- November 14, 2019
- Child's health
- Svetlana Pavlova
Patients who consult a doctor are often prescribed diagnostic procedures, the most common of which is a general blood test. Some time ago, special devices called scarifiers were used for this. Their main disadvantage is pain when piercing the dermis. Today they have been replaced by more advanced devices - lancets. How to use this device? This will be discussed in the article.
What is this device?
The lancet is intended for single use when taking capillary blood for analysis. This is a specially designed special device that prevents injury to the phalanges of patients' fingers when it is necessary to repeatedly take blood for analysis.
The lancet has an ultra-fine needle that is painlessly inserted under the dermis and leaves no marks. The device is automated and is activated when you press a special button or touch the skin. Sterility is ensured by a plastic removable cap. The blood collection procedure lasts only two to three seconds.
Which glucometer is the best?
For a doctor, accuracy is important in a glucometer; for a patient, convenience and ease of use are important.
Accuracy. The accuracy of the instrument is important. International accuracy standards have been adopted for a glucometer for home use. According to ISO 15197, the error compared to the laboratory should be within 20%. This means that by taking 2 different glucometers and measuring blood with them simultaneously, you can get results that differ by up to 40%. There is no need to be scared, it is better to choose one device and use it constantly, this will give a real picture of your sugar level over time and will help you and your doctor.
Convenience. The device should be as gentle and comfortable as possible. A device with capillary blood sampling is considered more convenient. After the puncture, you dip the edge of the test strip into a drop of blood and it itself absorbs the required amount. There are devices where you need to drop a drop of blood into a special field on the test strip; this is more difficult to do, especially for an elderly person.
The display should be bright, with large font so that the readings are easy to read. It is advisable to choose a device where you do not need to enter the coding for calibration manually. This reduces the likelihood of measurement errors.
Younger users can choose glucometers that transmit readings via Bluetooth and have various software and applications. If the user is elderly and writes down data in a notebook the old-fashioned way, these functions can also be useful, but for control by relatives and the attending physician.
There are glucometers that transmit readings via Bluetooth and have various software and applications.
One of the most painful topics is the price of test strips. This is what you need to focus on when choosing a glucometer, among other characteristics. The average price category provides good quality measurements, the main thing is to take them regularly.
Also, when traveling abroad, you need to have a supply of test strips, since the models of glucometers may differ in different countries and strips purchased abroad may not fit your device.
Therefore, it is impossible to say unequivocally which device is better. It is necessary to know who will use it and under what conditions. Based on this price-quality ratio, make a choice.
Disposable lancets
Modern devices used to take blood for analysis greatly facilitate the procedure. There is no discomfort or pain at all. They are most suitable when you need to frequently monitor your blood composition. How to use a disposable lancet?
Step-by-step instruction:
- Use an alcohol wipe to disinfect the puncture site.
- Turn clockwise and remove the protective cap.
- Load the needle holder and adjust the puncture depth.
- Place the device firmly on the side of your fingertip and press the “Start” button. There are models that are triggered when the body comes into contact with the surface of the dermis.
- Using gentle pressure on your finger, draw blood.
The disposable device cannot be reused; immediately after the procedure is completed, the needle is blocked and the device must be disposed of. This ensures that the infection cannot spread from person to person.
Main advantages
Lancets for collecting blood are a new development that greatly facilitates the procedure for collecting biological material from a patient for conducting a general blood test and assessing the glucose concentration in it. The advantages of this device include the following:
- after the procedure is completed, there are no wounds or bruises left on the patient’s skin;
- The technique is painless, the risk of wound infection is minimal;
- needle penetration does not depend on how hard the medical worker presses. There is no human factor here (hand trembling, etc.);
- The lancet is packaged in a sterile container; the packaging is opened immediately before use. Before blood is collected, it is disinfected using special gamma radiation;
- the procedure lasts a few seconds, but this does not affect the accuracy of the blood test;
- The device can be used both in the laboratory and at home, for example, to measure the amount of sugar in patients suffering from diabetes;
- The puncture site heals very quickly, which is convenient for use in small children and newborns.
