Classification of pathological condition
Mitral valve prolapse is a disease that can be congenital or acquired. In addition, the defect is classified into audible and silent. In the latter case, the disease is detected only during examination by a cardiologist.
Classification according to the degree of protrusion of the atrioventricular valve leaflets into the atrium cavity:
- 1st degree – up to 0.5 cm;
- 2nd degree – from 0.5 to 0.9 cm;
- 3rd degree – more than 1 cm.
The disease is most often diagnosed at the age of 5-7 years. Due to the fact that modern examination methods are used today, such as echocardiography, the disease is diagnosed at an early age. According to studies, it was found that up to 15% of children suffer from the pathological condition in question.
Mitral valve prolapse
18.09.2014
Mitral valve prolapse
General information about mitral valve prolapse, its clinical picture and diagnosis.
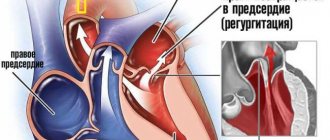
Mitral valve prolapse is sagging (bending) of the mitral valve leaflets into the left atrium.
Mitral valve prolapse syndrome, or Barlow's syndrome , was described by J. Barlow in 1963 and is extremely common - in 5-10% of people in the population.
It is necessary to distinguish between true prolapse of the valves and their wave-like sagging (billowing).
In many cases, mitral valve prolapse is asymptomatic (has no symptoms); in some cases, (heart rhythm disturbances), the presence of a characteristic noise when listening to tones , chest pain , and shortness of breath can be observed . Emotional lability, fatigue and other nonspecific clinical signs are also recognized as associated with mitral valve prolapse .
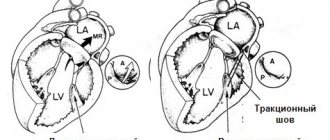
Prolapse, or sagging, of one or both cusps of the mitral valve during systole into the cavity of the left atrium is considered true only if it is recorded in two echocardiographic positions: apical four-chamber and parasternal along the long axis of the left ventricle.
Diagnosis of mitral valve prolapse is carried out during an echocardiographic study carried out in B-mode, M-mode, color and spectral Doppler modes.
In the expert practice of ultrasound examinations of the heart, only a combination of all modes allows one to obtain a holistic understanding of the nature of the process, the presence and severity of hemodynamic disorders.
In a number of countries, there is a rule to perform any surgical interventions in patients with prolapse syndrome under the guise of antibiotics in order to prevent complications.
Currently in our country there is overdiagnosis of mitral valve prolapse in children and adolescents.
This may be due to incorrect execution of the research procedure (technique) - incorrect identification of the apical position of the heart. In addition, a slight sagging of the base of the anterior leaflet of the mitral valve in children and adolescents up to 3–5 mm is normal if it is not accompanied by pathological regurgitation. In addition, the valve leaflets and chords develop faster than the fibrous rings, therefore, sagging of the leaflets is more often recorded in childhood and adolescence.
It is necessary to distinguish between physiological mitral valve prolapse - without disrupting its function, and pathological mitral valve prolapse - with pathological mitral regurgitation.
Mitral valve prolapse syndrome is characterized by young age of patients - usually 20–50 years; predominance of women; the presence of noise - a “click” during auscultation, thickening of the valves and their systolic displacement during echocardiography, hypotension, as well as mitral regurgitation during Doppler examination, the degree of which exceeds physiological.
Myxomatous degeneration is not uncommon , signs of which are found in older patients - 40-70 years old, among whom males predominate. In these cases, pathological mitral regurgitation is detected by echocardiography, and there are pronounced changes in the leaflets that require cardiac surgical correction.
Myxomatous degeneration of the mitral valve leaflets, as one of the most common causes of mitral valve prolapse, can affect the leaflets of all heart valves, but the most common lesion is the mitral valve.
Over the past few years, the number of people suffering from this pathology has increased significantly throughout the world. Just 10 years ago, the majority of patients with myxomatous degeneration were patients with Marfan syndrome. Currently, the connection between unfavorable environmental factors and the use of a number of weight loss drugs in the occurrence of this pathology has been proven. The number of patients over 70 years of age suffering from myxomatous degeneration has increased significantly.
An echocardiographic examination clearly shows scalloped, “serpentine”, uneven, thickened cusps of the mitral valve. They prolapse into systole into the cavity of the left atrium. Rounded protrusions are formed on the valves, resembling small tumors - myxomas. This is where the name of this pathology comes from. You can often observe separation of the valve chords.
Most patients with myxomatous mitral valve degeneration demonstrate cardiac arrhythmias—atrial fibrillation or frequent ventricular extrasystole. The causes of arrhythmia are pathological mitral regurgitation against the background of myxomatous changes in the valve leaflets and, as a result, increased pressure in the cavity of the left atrium.
Patients with myxomatous degeneration require dynamic monitoring; those with significant mitral regurgitation require consultation with a cardiac surgeon.
The nature of changes in the structure of the mitral valve leaflets and the occurrence of pathological mitral regurgitation can contribute to infection of the valve. Differential echocardiographic diagnosis in this case may be difficult.
The differential diagnosis of myxomatous degeneration of valve leaflets should be made with infective endocarditis and Lamble's growths. Clinical and laboratory diagnostics play an important role in this. Thus, with myxomatous degeneration there is no inflammatory reaction recorded during laboratory testing.
Secondary mitral valve prolapse occurs in the following situations:
- Marfan syndrome is a mesenchymal dysplasia. It is accompanied by a characteristic appearance of the patient (“Marfan-like type”) - increased joint flexibility, aortoanular ectasia, frequent development of aortic aneurysm and intimal detachment of the aorta in the thoracic ascending region and myxomatous degeneration of the valves and subvalvular structures. In this case, all heart valves prolapse. The degree of prolapse is usually significant. Pathological valvular regurgitation is recorded.
