The heart of an expectant mother: what are the dangers of mitral valve prolapse?
The human heart is a tireless worker. On average, this muscular organ weighs only about 300 grams, but daily pumps 2 thousand liters of blood through 90 thousand kilometers of blood vessels.
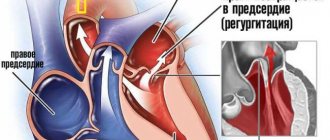
The heart consists of four chambers - the right and left atria and ventricles. Its right and left halves perform different functions. Normally, they are isolated from each other, but the atria and ventricles of the same name are separated from each other by special valves. The right atrium and right ventricle have a tricuspid valve, and the left-sided sections have a bicuspid, or mitral, valve. The purpose of these valves is to ensure proper blood flow. Namely: when the atria contract, blood should freely enter the ventricles, and when the ventricles contract, it should be sent further into the blood vessels. That is, the valves prevent reverse blood flow (regurgitation). Venous blood (saturated with carbon dioxide) enters the right atrium, and then into the right ventricle. Then it goes to the lungs, where it is enriched with oxygen and becomes arterial, acquiring a bright scarlet color. This is the so-called pulmonary circulation. Arterial blood is pumped into the left atrium and, bypassing the mitral valve, ends up in the left ventricle. From here, thanks to powerful muscle contractions, blood flows into the aorta, the largest artery in the body. Further, through the system of blood vessels, oxygen-rich blood is sent to all tissues and organs. This is a large circle of blood circulation. But if there is damage to the blood vessels, heart or valves, then malfunctions may occur in this ideal mechanism.
Mitral valve prolapse: “flapping” leaflet
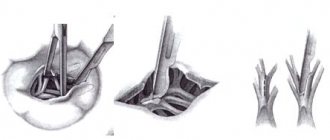
The mitral valve consists of two leaflets - anterior and posterior, which separate the cavities of the left ventricle and left atrium. This ensures proper blood flow - when the heart muscle contracts, blood should only move in one direction. With mitral valve prolapse (other names for this pathology are “flapping” or “sailing” valve, Barlow’s syndrome, late systolic murmur syndrome), its leaflets do not close completely, as if “sagging”. In this case, the left ventricle and left atrium experience a constant increased load caused by excess blood volume. In severe cases, such long-term effects on the heart can lead to serious problems.
Looking for the causes of mitral valve prolapse
What is the cause of this anomaly? Very often - heredity, namely, a violation of the development of connective tissue (connective tissue dysplasia). The fact is that connective tissue makes up half of the body’s weight and performs many functions: protective, supporting, mechanical, etc. In other words, it forms the skeleton, joints, tendons, ligaments, outer integument, forms the walls of blood vessels, and is included in all organs and systems of the body. The proper functioning of connective tissue largely depends on how the child developed in the womb. Violation of the formation of connective tissue in the fetus is the cause of many congenital diseases, including mitral valve prolapse. And very often, prolapse is accompanied by other “companion diagnoses” caused by insufficiency of connective tissue, varicose veins, prolapse of internal organs, myopia, and disorders of the nervous system.
What causes connective tissue dysplasia? The answer from doctors is unanimous: one of the main reasons is a deficiency of microelements, in particular potassium and magnesium. How can you enrich your diet with essential microelements? Include fresh meat dishes, milk, buckwheat, dried apricots, baked potatoes, spinach, bananas, and nuts in your menu. Completely eliminate simple carbohydrates - sweet pastries, sugar, as well as tea and coffee. If connective tissue dysplasia is suspected, the pregnant woman is prescribed additional potassium and magnesium supplements along with a special diet.
Other causes include previous inflammatory diseases, injuries, age-related changes, and disorders of the elasticity of connective tissue.
Types of mitral valve prolapse
Mitral valve prolapse (MVP) is divided into two groups:
anatomical (congenital);
as a syndrome associated with disruption of the nervous and hormonal systems , as well as arising against the background of various diseases - rheumatism, coronary heart disease or chest trauma.
The more significant the non-closure of its valves, the more the load on the heart increases, which has to pump a larger volume of blood. The left atrium, under constant pressure, enlarges. And during pregnancy and childbirth, when the heart is already working “for two,” additional loads can pose a threat to the health of the expectant mother and fetus.
There are three degrees of mitral valve prolapse:
- I degree – non-closure of the valves by 3–6 mm;
- II degree – 6–9 mm;
- III degree – over 9 mm;
It is also customary to distinguish the severity of reverse blood flow (regurgitation):
- I degree – regurgitation at the level of the leaflets;
- II degree – regurgitation to the middle of the atrium;
- III degree – regurgitation to the opposite side of the atrium.
Let's evaluate the risks of mitral valve prolapse during pregnancy
During pregnancy, a third circulation is added to the systemic and pulmonary circulation - the uteroplacental one. If a woman is expecting one baby, then the blood volume increases on average by 30–50%. If there are twins or triplets, then even more. Wise nature has prepared a woman’s body for such stress - during pregnancy, the size of the heart increases slightly, its muscle walls thicken. From about the 20th week, the heart rate increases - by 10-12 beats per minute. Thanks to these changes, the developing fetus is provided with all the necessary substances supplied by the blood.
