Heart valves and their defects
The heart has four chambers: two atria and two ventricles.
From the atria, blood enters the ventricles, and then through the valves, with the help of contractions of the heart muscle, enters the arteries. The valves ensure blood flow in the desired direction and quantity. If they close or do not open completely, this prevents normal blood circulation. As a result, the heart gradually increases in volume and stretches, compensating for blood deficiency and working under constant overload. Exhaustive work of the heart can cause the development of serious cardiovascular diseases, such as arrhythmia or heart failure. In addition, heart valve defects can cause complications due to certain ongoing infectious diseases.
Most often, heart defects are diagnosed in patients over sixty years of age. The reason is that with age, the valves of the valve apparatus lose their elasticity, and the heart increases in size. As a result, blood flow decreases and it unevenly fills the cavities of the heart - heart failure develops.
There are four types of heart valves, and each has a specific function:
- Aortic : prevents blood from flowing from the aorta into the left ventricle of the heart.
- Mitral : prevents the flow of blood from the left ventricle of the heart into the left atrium at the moment when the heart muscle contracts and blood is pushed into the vessels.
- Pulmonary : Prevents the flow of blood from the pulmonary artery into the right ventricle of the heart.
- Tricuspid : valve between the right ventricle of the heart and the right atrium.
If the valves are enlarged, narrowed, loose or torn, it becomes difficult for them to close, and blood flows back with each contraction of the heart. As a result, the heart experiences enormous stress and eventually loses its performance.
Depending on the form of the disease, heart valve defects can manifest as:
- stenosis – narrowing of the lumen (opening) of the vessels through which blood flows. This significantly increases the load on the heart, as it makes it more difficult for blood to be pumped out.
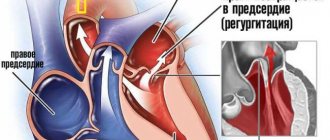
- insufficiency - damage to the heart valve leaflets, resulting in their inability to close completely. In such cases, the blood flows back.
- a combination of stenosis and insufficiency - the affected valves form an obstacle to the passage of blood. In this case, some of the blood passes through the hole, but returns back into the next phase of the cardiac cycle.
Indications for surgery
The main indication for replacing a valve in the heart is its severe organic damage with the formation of heart disease,
having a significant effect on hemodynamics. Valve defects can develop as a result of rheumatic fever (rheumatism) - a form of streptococcal infection characterized by damage to the joints and heart (usually occurs as a result of frequent tonsillitis, chronic tonsillitis).
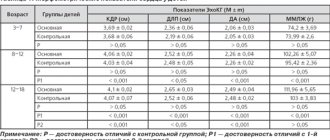
The need for valve replacement is taken into account based on the stage of heart failure, as well as according to data obtained from ultrasound of the heart (echocardioscopy).
valvular structure of the heart and an example of mitral valve stenosis requiring replacement
So, clinical indications for surgery:
- Fainting, chest pain, shortness of breath in patients with aortic valve stenosis,
- Clinical manifestations of aortic stenosis in patients who have undergone coronary artery bypass grafting,
- Severe stages of chronic heart failure - severe shortness of breath at the slightest household activity and/or at rest, significant swelling of the limbs, face, whole body (anasarca) in patients with moderate or severe mitral valve stenosis,
- Initial signs of heart failure (shortness of breath during significant physical exertion, heart rhythm disturbances) in patients with mild mitral valve stenosis,
endocarditis is one of the causes of valve damage
Infectious, or bacterial endocarditis - vegetation of bacterial inflammation on the inner lining of the heart, including the valves.
Echocardioscopy data:
- Severe (critical) aortic stenosis, even in the absence of clinical manifestations - the area of the aortic valve opening is less than 1 cm2,
- Reduced ejection fraction (the volume of blood thrown into the aorta with each contraction of the left ventricle) less than 50%,
- The area of the mitral annulus is less than 1.5 cm2,
- Ejection fraction with mitral stenosis is less than 60%.
