Testicular varicose veins, or varicoceles, are a problem that many men face. Often the disease occurs in adolescence and is detected during a urological examination. According to statistics, 5-7% of young people aged 18-20 years and 15-17% of men under 40 suffer from varicocele. In 80-98% of cases, left-sided varicose veins are observed.
Varicocele is characterized by a hidden course and does not manifest itself for a long time. It is possible to detect the disease in its early stages only with the help of special tests. The Valsalva maneuver for varicocele helps to visualize pathologically dilated veins. What is this research and what are its benefits?
Historical reference
Today, the Valsalva maneuver for varicocele is used to assess the increase in the venous network of the spermatic cord when holding the breath and straining. A similar technique with minor modifications was used more than 100 years ago, but for a different purpose.
Back in the 20th century, a method named after the surgeon Antonio Maria Valsalva was actively practiced. An Italian specialist studied the anatomy of the ear and concluded that the main function of the auditory tube is to ventilate the middle ear to maintain optimal pressure on both sides of the eardrum. In normal condition the pipe is closed. When diving under water, the pressure increases greatly. To normalize it, you need to exhale.
Initially, a technique based on this discovery was practiced to cleanse the middle ear and diagnose brain and heart diseases. Later, the scope of application became wider: a modified Valsalva maneuver began to be actively used in urology for the diagnosis of varicocele.
Algorithm and need for ultrasound scanning
While physical methods can only detect the presence of varicocele in the spermatic cord, ultrasound scanning informs about the type of disease and disturbances in spermatogenesis that the disease has caused, and provides an information base for prescribing adequate treatment tactics. To confirm the effectiveness of ultrasound scanning, it is advisable to familiarize yourself with the results of one of the studies. The work was carried out in the period 1998-2006 in the department of vascular surgery of the State Clinical Clinical Hospital. Men with varicocele (101 patients) aged 6 to 35 years were examined and operated on.
To assess the morphological state of the renocaval zone and the vessels of the pampiniform plexus, complex phlebography, echography and phlebottensiometry were used. Diagnostics made it possible to identify 3 types of hemodynamically significant reflux into the veins of the pampiniform plexus according to Coolsaet, with the first renospermatic type without reflux found in 89 patients, the second ileospermatic type was diagnosed in 7 men, and the third mixed type was observed in 5 patients.
During the ultrasound examination of the renocaval zone, close attention was paid to the signs of aorto-mesenteric compression of the left renal vein. Based on the examination, it was possible to formulate indications for reconstructive intervention on the left testicular vein.
Along with the Valsalva maneuver and ultrasound diagnostic methods, one of the mandatory procedures that the patient undergoes at the diagnostic stage is spermogram analysis. Such a study is aimed at determining the volume of ejaculate, the percentage of sedentary, immobile and dead sperm, the speed of their movement and other parameters affecting reproductive function.
Method of performing the Valsalva maneuver
The Valsalva maneuver is widely used in the diagnosis of varicocele in the early stages, when there are no pronounced clinical symptoms yet. The technique is used as an independent method of examination or in combination with ultrasound.
In patients with suspected varicocele, the Valsalva maneuver is performed at the first examination. The man takes a deep breath and holds his breath. At this time, the urologist palpates the scrotum and testicles. In the presence of pathological changes, even slight dilation of the veins becomes noticeable.
To assess blood flow in the affected vessels, the Valsalva maneuver is also performed during ultrasound. The specialist asks the man to take a deep breath and strongly tense his abdominal muscles. Signs of the disease are expansion of the spermatic cords and the appearance of elastic nodules.
Our clinic invites you to undergo diagnostics and surgical treatment of varicocele. The medical facility is equipped with the necessary equipment, and consultations are conducted by experienced urologists-andrologists. Sign up for consultations by phone.
Antonio Maria Valsalva was a distinguished anatomist, physiologist and professor of surgery at the University of Bologna. In 1704, he published his most famous work, De Aure Humana Tractatus, which served as a reference for the treatment of middle ear diseases for more than a century. In several paragraphs of his book, A. M. Valsalva described in detail a therapeutic technique “for pushing foreign bodies and fluids out of the middle ear,” in which the patient attempted to exhale for several seconds with his mouth and nose closed. Many years later (1851) in Germany, the physiologist Edward Weber detailed the changes in the cardiovascular system associated with this technique, allowing it to be used to determine the autonomic (autonomic) regulation of the heart. Historically, giving due credit to both authors, in world literature sources this technique is often called the Valsalva-Weber maneuver (VW) [1].
The test makes it possible to quantitatively and comprehensively assess the contribution of the sympathetic and parasympathetic parts of the autonomic nervous system (ANS) to the regulation of the functions of the heart and blood vessels [2].
The role of autonomic disorders in the origin of vasovagal syncope (VVO) is widely discussed. The possibilities of using PVV in patients with VZV have not been studied, which determined the relevance of this study.