As a rule, antenatal clinics require visits to a cardiologist during pregnancy, even if the expectant mother has absolutely no complaints. It is important to promptly inform your gynecologist about all existing (and past) heart problems.
In young women, minor mitral valve prolapse, as a rule, does not manifest itself in any way and is detected only by echocardiography.
With mild prolapse and slight regurgitation (grades I–II), the expectant mother usually feels normal. The pregnancy proceeds well, and the woman gives birth on her own. In this case, prolapse is considered not as a disease, but as an individual anatomical feature. Such pregnant women do not need specialized observation or treatment by a cardiologist.
If the degree of regurgitation and sagging of the mitral valve is somewhat greater, it is enough for a woman to undergo a follow-up examination with a cardiologist every 3 months.
With age, with deep prolapse, specific symptoms appear: rhythm disturbances, shortness of breath, pain in the heart. And if the expectant mother has grade III prolapse with symptoms of heart failure (such as swelling, shortness of breath, heart rhythm disturbances), then both a gynecologist and a cardiologist should monitor her condition during pregnancy.
To reduce all possible risks, it is very important for such expectant mothers to follow a strict sleep, nutrition and physical activity regime. They will have to eliminate salt from the menu and limit fluid intake to reduce the risk of swelling.
Is hospitalization necessary for mitral valve prolapse during pregnancy?
As already mentioned, for mild prolapse, only observation by a cardiologist is sufficient.
Indications for hospitalization in pregnant women with MVP may be the development of gestosis (a complication of the second half of pregnancy, in which pressure increases, swelling and protein appear in the urine), an increase in prolapse, an acute increase in pressure in the left atrium, accompanied by shortness of breath, fainting and dull pain in the left atrium. breasts
In this case, the expectant mother is hospitalized and prescribed treatment aimed at eliminating the main manifestations of mitral valve prolapse, heart rhythm disturbances, and also preventing damage to the heart muscle.
Treatment of mitral valve prolapse
No special treatment is required for this diagnosis. Intervention is necessary only in cases where arrhythmia (any disturbance in the regularity or frequency of normal heart rhythm) or pain in the heart is observed. For these conditions, sedatives (for example, products containing motherwort and valerian) help well. If necessary, the doctor will prescribe medications to prevent arrhythmia, as well as medications containing magnesium.
Perhaps the most frequently asked question when diagnosing mitral valve prolapse is – is it possible to give birth on your own? Will the heart survive? Doctors are quick to reassure: this diagnosis is not a contraindication for pregnancy and childbirth. It is only important to monitor your well-being and remember that you are responsible not only for your health, but also for the health of your child.
Is mitral valve prolapse hereditary? Alas, yes. The presence of this anomaly in a pregnant woman is one of the most common risk factors, and in the vast majority of cases, prolapse is a congenital defect of the heart valve.
Most people with this diagnosis have close relatives with a similar pathology. Children with prolapse have a thin build, they often have disorders of the musculoskeletal system (scoliosis, flat feet, weak ligaments). They are restless and get tired quickly.
But there is also good news. Mitral valve prolapse, as a rule, does not have any significant symptoms and does not require treatment (if we are talking about degrees I and II). Often the condition of the mitral valve remains unchanged throughout life. In some cases, as the child grows, the prolapse may decrease or disappear altogether. And to a large extent this will depend on the proper nutrition of the expectant mother and baby.
With minor prolapse (grades I–II), childbirth takes place in regular maternity hospitals; special observation in this case, as a rule, is not required.
In more serious cases, you will have to give birth in a specialized maternity hospital, which delivers births to women with serious cardiovascular diseases. The team of doctors, in addition to the obstetrician-gynecologist, neonatologist and anesthesiologist, also includes a cardiologist who closely monitors the work of the mother’s heart. If there are indications, the expectant mother undergoes a caesarean section.
Why is valve prolapse dangerous and its types?
Basically, heart valve prolapse is not expressed by any symptoms, and is detected by chance, during examination for other reasons. But some patients may feel pain in the heart area with vegetative manifestations (especially women), dizziness, fainting and lightheadedness, increased fatigue, rapid heartbeat and interruptions in heart function, a feeling of incomplete breathing and shortness of breath, an unreasonable feeling of anxiety, frequent nosebleeds, as well as a slight increase in body temperature. The cause of these manifestations is poor blood clotting, which is caused by a violation of the structure of connective tissue fibers.
Heart valve prolapse usually has a favorable course and a person with this pathology, as a rule, does not need special treatment. But still, heart valve prolapse should not be treated as a harmless disease. In some cases, severe forms of prolapse can cause serious complications in the heart - increased arrhythmia (which can cause sudden death), thromboembolism and infective endocarditis. If these complications occur, urgent medical treatment or surgical intervention is necessary.