Causes and symptoms
Heart valve defects can be congenital or acquired. The main causes of the development of heart valve defects are rheumatism, infections, myocardial and cardiovascular diseases.
Congenital heart valve defects develop before birth and depend on how the pregnancy progressed. Congenital heart valve defects are an extremely rare diagnosis, diagnosed only in 1% of cases. Congenital defects include defects of the aortic and pulmonary valves, which are treated by surgical intervention in the first years of the patient’s life.
Purchased . Acquired heart valve defects include transformations of the valve structure due to infections, inflammation, previous heart attacks, etc. Most of them arise as a result of a gradual change in the structure of the heart; in some cases, rheumatism leads to the defect. All congenital and acquired defects have related symptoms that can appear at any age:
- increased heart rate,
- dyspnea,
- swelling,
- other manifestations of heart failure.
Initially, they appear during physical activity, but as pathologies develop, they will begin to appear in a calm state. Among the types of heart valve defects, mitral valve prolapse is the most common. It occurs during heart contractions when the valve leaflets in the left atrium sag. The walls of the valve lose elasticity and it “leaks”. Prolapse can be primary or secondary:
- Primary prolapse refers to congenital valve defects. Connective tissue pathologies in this case are a genetic predisposition.
- Secondary prolapse is an acquired defect. It occurs due to chest injury, rheumatism or myocardial infarction.
Prolapse does not have serious health consequences, and its symptoms do not interfere with life. However, they may not appear for a long time and most often bother people in old age, which is why they are written off as “age-related.” If you do not pay attention to the symptoms in time, complications may arise, such as arrhythmia and heart failure.
Symptoms also include complaints of pain in the heart area. They arise against the background of anxiety, are not associated with physical activity and are not relieved with medication. The pain is not intense, but long-lasting, accompanied by anxiety and rapid heartbeat.
Prosthetic heart valves – what are they?
Since the 1970s, the configuration of prosthetic valves has undergone some changes. Valves based on ball prostheses are considered one of the most outdated.
Later, valves based on hinged disc prostheses began to be used.
The most modern valves are those based on bicuspid hinged prostheses, which are currently used.
In addition, in patients with an increased risk of thrombosis, models obtained from the pig heart are used - biological prostheses, or xenografts.
The disadvantage of mechanical prostheses is the high rate of formation of blood clots on the valve leaflets
, which is associated with a high risk of pulmonary embolism, ischemic stroke, thrombosis of the femoral arteries with possible amputation of a limb, etc. In this regard,
in elderly people (over 65 years old), it is preferable to undergo valve replacement surgery with a biological prosthesis.
It is also possible to have an operation with prosthetic replacement of the aortic valve with the patient’s own pulmonary valve with simultaneous replacement of the latter with a biological prosthesis.
The disadvantage of biological prostheses is the high risk of re-development of bacterial inflammation on the installed porcine valve.
The service life of the valves in the absence of complications is from 10 to 15 years; if the valve wears out, it is possible to perform a second operation to replace it.
Diagnosis and treatment
If you or your loved ones are experiencing the symptoms described above, we recommend getting tested. During diagnosis, the doctor monitors heart parameters at rest and during exercise.
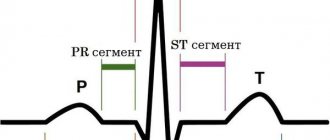
The patient is prescribed:
- daily ECG monitoring,
- echocardiography (ECHO-CG),
- chest x-ray,
- CT and MRI using special equipment that allows you to examine the heart virtually between beats.
Such diagnostics are carried out not only during the initial examination of patients with suspected disease, but also in dispensary groups of patients with an already confirmed diagnosis.
Depending on the diagnostic results, the doctor prescribes the necessary treatment: therapy or surgery.
- Therapy is aimed at preventing, preventing and alleviating relapses of the disease that became the root cause of the defect, as well as treating heart failure.
- Surgical intervention is an extreme necessity, which due to age or complications may not be prescribed for all patients.