The device is considered safe and does not cause pain to a person
When performing an analysis using a scarifier, the accuracy of the study is somewhat compromised, because the blood interacts with air. The lancet provides the most reliable data, since here the material enters directly into the device.
Important! The emotional state of a child or adult can affect the composition of the blood, which is why the aspect that the lancet does not cause pain or discomfort to the patient is so important.
Devices for children
They stand out in a separate category and have very thin and sharp needles so that the baby does not experience fear before the procedure, which worsens blood counts. How to use children's lancets?
They are used according to the following scheme:
- unscrew and remove the cap;
- press the body of the device tightly against the child’s finger - it will work automatically;
- Using gentle pressure, select the required amount of biomaterial.
As you can see, using the lancet is not difficult.
Following the procedure, the needle is automatically retracted into the body and locked. All devices for collecting blood for analysis in children are disposable and are disposed of after use. But before this manipulation they are disinfected in an autoclave, after which they become safe garbage that can be thrown away.
Features of recycling
All consumables for injection procedures and sampling of biomaterials, including capillary blood, must be disposed of after use. In particular, the reuse of disposable lancets in most cases is impossible due to the design features: after performing a puncture and taking a sample, the needle is automatically hidden inside the body and blocked there. This is done in order to prevent the spread of infection. At home, when using universal lancets together with a glucometer, usually only the needles are changed, which are also a source of danger. They should not be thrown into the bin with normal household waste.
In medical institutions, all consumables that were used for collecting and conducting blood tests, syringes and other accessories after use are placed in special tanks for class B medical waste. Before disposal, they are disinfected under high temperature, chemicals or other means. Only after they become safe for people and the environment are they destroyed.
Accu-Chek FastClix Lancets
These devices, easy to use, have been specially designed to painlessly prick a finger or earlobe to obtain a drop of blood. The depth of the puncture is selected depending on the individual characteristics of the skin. The structures are intended for individual use only to avoid infection.
When installing or replacing you must:
- twist the protective cap;
- when replacing, remove the old lancet by pulling the sliding sector;
- place the new lancet in the holder and press until it stops;
- screw on the cap;
- make sure that the notch on the cap is aligned with the center of the semicircular cutout on the sliding sector.
Content:
- What is a glucometer and how it works?
- How to properly set up a glucometer?
- How to use a glucometer correctly?
- Short description
Any disorders of carbohydrate metabolism, including diabetes mellitus type 1 or 2, require monitoring of blood glucose levels. For this purpose, a glucometer is used. How to use the strips and the device itself, and calibrate it to obtain reliable results is indicated in the instructions. In general, most devices have similarities in the principle of glucose determination and use.
Instructions for using Accu-Chek FastClix
How to use the lancet? To obtain a drop of blood you must:
- Conduct preliminary preparations. Wash your hands with warm water and soap and wipe dry. This promotes hygiene and better blood circulation. The puncture is made on the surface of the fingertips on the side, where there is minimal pain.
- Depth selection. There is a puncture depth regulator on the cap of the device. When using the device for the first time, set it to the mark with value 2. After that, check whether you did it correctly.
- Taking blood. Press the cocking button all the way. The readiness of the device for operation is determined by the yellow eye in the transparent window of the shutter button. Press the device against your fingertip and press the shutter button.
If a drop of blood does not form, increase the depth of the puncture and repeat the steps again.
Modern devices for self-monitoring of blood sugar levels
Determining blood glucose levels is one of the most common tests performed by clinical diagnostic laboratories. In addition to various laboratory methods for analyzing glucose levels, there are a large number of portable devices that operate on the principle of “dry chemistry”. We are talking about so-called glucometers, which allow you to carry out this procedure at home. The choice of device in each individual case depends on many objective and subjective factors, which are discussed in this article.