There are two types of heart valve prolapse: primary and secondary.
Primary prolapse
is congenital and is often inherited. It is caused by a genetic defect in the structure of the connective tissue of the valve leaflets and chordae tendineae and is called myxomatous degeneration. People with the pathology of congenital prolapse often exhibit the following signs: a long, thin face, tall, long arms and legs, thin and elastic skin, hypermobility (too mobile joints), squint with poor vision. But nevertheless, congenital prolapse does not cause significant disruption of blood circulation and treatment for this is not required.
Secondary prolapse
heart valves is acquired. It occurs with myocardial infarction, rheumatism, as a result of chest trauma and other reasons. In secondary prolapse, sagging of the valve leaflets can cause rupture of the chordae tendineae or inflammation.
MVP (Mitral Valve Sagging)
Sagging (prolapse) of the mitral valve is relatively common in clinical practice.
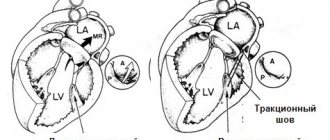
MVP is the sagging of one or both mitral valve leaflets into the cavity of the left atrium during systole at least 3 mm above the plane of the atrioventricular orifice. There are primary (idiopathic) and secondary MVP. The causes of secondary MVP are rheumatism, acute myocardial infarction, chest trauma and some other diseases in which the mitral valve chords detach and the leaflet begins to sag into the cavity of the left atrium.
Chest trauma causes acute chordal rupture and the development of severe mitral regurgitation with the clinical picture of acute left ventricular failure. This is often the cause of death.
Acute posterior myocardial infarction affects the posterior papillary muscle. This leads to separation of the chords, and prolapse of the posterior leaflet of the mitral valve develops.
Diagnostics
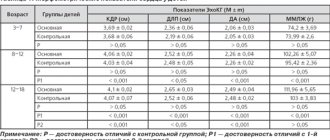
The main method for diagnosing MVP is echocardiography. It is customary to divide MVP into 3 degrees depending on the depth of prolapse:
- I stage -3−6 mm below the valve ring,
- II stage - 6−9 mm
- III degree - more than 9 mm. \
It is also customary to divide MVP into organic (with myxomatous degeneration) and functional (without myxomatous degeneration). This division is more correct, since the likelihood of developing complications depends on the presence of myxomatous degeneration.
Myxomatous degeneration is a complex of morphological changes in the mitral valve leaflets, corresponding to the “weakness” of the connective tissue, which is expressed in the thickening of the leaflet by more than 4 mm and a change in its echogenicity. MVP with myxomatous degeneration is one of the causes of stroke in young people in the absence of arterial hypertension. Myxomatous changes in the mitral valve leaflets can be the basis for the formation of micro- and macrothrombi. Strokes in these patients are of thromboembolic origin, and therefore, for persons with MVP and myxomatous degeneration, a number of authors recommend daily intake of small doses of acetylsalicylic acid. Another reason for the development of acute cerebrovascular accidents in MVP is bacterial endocarditis.
Treatment
Recently, it has been proven that patients with MVP have magnesium deficiency and it has been proposed to treat them with magnesium preparations.
For complaints of palpitations or chest pain, beta-blockers are prescribed; for RI disorders, aspirin and warfarin are prescribed. In patients with severe mitral regurgitation, if there are symptoms of heart failure, cardiac catheterization is offered as surgical treatment. If a rupture of the subvalvular chordae with the development of acute mitral regurgitation is suspected, mitral valve repair with a good long-term prognosis is indicated.
In case of severe MVP, echo-CS dynamics is recommended up to 2 times a year, examination by a therapist or cardiologist up to 3-5 times a year. When treating MVP, it is necessary to normalize work and rest, daily routine, and sleep duration.
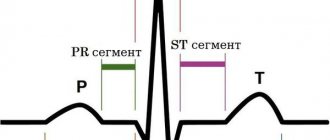
The question of playing sports is decided individually. It is allowed to lead an active lifestyle; swimming, skating, skiing, and cycling are recommended. Wrestling, jumping, lifting barbells, and weight training equipment are not recommended. If mitral regurgitation, ventricular heart rhythm disturbances, or prolongation of the QT interval are detected on the ECG, it is recommended to limit physical activity and sports.
General restorative, non-drug therapy is recommended. Psychotherapy, auto-training, physiotherapy, water procedures, and spinal massage are prescribed. Treatment of chronic foci of infection is mandatory. Herbal medicine with sedative herbs, tincture of valerian and motherwort are very useful. Pregnancy with MVP is not contraindicated.
It is also recommended for patients with MVP:
- follow a diet high in magnesium (legumes, almonds, cocoa, oatmeal) and vitamins;
- perform physical training without overload;
- visit a doctor once every 3-5 years, even if there are no complaints.
Book an echocardiogram
Functional diagnostics doctor - Andrienko Olga Leonidovna