- Hypertrophic cardiomyopathy. In this case, mitral valve prolapse is associated with increased pressure in the cavity of the left ventricle during systole. Prolapse is especially pronounced in patients with obstructive hypertrophic cardiomyopathy.
- Ehlers-Danlos syndrome - connective tissue dysplasia syndrome - is a hereditary defect of hemostasis with damage to collagen structures. Accompanied by increased joint flexibility, increased skin stretching, bleeding and prolapse of heart valves
- Dysfunction of the papillary muscle due to myocardial infarction or cardiac injury is accompanied by prolapse of the valve leaflet and significant mitral regurgitation.
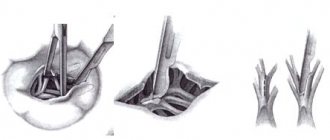
- Severance of the chords of the valve leaflet against the background of infective endocarditis, myxomatous degeneration, myocardial infarction, rheumatic lesions, etc. leads to prolapse of the leaflet and pathological valve regurgitation.
Assessment of the degree of mitral valve prolapse is carried out by assessing the severity of sagging of the leaflets:
- Minor mitral valve prolapse – 3–6 mm (1st degree mitral valve prolapse).
- Moderate mitral valve prolapse – 6–9 mm (2nd degree mitral valve prolapse)
- Significant mitral valve prolapse – more than 9 mm (grade 3 mitral valve prolapse).
It must be remembered that the degree of prolapse and the degree of mitral regurgitation may not correlate with each other . For example, when the chords are torn off at the end of the mitral valve leaflet, prolapse of up to 3 mm can be seen and grade 3–4 mitral regurgitation can be recorded.
Mitral valve prolapse is not a difficult diagnosis if echocardiographic examination is performed by an experienced specialist using high-resolution ultrasound systems.
What we offer for mitral valve prolapse:
The multidisciplinary medical professor offers you high-precision diagnostics of minor cardiac anomalies, including mitral valve prolapse, other cardiac and cardiovascular diseases only at an expert level.
Leading Russian specialists cooperate with us -
- Professor Sedov Vsevolod Parisovich,
- Professor Rybakova Marina Konstantinovna,
- Professor Khadzegova Alla Blalovna,
- Professor Tarasova Alla Alekseevna,
consulting cases of any diagnostic complexity in adults (V.P. Sedov, M.K. Rybakova, A.B. Khadzegova) and in children, including infants (A.A. Tarasova). Also, echocardiographic studies in adults in our clinic are carried out by doctors Natalya Vladimirovna Gerasimova and Natalya Mikhailovna Medvedeva. Echocardiography at home is performed by Oleg Evgenievich Isakov.
All echocardiographic studies in our center
(excluding procedures at home) are carried out on one of the world's best specialized ultrasound systems - Acuson Sequoia - 512 (Siemens AG, USA), equipped with all modern technologies and sensors.
See also:
- Echocardiography for adults
- Echocardiography for children
In addition to ultrasound examination of the heart, we also offer a wide range of services, including consultations with experienced cardiologists - Candidate of Medical Sciences Andrey Valentinovich Syrov and Candidate of Medical Sciences Olga Vladimirovna Morozova, electrocardiography, Holter ECG monitoring and 24-hour blood pressure monitoring, bicycle ergometry, any types of ultrasound and laboratory tests, consultations with various specialists.
A number of special programs for the prevention, diagnosis and treatment of the most common cardiovascular diseases have been created for you.
You can find more detailed information in other reviews and articles, as well as in the Services section.
We wish you good health and will be glad to see you at our clinic,
team of MPMC "Vascular Clinic on Patriarch's"
Etiology of the disease
The main cause of the disease is dysgenesis of connective tissue, which is part of many organs and, in particular, the valve apparatus.
Underdevelopment of connective tissue can be caused for various reasons. These could be infections, intoxications and occupational hazards that affected the body of a pregnant woman and the fetus. There is no clear answer to what causes the disease.
The acquired form of the pathological disease occurs after an inflammatory disease, in particular infective endocarditis, rheumatism.
Magazine "Child's Health" 2(5) 2007
Mitral valve prolapse (MVP), which is based on structural and functional disorders of the mitral valve of the heart, leading to bending of the valve leaflets into the cavity of the left atrium at the time of left ventricular systole, occupies a leading place in the structure of childhood diseases.
In recent years, the incidence of MVP has increased, therefore, despite the fact that the most characteristic auscultatory manifestation of the MVP phenomenon is the presence of systolic clicks (clicks) in combination with systolic murmur, with the widespread introduction of ultrasound research methods into practice, it became clear that even the absence of any - complaints, clinical symptoms and auscultatory changes do not exclude the possibility of its existence [1, 2].
At the present stage, the etiopathogenetic heterogeneity of the MVP phenomenon has been convincingly proven, manifested by clinical polymorphism and represented by such most recognized factors as, firstly, congenital microanomalies of the architecture of the valves, chords and atrioventricular ring, which over time, due to repeated microtraumas against the background of hemodynamic influences, become more pronounced, accompanied by excess production of collagen, predominantly type 3, in the valve stroma, and, secondly, the theory of a primary defect in the development of the connective tissue apparatus of the mitral valve, which is combined with an increase in the number of stigmas of disembryogenesis [2, 7, 14]. The clinical manifestations of MVP are influenced by: the degree of valve prolapse, the background against which MVP is detected, the nature of electrocardiographic abnormalities, and the presence of complications [8–10, 13].