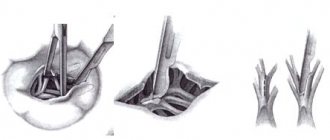
Typically, heart valve disease is a mechanical problem that can only be solved with surgery performed by a surgeon. For stenosis, an operation is indicated to separate the fused valve leaflets and widen the atrioventricular opening - commissurotomy. If there is insufficiency, prosthetics are performed: replacement with a biological or mechanical analogue.
Contraindications for surgery
Heart valve replacement surgery is contraindicated for the following diseases and conditions:
- Acute myocardial infarction,
- Acute cerebrovascular accidents (stroke),
- Acute infectious diseases, fever,
- Exacerbations and worsening of chronic diseases (diabetes mellitus, bronchial asthma),
- Extremely severe heart failure with an ejection fraction of less than 20% with mitral stenosis, in which case the attending physician should decide whether a heart transplant is necessary.
How is the operation performed?
Preoperative preparation is limited to the prescription of sedatives and hypnotics. The operation is performed under general anesthesia on the same or the next day after hospitalization using a heart-lung machine, which performs the functions of pumping blood throughout the body during manipulations.
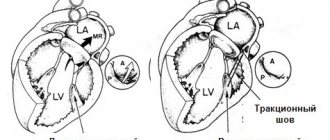
After putting the patient into deep sleep, a median sternotomy is performed - a longitudinal incision of the skin and sternum. Next, an incision is made in the left atrium for mitral valve replacement and in the aortic wall for aortic valve replacement. After this, the prosthesis ring is fixed with continuous sutures and the dissected part of the heart is sutured.
After installing the prosthesis, electrodes for temporary cardiac stimulation must be applied, and the surgical wound is sutured. Wire sutures are used to fuse the edges of the sternum.
In the early postoperative period, the patient is in the intensive care unit with artificial ventilation, the cessation of which is possible only when the patient is completely stabilized and spontaneous breathing is restored.
The operation time is from three to six hours, and the hospital stay is determined by the general condition of the patient and ranges from two to four weeks.
In addition to open heart operations, it is currently possible to perform minimally invasive operations, in particular, with a mini-access from an intercostal incision on the right or left without dissecting the sternum, as well as with endovascular intervention.
minimally invasive aortic valve replacement
The latter is used only for aortic valve replacement and is carried out by introducing a biological prosthesis through the femoral vein into the right and then into the left atrium with further location in the aorta.
Endovascular heart valve replacement is primarily preferred for individuals for whom open heart surgery is contraindicated.
Video: report on valve replacement surgery
Postoperative period and discharge
Upon admission to the intensive care unit, the condition is severe and corresponds to the volume of surgical intervention.
In the postoperative period, sinus rhythm was restored, followed by a breakdown into atrial fibrillation. An attempt at recovery with a short-term effect. It is recommended to perform electrical pulse therapy three months after surgery.
On the fourth day after surgery, the patient was transferred from intensive care to the department in satisfactory condition.
Cost of the operation
In most cases, surgery to replace heart valves is performed free of charge, thanks to quotas from the Russian healthcare system under the compulsory medical insurance system. However, if for some reason it is not possible to obtain a quota, there is always the option of carrying out the operation at your own expense.
The cost of the operation itself, the prosthesis and rehabilitation in the early postoperative period ranges from 90 to 300 thousand rubles
, and the price is higher, the more complex the operation is, for example, the simultaneous replacement of the aortic valve and pulmonary valve is higher than one of them.
Heart valve replacement surgeries are carried out in all major cities of Russia, and now such interventions are not rare or inaccessible to the population.
Acquired vices
The causes of acquired defects are severe chronic diseases, so they often develop in adulthood. The greatest connection has been established with:
- rheumatism;
- septic conditions (endocarditis);
- previous pneumonia;
- syphilis;
- atherosclerosis.
The nature of pathological changes is different:
- With rheumatic lesions, the valves are soldered at the base and wrinkled.
- Endocarditis deforms the valves, starting from the free edge. Here, warty growths are formed due to the proliferation of colonies of streptococci, staphylococci, and chlamydia. Fibrin is deposited on them and the leaflets fuse together, losing the ability to completely close.