Historical reference
More than 100 years ago, it was discovered that eating carbohydrates increases the amount of sugar in the urine, and people with diabetes mellitus (DM) were advised not to eat foods containing carbohydrates as a treatment. The only method of monitoring the effectiveness of such restrictions was frequent determination of sugar levels in the urine using Benedict's reagent, a solution containing copper sulfate, citric acid and sodium carbonate. To carry out a qualitative analysis, it was necessary to add 8 drops of urine to 5 ml of the reagent in a test tube and boil the solution, holding it directly over the fire for 2 minutes. In this case, urine glucose was oxidized, as a result of which the intensity of the blue color of copper sulfate decreased, the color of the solution changed, and a colored precipitate formed. Color and sediment were indicators of urine glucose levels. A clear blue color without sediment indicated the absence of glucose, while changes in color - from green with a yellow sediment to deep orange or red - were directly related to the amount of sugar in the urine.
Determination of the level of glycosuria became most popular after the discovery of insulin in 1921 and was subsequently used in the treatment of diabetes. However, until 1941, that is, until Walter Compton and Maurice Treneer invented the first chemical test with a dry reagent in the form of Clinitest reagent tablets, there was no simpler way to control glycosuria. The tablets contained the same reagent as in the Benedict test, but in dry form with the addition of sodium hydroxide. The liquid needed to trigger the reaction was urine. The tablet was dropped into a small amount of urine in a test tube and an immediate reaction occurred, producing enough heat to cause it to boil. The glucose in the urine was oxidized, and the blue color of the copper sulfate was reduced, causing the solution to change color from blue to green to yellow and orange. The semi-quantitative result was assessed by visual comparison of the resulting color with the standard scale.
The first test strips with a “dry reagent” were demonstrated in 1956. We are talking about the Clinicix system - a test strip for determining glucose in urine. All necessary reagents (glucose oxidase, peroxidase and chromogen) were encapsulated in the porous strip base. The same enzyme principle was used in the 1964 development of Dextrostix, a disposable test strip for semi-quantitative blood glucose testing. The main component of the dry reagent contained three layers: a supporting layer, a reflective zone and a reacting zone. The water necessary to start the reaction was contained directly in the component under study (blood, plasma, serum, urine). The color obtained as a result of the reaction could be assessed visually by comparing it with a printed reference color scale. This allowed semi-quantitative analysis, the result of which depended largely on the user's ability to correctly compare the color of the test field with the sample. Many patients with diabetes who have vision problems could not correctly evaluate the results obtained, especially if there was a slight transition from blue to green.
Urinary glucose test strips are still used as a screening method and very rarely as a diagnostic method to adjust diabetes treatment. Despite the low cost of determining the level of glucosuria, this method does not allow prescribing high-quality treatment for diabetes, since it does not make it possible to detect hypoglycemia, and the results of the analysis depend on many factors affecting the renal excretion of glucose in the patient.
Considering the difficulties of qualitative subjective analysis of glycemic levels using visual test strips in patients with vascular and neurological complications of diabetes, manufacturers have developed devices for assessing changes in the color of the test strip.
Reflectometers
Reflectometers appeared in 1969 and were introduced by Bayer AG. They measured the reflected light from a colored test strip and converted the signal into a quantitative expression of glucose concentration. The first instruments were heavy and bulky, required manual calibration, and the test strip had to be rinsed and blotted before being placed in the instrument. The main advantage of these glucometers is that the measurement results were no longer semi-quantitative and, despite the wide analytical range, measurement errors that depended on the user’s ability to visually assess the color of the strip were excluded. However, the problem of misinterpretation of results was still present if the examiner did not scrupulously follow all manufacturers' instructions during the test. Thus, it was up to the user to comply with the rules for storing strips, programming the code, and obtaining a drop of blood of the required size (about 50 μl). It was also quite difficult to adhere to the time frame for applying a drop of blood to the test strip and the technique of erasing it from the test field before determining the color. If the test strip was not placed correctly in the meter, the test results would be unpredictable. These glucometers were designed in such a way that a chemical reaction to the test field occurred after placing the test strip in the glucometer, which subsequently required mandatory monitoring of the cleanliness of the optical zone of the device.
Nowadays, reflective glucose measurement systems are compact, easy to use and require minimal user intervention, which minimizes subjective errors. The use of new technologies (the color analyzer is placed under the test strip) eliminated the need to wipe off blood from the strip. Devices with automatic time counting appeared, and the amount of a drop of blood required for analysis was reduced to 1–2 μl. In addition, glucometers began to automatically warn the user about possible errors when measuring glycemia.
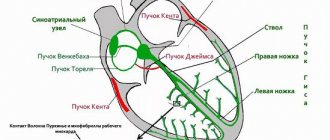
Biosensors
Biosensors appeared in the late 80s. last century and became the first generation of test strips using an “indelible” system for determining glycemia. A biosensor is a bioelectrochemical transducer that, together with a portable analyzer, registers the electrical signal produced during a biochemical reaction. Many devices use test strips with a sensor that includes an enzyme that very specifically accelerates the process of glucose oxidation and a mediator involved in the redox reaction.
The first glucose sensor, ExacTech (MediSense), used an electrode containing glucose oxidase as an enzyme and ferrosene as a mediator. The test field of the sensor consisted of two electrodes in the form of conductive “tracks”:
- bioactive working electrode containing glucose oxidase and ferrosene;
- a second electrode that functions as an auxiliary electrode and a reference electrode simultaneously.
The latest model sensors have three electrodes: reference, base and trigger, where the third electrode prevents high concentrations of uric acid, ascorbic acid and paracetamol from influencing the glucometer readings by “subtracting” electrons from the metabolites of the listed substances. The presence of excess (compared to normal) content of these compounds may slightly increase the level of glycemia.
When a drop of blood is placed on the test field, glucose is oxidized to gluconolactone and the glucose level decreases. The released electrons are absorbed by the mediator ferrosene, and the resulting compound is oxidized at the electrode. The flow of electrons is proportional to the blood glucose level.
A drop of blood in biosensors is applied to an electrode outside the device itself and does not come into contact with the internal component of the glucometer.
Principles of glucose measurement
The first chemical tests were too nonspecific, since they measured not only glucose but also other sugars and required the application of a very large drop of blood. Today, the measurement is more specific and less influenced by other sugars. Three enzymes are currently used to measure glycemia:
- glucose oxidase;
- hexokinase;
- glucose dehydrogenase.
The glucose oxidase method is more susceptible to the influence of various drugs and other endogenous blood components than both other methods.
Glucometers
The table shows reflex and biosensor systems for measuring glucose registered in Russia. When used correctly, according to the manufacturer's recommendations, all of them generally reflect fairly accurate blood glucose levels.
The criteria for choosing a device depend on the frequency of its use by the patient, the cost of the device and test strips, as well as other factors, which include: the size of the device and display, type of batteries and ease of replacement, ease of use, availability of memory, warranty service. In addition, the following factors are taken into account.
Blood volume
Over the years of using glucometers, the volume of blood required to correctly determine glycemic levels has decreased significantly. The first generation test strips required at least 50 µl of blood; in the latest generation glucometers this volume is less than 2 µl. The user should be aware that some blood glucose meters or sensors may give low results if the blood drop is not large enough. In addition, the result will be erroneous if an additional drop of blood is applied to the test field if the first sample was insufficient.
In practice, patients often confuse the two main methods of blood collection. The first is when blood is dripped onto a strip - in which case the volume of blood usually must be controlled by the person measuring it. The second (capillary) is when, when touching a strip inserted into the glucometer, a drop of blood is itself absorbed in the required volume, while the glucometer “knows” when to start measuring and when to finish it. That is why the first method requires up to 50 µl, and the best samples of the second method require 0.3–3 µl. Some patients, without reading the instructions, try to drip blood, as they have long been accustomed, onto the sensor strip and a week later they come to replace the glucometer, despite the complete working order of the device.
Thus, it should always be taken into account that if the measurement procedure is performed correctly, any glucometer will give an adequate result.
Expiration date of test strips and their storage
Test strips are individually packaged or placed in a special tube that usually contains silica gel (a desiccant) to prevent excess moisture from affecting the reagent. The user must ensure that the test strip container is closed immediately after removing the strip, as remaining test strips must be stored at a specified temperature and not exposed to excessive heat or cold. Although test strips are stable at room temperature and have a shelf life of about two years, improper storage can accelerate the deterioration of the reagent, causing incorrect blood glucose readings. Test strips should not be used if they have exceeded their expiration date. It is also important to know that after opening the tube, the shelf life of the strips, as a rule, does not exceed 3-4 months; for the Accu-Chek Active and Accu-Chek Go test strips - up to 1-1.5 years (regardless of moment of opening the tube).
Effect of hematocrit
When the blood plasma interacts with the dry reagent of the test strip, it wets the dry chemical agents, which initiates the reaction. This mechanism is influenced by hematocrit when whole blood is used. Blood samples with a high hematocrit or increased viscosity may affect the rate or amount of plasma absorbed and mechanically impede glucose diffusion, resulting in underestimation of glycemic values. Accordingly, a sample with a low hematocrit overestimates the blood glucose level.
Limitation of use
The correct procedure for applying the blood sample to the test strip must be used with each test, so blood glucose meters that use whole blood are not suitable for some patients. Such glucometers cannot be used in patients with hyperosmolar hyperglycemia, since glycemic values may be significantly underestimated.
Please note that some medications and other substances specified by the manufacturer may affect the interpretation of measurement results. Reflective or biosensor glucose meters that use the glucose oxidase method of measuring glycemia are affected by high levels of blood lipids or bilirubin, paracetamol, vitamin C or uric acid.
Safety or Cross Contamination
The safety of using the device does not directly affect the performance of glycemic measurements, but the health of the patient and medical staff may be subject to cross-infection during the analysis. Safety is especially important when using a device on multiple patients (eg in a hospital setting), where you need to be sure that the selected device and lancets are the most appropriate for the situation and do not transmit infection. Medical staff should change test strips and, if necessary, clean the test zone of the device between blood glucose measurements in different patients, which is especially important when using glucometers in specialized children's hospitals to eliminate the risk of cross-infection.
Instrument calibration
Although blood glucose meters and sensors are calibrated by the manufacturer, users should also be aware of the calibration information for each pack of test strips or electrodes. Typically, code changes are manually made to the program using a special code button on the device. Because calibration has a significant impact on blood glucose results, manufacturers have attempted to minimize operator error when manually changing the code in the following ways:
- information about the code is in the test strip; the glucometer “reads” it independently;
- Each batch of test strips has a calibration key that is inserted into the meter;
- Each batch of test strips contains calibration strips to transfer the necessary information to the meter.
Almost all blood glucose meters use capillary whole blood to measure blood glucose levels. Devices calibrated with whole blood will produce different glycemic values than those obtained with a meter calibrated with plasma, which should be kept in mind when interpreting your results.
Subjective factors influencing measurement results
Glucometers are widely used by both patients and healthcare professionals, ranging from nursing staff to professional diabetologists, and test results depend on the operator's ability to follow the manufacturer's instructions. Devices for personal use should be characterized by a minimum number of manipulations and be easy to use to reduce the likelihood of incorrect blood glucose measurements. Before recommending a particular device for home use, it is necessary to determine the patient’s capabilities and skills in performing this type of manipulation. Below are some of the most common features of blood glucose testing that help minimize operator error and improve the quality of your blood glucose measurements. Systems that do not require blood removal are characterized by the lowest number of operator errors.
Advantages of modern glucometers that eliminate user error:
- minimal user participation;
- applying calibration information to an electronic chip or calibration strip;
- minimum blood volume;
- capillary blood sampling;
- automatic counting of measurement time;
- no need to wipe off blood from the test area of the strip;
- electronic warning about user errors;
- mandatory quality control of the measurement procedure.
Glucometer Glucochrome M
Specifications:
- measurement ranges - 2.2–22 mmol/l;
- power supply - 2 batteries with a voltage of 1.5 V;
- permissible external conditions - 15–35°C, up to 75% relative humidity;
- measurement principle: photometric;
- analysis time - 2 min;
- calibration - whole capillary blood;
- sample - fresh capillary blood from a finger;
- memory - 15 values;
- dimensions - 50 x 130 x 18 mm;
- weight - 95 g (including battery);
- control of operation - using control strips included in the kit of the Glucochrome M device;
- Contents: device with battery, case, test strip, instruction manual.