Currently, the attention of clinicians is attracted by anomalies in the development of the choral apparatus of the heart, which occur in children in an average of 38% of cases [1]. The frequency of MVP, which is also a developmental anomaly, in children ranges from 3–5% at the age of up to 1 year, increasing by 14 years to 22–31% and depends on the diagnostic method [7]. Considering the prevalence of MVP among the pediatric population, pediatricians and cardiologists need to lean toward greater clinical vigilance and prevention of possible complications [1].
The purpose of this study was to study the effectiveness of complex therapy for clinical manifestations of MVP based on the results of prospective observation of children in the cardiology department of Children's Clinical Hospital No. 5 in Zaporozhye.
Material and methods
703 children (280 boys and 423 girls) from 3 to 18 years old were under observation. There were 108 (15.36%) children aged 3 to 7 years; from 8 to 12 years - 243 (34.57%); from 13 to 18 years old - 352 (50.1%) children.
All children underwent a comprehensive clinical examination, taking into account complaints, anamnestic data, results of physical examination methods, general clinical laboratory and instrumental (electrocardiography, echocardiography with Doppler ultrasound) research methods using standard methods. To diagnose concomitant somatic pathology, the children were examined by an otolaryngologist, neurologist, ophthalmologist, orthopedic surgeon, endocrinologist, dentist, and the girls were examined by a gynecologist. The nature of cardiac disorders was assessed according to ICD-10 recommendations.
The results obtained were processed using traditional statistical methods using Excel [4, 12].
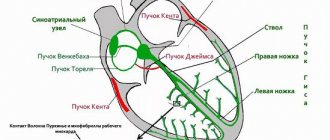
Depending on the clinical manifestations, all observed children were divided into 3 groups: MVP with rhythm disturbance and electrocardiographic symptoms (short P-Q syndrome, WPW syndrome, long QT syndrome), MVP as a manifestation of connective tissue dysplasia, and MVP with clinical signs of dysfunction of the autonomic nervous system .
The patients underwent echocardiographic examination in M- and B-modes and Doppler ultrasound in constant wave and pulse modes using an Aloka SSD-630 device. The generally accepted criteria for identifying PMC were used [1, 2, 7]. Also, two-dimensional echocardiography made it possible to detect morphological microanomalies in the structure of the valve apparatus that underlie the occurrence of mitral valve prolapse in the form of ectopic attachments or impaired distribution of tendon filaments, changes in the configuration and position of the papillary muscles, elongation of tendon filaments, and redundancy (enlargement) of the valve leaflets. Transmitral blood flow and mitral valve function were quantitatively assessed using Doppler ultrasound. Mitral valve regurgitation was diagnosed by the presence of turbulent systolic flow under the mitral valve leaflets in the left atrium. The following gradations of regurgitation magnitude were adopted:
— 1st degree (+) — systolic regurgitation in the area under the mitral valve;
— 2nd degree (++) — systolic regurgitation extends to 1/3 of the cavity of the left atrium;
— 3rd degree (+++) — spread of systolic regurgitation to 1/2 of the cavity of the left atrium;
— 4th degree (++++) — spread of regurgitation to more than 1/2 of the cavity of the left atrium [1, 7].
Results and discussion
Over the past five years, according to our observations, the number of children with MVP has increased in dynamics from 18.5% in 2002 to 29% in 2006, which is explained by both the expansion of the capabilities of ultrasound diagnosis of MVP (EchoCG) and the increase in the prevalence of connective dysplasia syndrome tissues with manifestations of dysfunction of the autonomic nervous system in children.
As a result of the study, it was established that in adolescents MVP is diagnosed significantly more often than in other age groups, with a predominance in girls in a ratio of 2: 1. In other groups of children studied, this pathology occurs equally often in both boys and girls.
All children, regardless of the severity of MVP, presented almost the same type of complaints, the variability of which varied depending on the degree of autonomic disorders. There was pain and heaviness in the heart area, a feeling of lack of air, and frequent deep sighs. A number of children experienced paroxysmal conditions, which manifested themselves as an atypical attack of suffocation, mainly after physical exertion and psycho-emotional stress. These conditions in children with severe MVP (as a rule, these are vagotonic children) were regarded as vegetative crises. Often, such children had syncope during follow-up.
Changes in the electrocardiogram (ECG) in the form of extrasystole, long QT syndrome, WPW syndrome were noted in 24% of children with MVP, MVP in combination with other manifestations of connective tissue dysplasia (joint hypermobility, myopia, high “Gothic” palate, low position of the ears, flat feet, asthenic constitution, etc.) were observed in 12% of patients, 64% of children were diagnosed with severe autonomic disorders.
According to the echocardiographic study, depending on the severity of MVP, MVP of the 1st degree was significantly more common and was recorded in 609 children examined (86.6%), MVP of the 2nd degree was detected less often - in 81 children (11.5%), 3rd degree - in 10 people (1.5%), 4th degree - in 3 children (0.4%).
The examined patients had predominantly holosystolic and late systolic variants of prolapse (98%). In 9 patients, Doppler ultrasound examination revealed 1st degree mitral regurgitation, despite the presence of MVP greater than 7 mm.
Morphometric parameters of the heart in the examined children are presented in Table. 1. The echocardiographic examination revealed in children of all age groups, in comparison with controls, only a tendency towards an increase in the size and mass of the left ventricular myocardium. The data obtained do not contradict the literature data [1] that in children with mitral valve prolapse and metabolic disorders of the myocardium, the end-diastolic volume of the left ventricle increases by an average of 20%.
Indicators of pumping and contractile function of the myocardium in the examined children are presented in Table. 2. The analysis showed that in children with MVP in all age groups, the indicators that characterized the pumping ability (EF and %ΔD) and contractility of the left ventricular myocardium (n.Sk.ser. and Sk.ts.) also tended to decrease in comparison with control groups, which is associated with the development of metabolic disorders in the myocardium.