- With atherosclerosis, the lesion passes from the aortic wall, the valves thicken, fibrosis develops, and calcium salts are deposited.
- Syphilitic changes also spread to the valves of the aorta, but are accompanied by the death of elastic fibers and expansion of the fibrous ring. The valves become dense and inactive.
The causes of the inflammatory process can be autoimmune diseases (lupus erythematosus), chest injuries.
In older people, atherosclerosis of the aortic arch leads to expansion of the root, stretching and sclerosis of the valves.
Lifestyle
A person’s further life after surgery comes down to the following points:
- Regular visits to the doctor - monthly in the first year after surgery, every six months in the second year and annually thereafter, with constant monitoring of the functions of the cardiovascular system using ECG and echocardioscopy,
- Regularly taking prescribed medications (anticoagulants, antibiotics),
- Treatment of residual heart failure with the constant use of digoxin and diuretics (indapamide, veroshpiron, diuver, etc.),
- Adequate physical activity
- Compliance with the work and rest schedule,
- Following a diet - excluding fatty, fried, salty foods, eating large amounts of vegetables, fruits, dairy and cereal products,
- Complete elimination of bad habits.
Question of military service
Some young guys plan to enter naval schools or go to military service after reaching adulthood. Others want a reprieve. Therefore, a natural question would be whether an army with such a diagnosis as bicuspid aortic valve is possible. If, due to a valve defect, reverse blood flow is observed, that is, it flows in the opposite direction from the norm, then conscripts must be released from service. They are given a deferment and recognized as having limited fitness. This corresponds to category B.
But in the absence of signs of reverse flow and other complications, the congenital defect itself is not considered an argument for preventing conscription.
Complications
The most serious complications after the introduction of a prosthesis are thromboembolic ones. Prevention of their development is lifelong antithrombotic therapy with the help of anticoagulants and antiplatelet agents - drugs that “thin” the blood. Such drugs include:
- Subcutaneous injections of heparin in the early postoperative period,
- Continuous use of warfarin under monthly monitoring of INR (international associated ratio) - an important indicator of the blood clot-forming system; normally it should be within 2.5 - 3.5,
- Constant use of aspirin (thromboAss, acecardol, aspirin Cardio, etc.).
No less dangerous consequences are the development or recurrence of infective endocarditis, the prevention of which is the rational prescription of antibiotics in the postoperative period, as well as their further use during any operations and minimally invasive interventions (tooth extraction, gynecological and urological manipulations, etc.).
Structure
The mitral valve (MV) consists of a fibrous opening and leaflets that are attached around its circumference. The structure of the MV includes chordae tendineae, papillary papillary muscle fibers adjacent to the cardiac myocardium of the left ventricle, and its own fibromuscular ring. Each element ensures the normal functioning of the microcontroller.
Anatomy of the left atrioventricular orifice:
- The MV is divided into two valves by commissural septa, of which the anterior one is rounder and longer, the posterior one is short and somewhat reminiscent of a square;
- in some cases there may be from 3 to 5 valves;
- the number of additional elements depends on the size of the fibrous ring (AF);
- in the places where the valves close, papillary muscle fibers are attached (normally, a person has up to 3 anterior and 1-5 posterior muscles);
- tendon fibers (chordae) are attached to the fibrous surface of the MV, directed into the cavity of the left ventricle, which are further divided into threads for each leaflet;
- the movement of structures depending on the phase of contractility is smooth and precise;
- all elements ensure full opening of the bicuspid mitral valve of the heart in the antiphase diastole phase - multidirectional physiological movement of the valves, facilitating the outflow of blood.
Histological structure of the mitral valve
The main tissue components of MC:
- valves formed by three-layer connective tissue, attached to the atrioventricular opening;
- own valve ring made of fibrous and muscle tissue;
- the inner surface is lined with the lining of the heart, the endocardium;
- the middle section is made of spongy tissue.
What the mitral valve of the left chambers of the heart looks like and what it is is shown in the photo below: