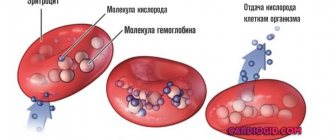
Each element of the blood performs its own function in the body, which is why it is so important that their levels remain at optimal levels. Small, anucleate platelets of blood called platelets take part in such an important process as blood clotting. They are responsible for the formation of a blood clot at the site of vessel damage in order to stop bleeding, support the constriction of blood vessels and their nutrition, and participate in immune processes and dissolution of the clot. That is, the rate of blood clotting and wound healing depends on their quantity and quality characteristics.
A condition characterized by low platelet levels is called thrombocytopenia. It can be observed in both adults and children. If, after taking a blood test, it is discovered that the child’s platelets are low, the cause should be determined and treatment should begin.
Role in the body
Despite the fact that more than 65% of people have been tested for these elements at least once in their lives, not everyone knows what their function is in the body. In professional language, platelets are often called thrombocytes, and their main task is to ensure timely blood clotting.
When a capillary is damaged, platelets ensure the formation of a clot, blocking the wound and thereby stopping the bleeding process. The number of these cells determines how quickly blood will stop moving from cuts and scrapes. The platelet level is determined using a complete blood count.
Functions and role of platelets
Platelets are small plates that are part of the blood. They prevent the formation of blood clots and protect blood vessels. If the walls of a capillary or vessel are damaged, platelets accumulate around the diseased area and form a clot.
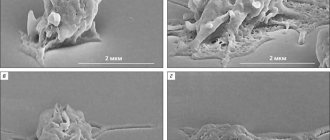
The life cycle of platelets begins from the moment they are separated from the red bone marrow and lasts about 8-10 days. At this time, the blood platelets retain their spherical shape and move freely through the vessels. The destruction of dead cells occurs in the liver and spleen.
Blood clotting depends on the number of platelets in its composition. To eliminate damage to the endothelium, they are deformed, acquiring a star shape. Layering one on top of the other, platelets form a blood clot. The rapid formation of a blood clot is facilitated by coagulation proteins released into the blood.
Platelets perform four main functions in the human body:
- The angiotrophic function ensures tissue integrity. When blood platelets are destroyed or interact, biological substances are produced that serve as food for the walls of blood vessels.
- The hemostatic function is to constrict blood vessels when damage occurs. Platelets accumulate in the resulting holes, thereby forming platelet plugs. This makes it possible to narrow the channel passage to avoid the leakage of biological fluid.
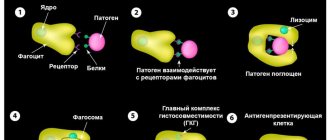
- The phagocytic function allows platelets to fight the development of pathogenic microorganisms. They attach to the walls of bacteria and inhibit their vital activity. Thus, the negative impact of external factors on the body is minimized, and the functioning of the immune system is stabilized.
- The regenerative function promotes the restoration of vascular walls due to growth factors. When the level of platelets decreases, the risk of blood loss increases due to the appearance of internal bleeding, since the strengthening of blood vessels will be insufficient.
Classification of pathology
International medicine distinguishes 4 stages of thrombocytopenia in children and adults:
- mild, with a platelet count from 75 to 100X10⁹/l;
- Moderate (from 50 to 74);
- moderate (from 20 to 49);
- heavy (less than 20).
If the indicator is significantly lower than normal, then the symptoms will be understandable. If a patient is diagnosed with an early or moderate stage of the disease, there may be virtually no symptoms. Usually at these stages, pathology is discovered by chance.
The main causes of the disease
Doctors say that in most cases, low platelet levels in children are temporary and result from the negative influence of environmental conditions or poor nutrition. However, sometimes a lack of platelets can be a sign of a serious illness.
Therefore, your doctor should order a comprehensive evaluation, including several tests, to determine what is causing the condition. Low platelet levels in children can be caused by reasons such as:
- Bone marrow dysfunction. This may be caused by leukemia, mumps, or medications that slow the growth of atypical cancer cells.
- Thrombocytopenic purple. In this disease, the body activates the production of antibodies against platelets, considering them foreign cells.
- Enlarged spleen (most often develops against the background of hepatitis or cirrhosis of the liver).
- Allergic reaction to food, external irritants. It is especially dangerous if this is caused by long-term use of drugs from certain pharmaceutical groups.
- Presence of infectious diseases.
- Autoimmune disorders.
- Advanced form of arrhythmia.
- Pulmonary tuberculosis.
- Endocrine system dysfunction.
- Metastases to the bone marrow.
- Toxin poisoning.
- The presence of parasites in the body.
- Cobalamin deficiency.
- Absorption of antibodies from mother to fetus through the placenta. Because of this factor, thrombocytopenia often occurs in newborns.
Why is it developing?
There are three main causes of low platelets:
- Decreased formation of anucleate cells in red bone marrow.
- Increased platelet destruction is the most common cause of low platelets.
- An abnormal distribution that results in a decreased concentration of platelets in the bloodstream.
Thrombocytopenia can be an independent disease, but often low platelets in a child are a symptom of various pathologies. The reasons may be as follows:
- infectious bacterial diseases;
- idiopathic thrombocytopenic purpura, in which platelets are destroyed due to autoimmune reactions;
- uremic syndrome;
- anemia;
- blood diseases;
- allergies (most often as a result of long-term use of medications);
- viral infections (mumps, rubella, measles, hepatitis);
- parasitic diseases;
- autoimmune reactions (lupus erythematosus);
- tuberculosis;
- poisoning due to inhalation of heavy metal vapors;
- penetration of antibodies from mother to fetus through the placenta;
- malignant diseases of the blood or bone marrow.
Symptoms
A low platelet count in a newborn can be identified by specific symptoms. The most common symptom is the appearance of pinpoint rashes on the body. If platelets decrease, the child will have nosebleeds and increased bleeding from the gums.
Other symptoms include the following:
- The urine will become reddish or pink;
- the child will have bruises on the body from ordinary touch;
- frequent headaches;
- Possible vomiting of blood;
- the stool will turn black;
- When cutting, the blood will be retained for a very long time.
Otherwise, primary thrombocytopenia appears. The pathology belongs to autoimmunology; doctors still cannot determine what factors provoke its occurrence. It is more common in children aged 2 to 6 years and develops after a viral illness or vaccination.
The disease develops quickly and is accompanied by the following symptoms:
- Petechiae and ecchymoses of various sizes and shapes are observed on the skin;
- spots on the body can be of different colors - from purple to greenish;
- the rash appears quite suddenly;
- Due to hemorrhage in the retina, the child's eyes will be constantly red.
In the acute form of the disease, the possibility of gastrointestinal bleeding cannot be ruled out.
How does it manifest?
With low platelets, the blood becomes liquid, clots poorly, and there is a danger of bleeding not only externally, but also internally. The child often develops bruises, and bruises are not needed to form them - touches are enough. The main symptoms in children are as follows:
- pinpoint rashes are observed in almost 100% of cases;
- about a third have nosebleeds;
- 20% of children have bleeding gums;
- pink or red urine due to blood in it;
- vomiting blood;
- black feces;
- With abrasions and cuts, the bleeding does not stop for a long time.
A characteristic symptom of thrombocytopenic purpura in children is the formation of hemorrhages on the body
What does a decrease in indicator mean?
If the average platelet volume is reduced, the deviation indicates the presence of a serious pathology. To help your child stay healthy, doctors must order comprehensive testing to determine what medical condition is causing the disorder.
In the absence of timely treatment, there is a high probability of serious consequences:
- Hemorrhage into an internal organ.
- Loss of large amounts of blood due to injury.
- Persistent retinal bleeding can impair vision.
- If a brain hemorrhage occurs, the child will die.
Thrombocytosis (increased platelet count) is no less dangerous; both pathologies require immediate treatment.
Normal platelet count in a child's blood
The platelet count is assessed based on the results of the analysis. In childhood, this indicator is very important, since a deviation from the norm may indicate the presence of serious diseases in the baby.
To carry out the study, blood is taken from the baby’s finger or vein. In newborn babies, blood can be taken from the heel.
During the analysis, the number of blood cells in 1 μl of blood is counted. In infants in the first five days after birth, the platelet count should be 180-490 thousand/µl. For babies under 12 months, the norm is considered to be in the range of 180-400 thousand/µl, and for children over 1 year old – 160-390 thousand/µl.
The MPV index in the analysis indicates the average platelet volume. In children under one year old, this figure is 7-7.9 fl. In children aged 1-5 years, the index is in the range of 8-8.9 fl. The normal MPV for older children is 7.5-11 fl. If the study results show that the mean platelet volume (MPV) is higher or lower than normal, the doctor will order additional tests for your baby.
Laboratory blood tests are prescribed for children during routine examinations, even when they have no external signs of illness. An unscheduled analysis is necessary if the child’s gums bleed, the bleeding does not stop for a long time when cuts occur, bruises appear, frequent pain in the legs and arms and other painful symptoms.
The level of platelets in a child’s blood is influenced by the following factors:
- Baby's age. The rate is higher in newborn babies than in older children.
- Products included in the baby's diet. Food can promote both the development of blood cells and the reduction of their number.
- Previous diseases, as well as medications used for treatment.
- Increased physical activity leads to a short-term increase in this indicator.
- At different times of the day, the content of blood platelets in biological fluid can vary within 10%.
In order for the test result to be most accurate, the following rules must be followed before taking blood:
- Platelets are elevated in an adult - what does this mean, and how to reduce them?
- the procedure must be performed on an empty stomach, so eating before taking the test should be avoided;
- a necessary condition is the absence of emotional or physical stress;
- The baby's clothing should be appropriate for the weather;
- If you are taking medications, you must inform your doctor.
Treatment options
A treatment regimen can be selected after the cause of the disease has been identified. To quickly normalize the blood cell count, it is necessary to act comprehensively.
Medicines
Taking medications from the following pharmacological categories will help increase platelet production:
- Immunoglobulins. Available in the form of a solution for intravenous administration. The positive effect is achieved due to the fact that the active components of the drug interact and destroy antigens, accelerating platelet production. The dosage and duration of treatment is determined by the attending physician.
- Corticosteroids. They regulate the activity of the adrenal glands using hormones. In turn, the adrenal glands normalize the functioning of the bone marrow, and platelet production is activated.
- Platelet transfusion. It is prescribed in the rarest cases, when the disease is in an advanced stage and the patient’s life is at risk.
Medical nutrition
The most important step in fighting disease is changing your diet. Your child should eat a proper and balanced diet to increase their platelet count. Products that worsen the situation should be excluded:
- products with added carcinogens;
- fast food;
- oranges, tangerines, grapefruits and juices;
- fatty food;
- fried and smoked foods;
- a pineapple.
The child’s diet should include lean meat (beef is best), quail eggs, sea and river fish. As a complement to the main dish, it is better to choose buckwheat, rice, beans with a lot of greens. Drink natural vegetable juices or mineral water instead of tea.
Traditional methods
The best folk remedy for thrombocytopenia is drinking nettle juice. The child should be given a medicine made from nettle juice and milk (in a 1:1 ratio). The drug is taken three times a day 30 minutes before meals.
She speaks positively about the use of sesame oil. To avoid complications, consult your doctor before starting therapy.
Specifics of treatment for newborns
The main task of doctors is to prevent the development of complications. For immunological forms of pathology, the infant is prescribed:
- Feeding with donor milk for the first 3 weeks, then breast milk is allowed (under platelet control);
- intravenous administration of immunoglobulins;
- Introduction of ascorbic acid and rutin.
In severe cases, platelet transfusion is indicated.
Thrombocytopenia in cancer patients
Thrombocytopenia is a problem that is familiar to many cancer patients. It develops due to chemotherapy: due to the use of platinum drugs (carboplatin, cisplatin, oxaliplatin) and gemcitabine. Each drug has its own mechanism for the development of thrombocytopenia:
- Platinum preparations
. These are alkylating agents that affect stem cells. Because of this, the production of platelets, as well as leukocytes and red blood cells, is suppressed; - Cyclophosphamide
. Affects the formation of megakaryocytes, from which platelets are subsequently formed; - Bortezomib
. Disturbs the process of separation of platelets from megakaryocytes; - Some medications cause platelet death
.
Radiation therapy also causes thrombocytopenia: it impairs bone marrow function, leading to low red blood cell levels. Thrombocytopenia develops especially often after radiation therapy in the pelvic area.
The likelihood of developing thrombocytopenia is even higher when radiation and chemotherapy are administered simultaneously. Certain tumors can also contribute to the development of this disease: lymphoma and leukemia. In this case, cancer cells quickly attack the red bone marrow, replacing its tissue with pathological ones. Less commonly, thrombocytopenia develops with damage to the bones, mammary glands, prostate and spleen.
When the level of platelets in the blood of cancer patients decreases, doctors need to determine the exact causes of this phenomenon. It may be necessary to change the treatment regimen or replace medications. Due to thrombocytopenia, the patient’s well-being significantly worsens, and difficulties arise in the treatment of oncology. Among them:
- When platelets decrease to less than 100*109 per liter
, the risk of bleeding increases; - Less than 50*109 per liter
– surgical interventions are not possible due to the risk of bleeding; - Less than 10*109 per liter
– multiple spontaneous bleeding occurs.
Prevention
The development of thrombocytopenia cannot be prevented; the main goal of preventive measures is to prevent relapse. The rules must be followed:
- minimize the risk of injury and skin damage;
- avoid physical activity;
- Avoid physical activity and eat a healthy diet.
A low platelet level in a child cannot be ignored. When the first signs of illness appear, the child must visit a doctor and undergo the necessary examinations. After this, appropriate treatment is prescribed.
How to treat?
Treatment begins after it is determined why thrombocytopenia has developed. If the causes of low platelets are other diseases, appropriate treatment is prescribed, and their levels return to normal.
In case of primary thrombocytopenia, the child is prescribed bed rest; in case of bleeding of the oral mucosa, it is necessary to give chilled food. In the acute form, spontaneous recovery is possible, but the transition of the disease to a chronic form is not excluded.
Depending on the severity of the condition, treatment can last from one to several months. The main methods are as follows:
- intravenous injections of immunoglobulins;
- hormonal therapy using corticosteroids;
- administration of anti-Rhesus serum;
- transfusion of donor platelet mass;
- surgery to remove the spleen.