Indicators of the systolic amplitude of movement of the posterior wall of the left ventricle and the interventricular septum, which indirectly characterize the state of the pumping function of the left ventricle, were reduced in children with MVP in all 3 age groups compared to the controls. Changes in the kinetics of the heart muscle, which turned out to be a violation of the movement of the interventricular septum and the posterior wall of the left ventricle, were mainly recorded in the form of hypokinesia of the posterior wall of the left ventricle and the interventricular septum.
Thus, in children with MVP, there are structural prerequisites for the formation of hemodynamic disorders, which are important in the diagnosis and development of diseases of the cardiovascular system in this group of patients and are characterized so far only by a tendency to increase the end-diastolic size and mass of the left ventricle with a decrease in indicators its contractility and contractility.
Taking into account the peculiarities of the clinical manifestations of MVP, we maximally individualized the treatment and management tactics of children, taking into account age, gender, heredity, the presence and nature of dysfunction of the autonomic nervous system, as well as the degree of prolapse of the mitral valve leaflets. Depending on the severity and nature of clinical manifestations, appropriate drug therapy was prescribed. Children with dysfunction of the autonomic nervous system underwent correction of autonomic disorders.
The main aspects of the recommended therapy included the normalization of the daily routine with alternating physical and mental activity. Without exception, everyone was prescribed therapeutic exercises and a visit to the pool. The department widely used physiotherapeutic treatment methods, in particular galvanization using the reflex-segmental technique. In the last 2 years, the department has introduced the administration of drugs immediately before galvanization (thiotriazoline was administered intramuscularly 2 hours before), which ensured a direct effect of the drug on the heart muscle during metabolic changes. In complex therapy, electrophoresis of medicinal substances on the upper cervical spine was widely used: for vagotonic dysfunctions - with calcium, for sympathicotonic dysfunctions - with bromine. The darsonvalization method was used very widely and successfully.
Almost all children were prescribed herbal remedies that have a sedative effect. Children with vagotonic tendencies were prescribed herbal adaptogens: tincture of ginseng, eleutherococcus.
Drugs that improve the metabolism of the central nervous system have proven themselves well. To improve microcirculation, cinnarizine was prescribed for 2–3 weeks. If changes in the rheoencephalogram of children were recorded in the form of difficulty in venous outflow, accompanied by frequent exacerbations of respiratory neurosis, bellataminal was prescribed for 2–3 weeks.
All children were required to be prescribed courses of cardiometabolites for the prevention and treatment of metabolic changes (riboxin, ATP, etc.). Antihomotoxic drugs were also used in the complex treatment of patients with MVP.
When MVP was combined with sinus tachycardia, extrasystole, long QT syndrome, and syncope, beta-blockers were prescribed: atenolol, metoprolol or propranolol in an individually selected dose (1–2 mg/kg) for 2–4 months, followed by gradual withdrawal. Beta-blockers were also recommended for children with severe mitral regurgitation and prolapse of the mitral valve leaflets of the 3rd degree. Children with persistent rhythm disturbances without prolongation of the QT interval on the ECG were prescribed antiarrhythmic drugs (cordarone). Also, in children with MVP, brain metabolites (piracetam), vascular drugs (cinnarizine), membrane stabilizers (Aevit), and antisclerotic agents (lidase) were used for heart rhythm disturbances.
Since many clinical manifestations of MVP can progress, all of our patients with this pathology were hospitalized in the cardiology department two to three times a year. A control echocardiographic study with Doppler ultrasound 6 months after complex treatment revealed clear positive dynamics in the course of the disease in 594 (84.5%) children. Among them, in 48 (8.1%) children, MVP was no longer registered, in 71 (11.9%) children, the degree of prolapse decreased, in 59 (9.9%) patients, cardiac arrhythmias disappeared and electrocardiographic study indicators normalized, in 6 (1%) patients no longer had mitral regurgitation.
Considering the existing possibility of complications from the cardiovascular system in the form of the formation of mitral valve insufficiency, secondary bacterial endocarditis, all patients with mitral valve prolapse were subsequently under medical supervision of a local pediatrician and cardio-rheumatologist, and children with an auscultatory form of MVP accompanied by regurgitation were required to undergo Antibacterial prophylaxis was carried out during dental procedures and surgical interventions.
The results of a comprehensive examination of children with MVP showed that in the occurrence of leaflet prolapse in these children, several factors were simultaneously important, the main ones being: inferiority of the connective tissue structures of the valve, minor anomalies of the valve apparatus, dysfunction of the autonomic nervous system, contributing to hemodynamic dysregulation. Timely diagnosis of MVP and a high probability of developing possible complications make it possible to recommend effective therapy, clinical observation and adequate physical activity for this group of children.
conclusions
1. Recently, there has been an increase in the number of children with MVP, especially teenage girls.
2. In the structure of all identified MVP in children, MVP of the 1st degree was significantly more common (86.6%), and less often - of the 2nd degree (11.5%), 3rd degree (1.5%), 4 th degree (0.4%).
3. Cardiac connective tissue dysplasia syndrome, represented by mitral valve prolapse, determines the presence of structural prerequisites for the formation of hemodynamic disorders in children.
4. As a result of the complex treatment, positive dynamics were observed in 84.5% of children with MVP, among whom MVP was no longer registered in 8.1%, the degree of leaflet prolapse decreased in 11.9% of those examined, heart rhythm disturbances completely disappeared in 9, 9%, and mitral regurgitation in 1% of children.
