathing, do not begin resuscitation until the airway is clear.
2. Attack of bronchial asthma
- Symptoms: cough, difficulty breathing, wheezing, up to severe respiratory problems. When to call a doctor: if (1) signs of asthma appear in a child for the first time, (2) the treatment prescribed by the doctor does not help, (3) the body temperature rises above 39°C, call a doctor.
- What to do: Reassure and reassure your child: anxiety can only make an asthma attack worse. Give your child the medications recommended by your doctor. Give your child little and often water.
3. False croup
False croup occurs in the form of difficulty breathing (mainly exhalation), hoarseness, and a “barking” cough. First aid procedure:
- Give an elevated body position;
- Provide access to fresh air;
- Call a doctor;
- Alkaline inhalations (1 tablespoon of soda per 1 liter of water);
- Distraction procedures - warm foot or hand baths;
- You can give your child an antihistamine in an age-appropriate dosage (pipolfen, suprastin, tavegil, etc.).
What not to do: the use of herbs and honey in any form, as well as mustard plasters, is contraindicated.
4. Fainting
Symptoms are “harbingers”: dizziness, nausea, darkness before the eyes, a feeling of faintness, failure, detachment. First aid procedure:
- Sit your child down and tilt his head down below his knees.
- Unfasten your collar, belt and other clothing that restricts breathing.
- If the child has lost consciousness, lay him on a flat surface and raise his legs 20-30 cm above the level of the body.
- Pat your cheeks, rub your temples.
- Let the vapors of ammonia, or vinegar, or another strong-smelling substance inhale (for children over 3 years old).
- Turn the child's head to the side to prevent suffocation in case of vomiting.
- Check if there is breathing and pulse (heartbeats); if not, call emergency help and perform artificial respiration.
If fainting lasts more than 5 minutes, call emergency services. After you come to your senses, give yourself some hot sweet tea to drink. Although fainting spells lasting less than 5 minutes usually do not harm the baby, it is important to find out why it occurs. Even if fainting occurs for the first time, be sure to consult a doctor as soon as possible!
Signs of particularly dangerous diseases accompanied by fever
Fever can be a sign of serious illnesses such as meningitis, urinary tract infection and sepsis. It is necessary to urgently call an ambulance or take the child to the hospital emergency room if he has:
- There is tension and stiffness in the neck muscles,
- A rash has appeared that does not go away when you press on it with a finger
- The child is very irritated by light,
- The attack of fever does not go away, the child “shakes” with chills
- The child has unusually cold hands and feet
- Your baby has pale, mottled, blue, or gray skin
- The baby's crying has become weak, moaning, and does not look like usual
- The baby is sleepy, lethargic, and difficult to wake up
- The child has difficulty breathing, the stomach is pulled in under the ribs when breathing
- In a newborn baby, the fontanel on the top of the head has become bulging
What should you do if your child has a seizure? Seizures are a very serious side effect of fever in some children. Febrile seizures occur in 2–4% of all children under 5 years of age. Not all seizures cause sudden muscle twitching. Some seizures look like “fainting.” If your child develops a seizure, do the following:
- Place your baby on his side.
- Do not put anything in your child’s mouth, even if “experienced” grandmothers recommend doing so.
- Call an ambulance immediately if the attack lasts more than five minutes.
- If the attack lasts less than five minutes, call your doctor or make an emergency visit to your doctor.