Materials and methods
The study included 12 healthy individuals (all men, mean age 31±7 years) and 30 patients with VZV (12 (40%) men, mean age 32±14 years). The patients had significantly lower height and body weight compared to the group of healthy individuals, probably due to the predominance of men in the latter group. The vasovagal genesis of fainting in patients in all cases was confirmed by clinical survey data using a specially developed questionnaire [3]. At the same time, other (metabolic, neurological, cardiac and orthostatic) causes of attacks of loss of consciousness are excluded by the results of a preliminary instrumental examination.
The patients also did not have clinically significant diseases of a somatic, endocrine, neuropsychic nature or were taking medications.
All individuals included in the study underwent PVV. The test was carried out using a specialized complex Task Force Monitor (“CNSystem”, Austria), which made it possible to synchronously monitor the electrocardiogram (ECG) and heart rate (HR) - RR
non-invasively, in a “beat-to-beat” mode, monitor blood pressure (BP) on the fingers of the right hand using the photocompensation method (based on changes in pulse blood supply) in combination with periodic calibration of the signal taking into account blood pressure measured by the oscillometric method on the left shoulder.
Initially, the patient was at rest, lying on his back, for 20 minutes, the initial parameters were recorded.
At this time, the test procedure was explained to the subject and the Valsalva maneuver was taught, including a short trial of performing it. Then PVV was performed in accordance with the recommendations of P. Novak [2].
When performing the test, the subject took a mouthpiece into his mouth (a disposable plastic syringe with a capacity of 10 ml, to the connector for the needle of which the inlet hose of the pressure gauge was connected; at a distance of 10 mm from this place, 4 holes were made in the body of the syringe with a needle No. 0740 to ensure a small leak of air during forced exhalation , which prevented “incorrect” performance of the test by a patient with a closed glottis). The patient took a deep breath and then exhaled forcefully into the mouthpiece. Based on the readings of a pressure gauge connected to the mouthpiece, he maintained a pressure of 40 mm Hg. within 15 s. Then the subject released the mouthpiece and took a normal breath. To facilitate the test, a special nose clip was used.
The test was repeated three times with a 3-minute interval between tests. For subsequent calculations, one of the tests with the minimum number of artifacts in blood pressure and heart rate trends was selected. For in-depth processing of the study results and calculation of additional indicators, data from trends in blood pressure and heart rate were exported into Excel spreadsheets, followed by calculation using the capabilities of the Excel program.
Analysis of the results of PPV to identify ANS disorders and determine the degree of their severity included a visual assessment of the curves of changes in blood pressure and heart rate, as well as the calculation of parameters that are currently used by leading laboratories involved in the diagnosis and treatment of ANS pathology [2, 4-6]. A complete list of such indicators is given in table. 1
, and a schematic representation of the sample phases is in
Fig.
1 .
Figure 1. Dynamics of mean blood pressure and RR
during PPV in a healthy volunteer. Explanations in the text.
Statistical processing and analysis of the obtained data was carried out using nonparametric methods. To assess intergroup comparisons of indicators, the Mann-Whitney test was used, and to study the reliability of changes in indicators in each of the study groups during the tests, the Wilcoxon method was used. To estimate the frequencies of qualitative characteristics, Fisher's nonparametric method was used. All differences were considered significant at p
<0,05.
Results and discussion
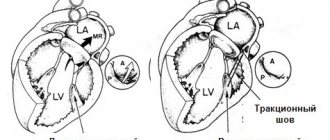
When analyzing changes in indicators of the cardiovascular system function during PVV, 4 phases are distinguished (see Fig. 1; Fig. 2)
[1, 2, 4-7].
Figure 2. Dynamics of mean blood pressure and RR
during PPV in a patient with VZV.
MAP in late phase II does not reach the initial level (for the normal version of the reaction for comparison, see Fig. 1). In phase I, when the subject takes an intense breath and begins expiratory effort, an increase in blood pressure is observed due to the increased ejection of blood from the heart, while a slight decrease in heart rate may be observed (an increase in the duration of the R-R
).
Phase II corresponds in time to expiratory tension and is characterized by a rapid initial decrease in blood pressure (early period). This is caused by a decrease in venous blood return and cardiac output against the background of high intrathoracic pressure, and then a gradual increase in blood pressure, often exceeding its initial level (late period), under the influence of compensatory baroreflex mechanisms. The result is excitation of the sympathetic part of the ANS and vasoconstriction, as well as a weakening of vagal influences and sinus tachycardia (decreased duration of R-R
). However, if immediately before the test the subject made deep breathing movements, then in phase II bradycardia may be observed, associated with the increased action of the vagus nerve [7]. A sudden cessation of expiratory effort 15 s from the start of the test leads to a drop in intrathoracic pressure and blood pressure (phase III). Subsequently, with the resumption of respiratory movements, the return of venous blood to the heart increases and, against the background of a persisting increased level of vasoconstriction (as a result of sympathetic activation in phase II), a rise in blood pressure is observed, exceeding its initial level (“overshoot”), and heart rate slows down.