5. The prevalence of mitral valve prolapse among children dictates the need for effective therapeutic measures and clinical observation of this group of patients in order to prevent the progression of MVP and the occurrence of complications.
Symptoms
These include the so-called stigmas - signs of imperfection of the connective tissue framework: joint hypermobility, winged shoulder blades, myopia, Gothic (high) palate, malocclusion, flat feet, tall stature and asthenic physique, scoliosis, hernias, varicose veins. There is also a violation of the architectonics of the atrioventricular ring with displacement of the valves and additional chords in the valve apparatus.
Later, by the age of 7, additional symptoms appear: short-term stabbing pains in the heart area of a psycho-emotional nature, and not due to damage to the heart muscle, attacks of rapid heartbeat, interruptions.
Symptoms of vascular dystonia include dizziness, cephalgia in the morning, worsening after overwork, decreased performance and increased fatigue. Children are tearful, often have fears, depression, irritability, and poor sleep. In fact, this is a mass of microanomalies combined with vegetative-vascular instability.
A pediatrician or cardiologist listens to the murmur over the heart area and determines its nature - late systolic or in the form of a systolic click.
Yu.M. Belozerov, Sh.M. Magomedova, I.M. Osmanov Moscow Research Institute of Pediatrics and Pediatric Surgery of the Ministry of Health and Social Development of the Russian Federation
It has been established that mitral valve prolapse (MVP) accounts for 3-5% of the population in the structure of childhood cardiovascular diseases [1]. Recent studies have shown the genetic and phenotypic heterogeneity of MVP syndrome [2, 3]. With autosomal dominant inheritance, 3 genes of the syndrome were found, which are mapped on chromosomes 16p12.1, p11.2 and 13 [4]. Another locus was found on the X chromosome (Xq28) and causes a rare form of MVP, which is designated “X-linked myxomatous valvular dystrophy” [5]. C. Yosefy, A. Ben Barak [6] identified polymorphism of the fibrillin 1 gene in exon 15 TT and exon 27 GG. This genetic heterogeneity of the syndrome causes the occurrence of various forms of primary MVP, as well as a wide range of clinical manifestations depending on age [7]. Various mutations of the listed genes lead to defective functioning of connective tissue, especially fibrillin, elastin, collagen types I and III [8]. Impaired fibrillogenesis of the extracellular matrix causes myxomatous infiltration of the mitral valve leaflets, deficiency of fibroelastic fibers, changes in collagen, and accumulation of mucopolysaccharides. Based on the “continuum of transition states,” Russian authors identify the concept of undifferentiated connective tissue dysplasia (UCTD) [9, 10], which underlies PMC. According to the Framingham Heart Study of the American College of Cardiology (ACC) and the American Heart Association, the diagnosis of MVP can only be made if two diagnostic signs are present: auscultatory and echocardiographic [11].
Material and methods All examined patients were divided into the following groups: 1st group MVP - with undifferentiated connective tissue dysplasia (UCTD) - 340 children and adolescents (this group also included primary and familial MVP with connective tissue dysplasia - DCT); Group 2 MVP - with differentiated connective tissue dysplasia (CTD) - 65 children and adolescents (this group included patients with Marfan and Ehlers-Danlos syndrome). The control group consisted of 200 children and adolescents of the same age. A scoring of the phenotypic manifestations of connective tissue dysplasia was made for group 1 - three subgroups (340 patients) were identified. A study of the elastic properties of the aortic wall was carried out in patients from both groups (64 patients). Study of the exhaustion of the autonomic nervous system - in 200 patients from all three groups, including the control.
Results and discussion According to the anamnesis, many children with MVP, both undifferentiated and differentiated CTD, were born to mothers with an unfavorable course of pregnancy and childbirth. Early and late gestosis were observed significantly more often in mothers who had children with MVP against the background of DSTD (56.9 compared to 25.8% with NSTD; pComplaints from patients with MVP with undifferentiated and differentiated DSTD were realized in a symptom complex of chronic psycho-emotional stress, the frequency of which was in 6 times higher than that of the control group of healthy children. Chronic psycho-emotional stress leads to neurocirculatory instability. Neurocirculatory instability (the term adopted by the European Association of Cardiology in 1995) is understood as a violation of the autonomous regulation of vascular tone in adolescents of the pre- and pubertal period [12 ] Unlike neurocirculatory dystonia, neurocirculatory instability is not accompanied by a persistent deviation of vascular tone - arterial hypo- and hypertension.Rises in blood pressure with neurocirculatory instability are variable, arterial hypertension can be replaced by arterial hypotension. Such changes in blood pressure can lead to somatic disorders and the formation of a specific somatotype. Significantly more often in children with DSTD compared to NSTD (52.3% and 20.2%, p In the examined children with MVP against the background of DSTD, the sensation of heartbeat can be associated with various reasons:
• disproportionate tachycardia during emotional or physical stress; • increased pulsation of the dilated aorta; • thoradiaphragmatic changes; • heart rhythm disturbances; • neuropsychiatric symptoms (panic attacks, nervousness, vegetative-vascular dystonia).
A significant increase in the frequency of cardialgia was observed in children and adolescents with MVP with undifferentiated and differentiated CTD. Pain in the heart area was characterized as “stabbing”, “pressing”, “aching” and was felt in the left half of the chest without any irradiation. In most children they lasted for 5-20 minutes, usually occurred when running, quickly climbing stairs, due to emotional stress and were usually accompanied by vegetative disorders: unstable mood, cold extremities, “chilliness”, palpitations, sweating, passed spontaneously and after taking sedatives. The absence of ischemic changes in the myocardium, according to a comprehensive examination, allows cardialgia to be regarded as a manifestation of sympathalgia associated with the psycho-emotional characteristics of children with MVP (“pain in the heart is inseparable from personality”). According to the literature, pain in the heart area in children and adolescents with MVP and CTD may be due to the following reasons:
• excessive tension of the chordae, leading to overstretching of the papillary muscles; • microembolism of the coronary arteries due to increased platelet aggregation and fibrinous deposits located in the angle between the left atrium and the posterior mitral leaflet; • disproportionate tachycardia during physical and/or emotional stress; • hyperadrenergic status, which increases myocardial oxygen demand; • spasm of the coronary arteries.
Fainting conditions were observed only with MVP against the background of DSTD and were caused by an orthostatic drop in blood pressure. Recently, the issue of disruption of neurovegetative regulation of cardiac activity and vascular tone has been discussed. Thus, many authors note orthostatic hypotension in Marfan syndrome [13], often accompanied by headaches [14]. The genesis of the resulting fainting is not fully understood. Our data confirm the presence of orthostatic instability in children and adolescents with DSTD and MVP, and fainting has a vasodepressor origin. The auscultatory picture with MVP against the background of undifferentiated and differentiated DST was almost the same. Most often, the auscultatory phenomenon of a combination of clicks with late systolic murmur was determined (53.5 and 42.9%, respectively), then late systolic or holosystolic murmur (13.3 and 30.8%, respectively, p There is a certain parallelism in the severity of leaflet prolapse and sound phenomena. With isolated clicks, the deflection of the valves is usually small, with isolated late-systolic and holosystolic murmurs it is significant. It is known that the general biological significance of growth is to achieve a level of development of the organism that is necessary for its reproduction. In humans, the final growth program is to achieve not only reproductive, but intellectual and social perfection [15].A high level of stigmata of connective tissue development was detected in children and adolescents with CTD, and we did not obtain significant differences in the subgroups with differentiated and undifferentiated dysplasia, with the exception of those disorders that are characteristic of a specific molecular genetic disease (Marfan disease - fibrillin-1 gene defect – 134797.0001, which is mapped to chromosome 15q21.1) or Ehlers-Danlos syndrome caused by mutations in the collagen alpha 1(V) gene (COL5A1; 120215), collagen alpha 2 A(V) (COL5A2; 120190) or collagen alpha 1(I) (COL1A1; 120150). On the other hand, the high frequency of stigmata of connective tissue dysembryogenesis in DST confirms the fact that, along with the genetic mechanisms of the disease, external factors are of great importance, which can cause significant individual deviations, clinical polymorphism of DST. The scoring of the phenotypic manifestations of connective tissue dysplasia in NSTD indicates a wide range of the studied parameters in this group of patients with MVP. In this regard, based on multifactor analysis, including anamnestic and genealogical data, as well as examination results, we identified three subgroups of children and adolescents with MVP against the background of NSTD:
1st – MVP with moderate manifestations of NSTD (score from 23 to 49 – 82 patients); 2nd – MVP with pronounced manifestations of NSTD (score from 50 to 75 – 196 patients); 3rd – MVP with pronounced manifestations of NSTD (score from 76 to 90 – 62 patients).
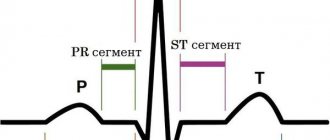
On physical examination, the boundaries of the heart in all examined patients corresponded to normal values, with the exception of children with chest deformities, when there was a shift (usually to the left) of the percussion boundaries of the absolute and relative dullness of the cardiac shadow. Quite often, in children with MVP against the background of NSTD, dilatation of the pulmonary artery was detected. It should be noted that X-ray examination allows to detect dilatation of the pulmonary artery (PA) and confirm its severity with a Moore index of more than 40%, but does not reveal the true cause of PA dilatation. We compared the Moore index with the level of stigmata of disembryogenesis. The Moore index was higher, the more phenotypic signs of connective tissue dysembryogenesis were determined. This confirms the connection between pulmonary artery dilatation and the inferiority of the connective tissue matrix. The main electrocardiographic abnormalities found in NSTD and DSTD occur in 30% of cases and include changes in the terminal part of the ventricular complex, cardiac rhythm and conduction disturbances, and prolongation of the QT interval. Repolarization anomalies are detected both during a standard ECG and much more often during 24-hour electrocardiogram monitoring [16]. This fact indicates the presence of hidden myocardial instability in children with MVP syndrome against the background of both differentiated and undifferentiated DST. The appearance of repolarization changes in orthoposition can be explained by an increase in the tension of the papillary muscles due to the resulting tachycardia, a decrease in the volume of the left ventricle and an increase in the depth of leaflet prolapse. If previously the cause of such ST-T changes on the ECG during MVP was associated with ischemic impairment of the coronary circulation or was considered as a combined manifestation of a dysplastic process in the heart, now most authors see the cause of repolarization disorders during MVP as hypersympathicotonia. This statement is justified by the fact that ST-T changes in MVP are variable in nature and completely disappear during a pharmacological stress test with a b-blocker. A few publications report the occurrence of myocardial ischemia in MVP syndrome in children [17]. The genesis of transient ischemia in such patients may be due to congenital anomalies of the coronary vessels. We identified myocardial ischemia during physical activity, if the process of repolarization of ischemic genesis deteriorated, and was detected in a few patients (2 patients with MVP and NSTD and 3 patients with DSTD). We conducted a study of minor anomalies in the development of cardiac structures in children with MVP and CTD. Most of the microanomalies are related to the connective tissue structures of the heart. Some minor anomalies, such as impaired distribution of the chordae, may be directly related to the MVP syndrome, being a causative factor. Other anomalies, such as dilatation of the great vessels, coronary sinus, etc., reflect the inferiority of connective tissue structures. Of particular importance are abnormally attached tendon chords of the subvalvular apparatus. A number of authors consider them to be the cause of mitral valve prolapse [18]. With connective tissue dysplasia, not only the valve apparatus of the heart is affected, but also the great vessels. In this regard, we undertook a study of the elastic properties of the aortic wall in adolescents with MVP using the method of E. Michelfelder et al. [19]. The distensibility index and stiffness of the aorta were determined. The study was conducted in 64 adolescents aged 15-18 years (average age 16.4±0.7), divided into 2 subgroups: 1st subgroup - 48 patients (33 girls and 15 boys) with MVP due to NSTD; 2nd subgroup – 16 (10 girls, 6 boys) patients with MVP and DSTD. A significant increase in the aortic distensibility index was established (aortic distensibility: control 0.0021±0.005 mmHg-1, MVP and NSTD - 0.0035±0.007 mmHg-1, MVP and DSTD - 0.0038±0.006 mmHg-1 (pCharacteristic vegetative changes were established with MVP against the background of NSTD. With an increase in the degree of DST, there was a significant increase in vagotonic signs, which may be associated with a compensatory reaction to the initial sympathicotonia. The study of the state of the autonomic nervous system made it possible to establish a characteristic autonomic pattern in DSTD, when the initial sympathicotonia is combined with asympathicotonic reactivity. This this fact indicates a low adaptive ability and rapid "exhaustion" of the sympathetic part of the ANS. Many children with MVP, mainly in adolescence, exhibit psycho-emotional disorders, represented by depressive and asthenic symptom complexes. In order to assess the psychological portrait of the individual, we used the abbreviated multifactor personality questionnaire - SMOL . When determining the psychological profile (200 adolescents were examined) of an individual by testing the SMOL, we obtained a number of patterns. Indicators of the average profile of SMOL in adolescents of the control group did not go beyond the conventionally accepted norm: >70 and Maximum characterological changes were found in adolescents with MVP against the background of NSTD. Noteworthy were the high values on the second and seventh scales, exceeding 70 points, which reflected pronounced psychological maladaptation, as well as profile peaks on the third scale, emphasizing exalted behavior and emotional lability. In addition, intergroup differences were obtained for the indicators of this scale between the groups with NSTD and DSTD. Noteworthy is also the peak of the profile on the first scale (67.5 points), approaching the conventional border of mental norm/pathology - 70 points. This indicates a significantly pronounced tendency towards aggravation, “going into illness” among adolescents in this group, which is combined with pronounced emotional lability. In the group of adolescents with MVP and DSTD, significant increases in the profile were found on the second, third and seventh scales relative to the comparison group, which reflected a gloomy mood background, increased anxiety combined with a tendency to hysterical reactions. A decrease in the quality of life in adolescents with various types of MVP has been revealed, affecting both mental and physical health. The degree of reduction in quality of life and the number of scales affected depends on the severity of connective tissue dysplasia. Adolescents with both MVP and DSTD and MVP and NSTD were characterized by a decrease in the quality of life on almost all scales studied. In scales characterizing physical functioning, the lowest scores were observed in the group of people with MVP and DSTD. As for the mental component of health, the lowest values were observed in the group of adolescents with MVP and NSTD, although in patients with MVP and DSTD they were also significantly lower than control values. Thus, we can conclude that the degree of connective tissue disorders is the leading factor determining the quality of life of a teenager. The management tactics for children with MVP vary depending on the degree of connective tissue dysplasia, the severity of leaflet prolapse, and the nature of autonomic and cardiovascular changes [20]. We noted a positive result in the treatment of children with MVP and DST with carnitene and magnesium preparations. In children and adolescents with MVP and CTD, in most cases, there is a deficiency of carnitine, which is confirmed by chronic fatigue syndrome. A test with carnitene is an indicator of the insufficiency of trophotropic mechanisms in the regulation of cardiac activity. A positive response to carnitene is indicated by changes in HRV in the form of an increase in VLF and a decrease in HF. All children with mitral valve prolapse are prescribed carnitene to improve energy processes in the heart muscle. There is no doubt that energy-tropic therapy with carnitene (based on the examination of 30 children) is an important element in the correction of metabolic disorders in the heart muscle in patients with MVP and CTD. On the other hand, the positive effect of the therapy confirms the large role of secondary mitochondrial failure in the pathogenesis of connective tissue dysplasia. We also conducted a study of the effect of the drug Magnerot® on the structure of the mitral valve leaflets in MVP associated with NSTD. In the initial values for MVP, a significantly greater thickness of the leaflets in boys was revealed (t = 5.11 p After a 6-month course of therapy with Magnerot® in patients with MVP and NSTD, a significant improvement in objective and subjective symptoms was found with a complete or almost complete reduction in the manifestations of the disease by more than in half of the patients. During treatment, there was a decrease in the severity of vegetative dystonia syndrome, vascular, hemorrhagic and psychopathological disorders, heart rhythm disturbances, blood pressure levels, as well as an improvement in the quality of life of patients. In addition, during treatment, the severity of morphological markers of connective tissue dysplasia significantly decreased [ 10]. Thus, the data obtained indirectly indicate that in the basis of dysplastic development of connective tissue structures, not only genetic factors play a great role, but also pathological “maturation”, differentiation of connective tissue with impaired fetal development. It should be noted that the development and the maturation of the mitral apparatus, connective tissue structures and the autonomic nervous system occurs synchronously at the same time of embryogenesis and postnatal ontogenesis.