If the compensatory physiological mechanisms for regulating blood pressure and heart rate are insufficient, the described phasing when performing PVV may be disrupted, and the reactions of hemodynamic parameters may be distorted, which is observed in various pathologies of the ANS.
Analysis of parameters characterizing various phases of PWV (see Table 1)
, did not reveal significant differences between healthy individuals and patients with VZV for most of them, with the exception of the “2” pressure index on the test
(see Table 1; Table 2)
.
In patients with VZV, the value of index “2” (i.e., the increase in blood pressure in the “late period” of phase II) on average for the group turned out to be less than in healthy individuals (see Fig. 1, 2)
.
During visual analysis, a significant change in the shape of the mean blood pressure curve, consisting in the fact that by the end of phase II of the test, blood pressure did not reach the initial level, was recorded in 10 out of 30 patients with VZV (i.e., 33%) (see Fig. 2)
, and not a single healthy person.
The differences in the frequency of detection of this phenomenon between the two groups are significant (see Table 2)
.
The indices we analyzed are used to identify damage to the sympathetic part of the ANS and the degree of its severity [4]. The magnitude of the decrease in average blood pressure (index “1”), the possibility of restoring this indicator by the end of phase II of PPV (index “2”), the residual value necessary to achieve its initial level (index “3”) are accepted as quantitative and qualitative criteria "sympathetic deficiency" assessments. According to the results of the study by P. Novak [4], the index “3” of all the studied indicators in the analysis of PVV was optimal for assessing the sympathetic link of blood pressure regulation, since it made it possible to clearly distinguish healthy individuals from patients with “sympathetic insufficiency” and was associated with orthostatic hypotension , as well as the degree of its severity.
In our work on index “3”, no significant differences were found between patients with VZV and healthy individuals. This may be due to the fact that, unlike the study by P. Novak, in our study the patients had no signs of classical orthostatic hypotension (decrease in systolic blood pressure >20 mm Hg) during an active orthostatic test.
There are differences of opinion regarding the presence of autonomic pathology in patients with VZV. It is believed that people susceptible to VZV do not have true damage to the ANS when using traditional criteria for assessing its function, and the existing symptoms are explained in terms of a hyperbolically expressed reflex response, leading to bradycardia and arterial hypotension [8]. At the same time, a number of clinical and experimental works [9-15] show that using other methods for assessing the regulatory capabilities of the ANS (analysis of heart rate variability indicators, microneurographic study of the sympathetic activity of the peroneal muscles, impedance cardiography, myocardial scintigraphy with metaiodobenzylguanidine labeled with radioactive iodine ) signs may be revealed that indicate an insufficient contribution of the sympathetic component to the regulation of the activity of the heart and blood vessels.
To truly judge the severity of damage to the ANS, a comprehensive analysis of the functioning of its two parts is necessary - sympathetic and parasympathetic. According to the results of our work, between patients with VZV and healthy individuals in parameters characterizing the “vagal” regulation of the heart (sensitivity of the arterial baroreflex, Valsalva ratio - see Table 1
), no significant intergroup differences were obtained.
At the same time, in 9 (30%) of 30 patients, an individual analysis of the Valsalva ratio adjusted for gender and age [2] revealed its decrease (see Table 2)
. The results obtained in this work differ from the literature data [13, 15], which indicate the preservation of “vagal” influences on the sinus node in patients with VZV and even their intensification both in the resting position, lying down, and especially with the development of syncope. The reason for such differences may be both the methodological features of assessing the function of the ANS (analysis of heart rate variability) used in these studies, and the factors involved in the formation of different samples of patients.
To identify autonomic disorders, an integrated approach is usually used - several tests are performed (deep breathing test, Valsalva maneuver, test with active or passive orthostasis and sudomotor test), and when determining the severity of the detected pathology, it is customary to use special scales. PVV is the only one of those listed, the evaluation of the results of which allows us to draw a conclusion about possible disorders in both the sympathetic and parasympathetic parts of the ANS.
In general, in 16 (53%) of 30 patients with VZV, signs of autonomic disorders were identified either in the sympathetic (altered shape of the BP mean curve) or in the parasympathetic (individually altered Valsalva ratio) part of the ANS. The coincidence in the involvement of both parts in the process was stated in 3 cases. Using scales for assessing the degree of autonomic failure [2], the identified disorders in the patients included in this study can be assessed as mild.
Conclusion
When performing dosed PVV, signs of sympathetic insufficiency (impaired adrenergic regulation of blood pressure) are detected in 33% of patients with VZV, and parasympathetic insufficiency (impaired “vagal” regulation of cardiochronotropic function) - in 30%.