References 1. Sakamoto S. Mitral valve prolapse. Nippon Rinsho. July 2005; 63 (7):1195-2000. 2. Yosefy C, Levine RA, Picard MH et al. Pseudodyskinesis of the inferior left ventricular wall: recognizing an echocardiographic mimic of myocardial infarction. J Am Soc Echocardiogr. 2007 Dec; 20 (12): 1374-9. 3. Martínez-Sellés M., García-Fernández M.A., Larios E. et al. Etiology and short-term prognosis of severe mitral regurgitation. Int J Cardiovascular Imaging. Feb 2009; 25 (2): 121-6. 4. Levine RA, Slaugenhaupt SA Molecular genetics of mitral valve prolapse. Curr Opin Cardiol. May 2007; 22 (3): 171-5. 5. Grau JB, Pirelli L., Yu PJ, Galloway AC, Ostrer H. The genetics of mitral valve prolapse. Clin Genet. 2007 Oct; 72 (4): 288-95. 6. Yosefy C., Ben Barak A. Floppy mitral valve/mitral valve prolapse and genetics. J Heart Valve Dis. 2007 Nov; 16 (6): 590-5. 7. Romanelli P., Romanelli R., Rongioletti F. et al. Clinical significance of cutaneous proteoglycan (mucin) infiltration in patients with mitral valve prolapse. J Am Acad Dermatol. July 2008; 59 (1): 168-9. 8. Gupta-Malhotra M., Dave A., Sturhan BC et al. Prevalence of undiagnosed congenital cardiac defects in older children. Cardiol Young. 2008 Aug; 18 (4): 392-6. 9. Martynov A.I., Stepura O.B., Ostroumova O.D. etc. Mitral valve prolapse. Part I. Phenotypic features and clinical manifestations. Cardiology. 1998; 1: 72-80. 10. Melnik O.O., Ostroumova O.D., Stepura O.B. Mitral valve prolapse - normal or pathological? 2002; 10:28:1314-28. 11. Freed LA, Levy D, Levine RA et al. Prevalence and clinical outcome of mitral valve prolapse. N.Engl. J. Med. 1999, 341(1): 1-7. 12. Mochizuki Y., Okutani M., Donfeng Y. et al. Limited reproducibility of circadian variation in blood pressure dippers and nondippers. Am J Hypertens. 1998 Apr; 11 (4 Pt 1): 403-9. 13. van Dijk N., Boer MC, Mulder BJ, van Montfrans GA, Wieling W. Is fatigue in Marfan syndrome related to orthostatic intolerance? Clin Auton Res. 2008 Aug; 18 (4): 187-93. 14. Rosser T., Finkel J., Vezina G., Majd M. Postural headache in a child with Marfan syndrome: case report and review of the literature. J Child Neurol. 2005 Feb; 20 (2): 153-5. 15. Veltishchev Yu.E. Child growth: patterns, normal variations, somatotypes, disorders and their correction. 2000; 66. 16. Digeos-Hasnier S., Copie X., Paziaud O., Abergel E., Guize L. et al. Abnormalities of ventricular repolarization in mitral valve prolapse. Ann Noninvasive Electrocardiol. July 2005; 10 (3): 297-304. 17. Guthmann JP, Rossignol AM, Wolf JE, Azoulay A., Bost M. Transient myocardial ischemia and isolated congenital mitral valve prolapse in an infant. Arch Mal Coeur Vaiss. May 1991; 84 (5): 735-8. 18. Boon R., Hazekamp M., Hoohenkerk G., Rijlaarsdam M., Schoof P. et al. Artificial chordae for pediatric mitral and tricuspid valve repair. Eur J Cardiothorac Surg. July 2007; 32 (1): 143-8. 19. Michelfelder EC, Khoury P., Witt SA, Glascock BJ, Kimball TR Noncircumferential myofiber function: impact on early diastolic filling in children. J Am Soc Echocardiogr. 2001 Nov; 14 (11): 1065-9. 20. Scordo KA Medication use and symptoms in individuals with mitral valve prolapse syndrome. Clin Nurs Res. Feb 2007; 16 (1): 58-71.
Symptoms of the disease in the younger age group
Diagnosis of MVP in children under 3 years of age is carried out mainly under the supervision of a family doctor. The appearance of complaints is most often associated with high physical or psycho-emotional activity.
Physical activity for children in the first year of life is considered to be breastfeeding or crying. Signs of disorders in the cardiovascular system: shortness of breath, redness or cyanosis (cyanosis) of the skin, flaring of the nose or noisy inhalation.
The most common complaint with mitral valve prolapse in a teenager is nonspecific (“stabbing”, “pressing” or “aching”) pain in the left half of the chest. They are characterized by the absence of irradiation and last from 5 to 20 minutes.
Most often, pain occurs when running or quickly climbing stairs and is accompanied by unstable mood, sweating, and cold extremities. Doctors associate the appearance of this symptom with increased activity of the sympathetic division of the autonomic nervous system (increased release of catecholamine contributes to vasospasm and increased myocardial oxygen demand).
The main symptoms that occur in children with MVP:
neurocirculatory instability, which is manifested by changes in blood pressure (alternating rise and fall);- disproportionate tachycardia (rapid heartbeat) during physical exertion or severe emotional shock;
- increased and accelerated pulsation of blood vessels;
- rhythm disturbances (secondary changes that occur with significant remodeling of the heart or involvement of the conduction system in the process);
- neuropsychic symptoms (panic attacks, nervousness, vegetative-vascular dystonia).
The diagnosis of MVP is made only after confirmation of the anomaly using auscultation (a characteristic systolic murmur is heard at the apex of the heart) and echocardiography.
Signs of pathology during ultrasound examination are changes in thickness and eversion of the valves during systole into the atrium cavity, as well as the level of regurgitation. Depending on the severity of the reverse blood flow, the degree of prolapse is determined, which determines the prognosis and further tactics of patient management.