Advantages of Glucochrome D test strips:
- designed for both visual and automatic assessment of the result;
- assessment colors are well defined and readable thanks to the separated reactive field;
- color stability after the reaction leaves enough time to evaluate the result;
- relatively low cost of test strips and the opportunity to receive them for free in some Russian cities.
Flaws:
- the measurement results depend on the user’s ability to strictly follow the operating rules of the device;
- test strips are packaged in a tube; storage conditions for open packaging should be carefully observed;
- the analysis requires a large drop of blood - 10 μl;
- It is necessary to erase a drop of blood from the test field of the strip after 1 minute. after application;
- The optical zone of the device requires cleaning.
Glucose meter Glucocare
Specifications:
- measurement ranges - 2.2–25 mmol/l;
- power supply - 3 batteries with a voltage of 1.5 V (GP A 76);
- permissible external conditions - 15–30°C, humidity less than 85%;
- measurement principle: photochemical;
- analysis method - glucose oxidase-peroxidase reaction;
- analysis time - less than 1 minute;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 150 values;
- dimensions - 101 x 50 x 15 mm;
- weight - 58 g (including batteries);
- performance control - control strips;
- equipment - device, test strips (2 pcs.), pen for pricking the finger, 8 lancets, instructions;
- Warranty period - 3 years.
Advantages:
- memory for 150 analyzes with date and time indication;
- There is an interface to the computer.
Flaws:
- strips should be stored at a temperature of 5 - 30 ° C, in a dry place protected from direct sunlight;
- strips must be used within 3 months. after the first opening of the tube;
- Avoid direct sunlight on the test strip when performing the analysis;
- the influence of hematocrit and cholesterol and triglyceride levels on study results;
- taking orally or injecting large doses of vitamin C underestimates the true glucose concentration;
- Dehydration and kidney dysfunction may also affect test results.
Glucometer Elta-Satellite
Specifications:
- measurement ranges - 1.8–35 mmol/l;
- power supply - 1 CR 2032 battery, voltage 3V;
- measurement principle - electrochemical;
- analysis time - 45 s;
- calibration - whole capillary blood;
- sample - fresh capillary blood from a finger;
- memory - 40 values;
- dimensions - 110 x 60 x 25 mm;
- weight - 70 g;
- control of operation - using the control strip included in the device;
- coding - manually;
- complete set - device with battery, strips in individual packaging (10 pcs.), case, control strip, instruction manual;
- The warranty period is unlimited.
Advantages:
- electrochemical measuring principle;
- does not require blotting of test strips and control of measurement time;
- each test strip is packaged in a separate sealed bag;
- a drop of blood is applied outside the device;
- Each device is covered by an unlimited warranty;
- economical due to its affordable price and the use of inexpensive test strips.
Flaws:
- a large drop of blood is required - at least 5 µl;
- There is no protection system against incorrect measurement procedures.
Glucometer One Touch Profile
Specifications:
- measurement ranges - 0–33.3 mmol/l, higher results are displayed on the screen as the inscription “Hi”;
- power supply - 2 alkaline batteries, size AAA, voltage 1.5 V;
- permissible external conditions - 15–35°C, humidity 0-90% (without condensation), hematocrit 25–60%;
- measurement principle: photometric;
- analysis time - 45 s;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 250 values;
- dimensions - 109 x 66 x 30 mm;
- weight - 127.5 g (including battery);
- control of operation - using the control solution included in the device kit;
- coding - manually;
- equipment - device with battery, test strips (10 pcs.), Penlet Plus piercing pen, Fine Point lancets, control solution, case;
- Warranty period - 5 years.
Advantages:
- the test strip does not require wiping a drop of blood;
- the results obtained can be marked with the corresponding names of “events” (on an empty stomach, before breakfast, after breakfast, etc.);
- when you turn on the device for the first time, the average value of the results for 14 days appears on the screen;
- there is a function “Insulin Information”;
- You can view average results for 15 possible “events” on the screen, as well as the average blood test result for the last 30 days;
- connecting the cable allows you to transfer information stored in the device’s memory to a computer for further processing using a special computer program.
Flaws:
- it is necessary to wash the test strip holder from blood;
- it is necessary to wipe the optical zone of the test from blood;
- Applying an insufficient volume of blood is a mistake in conducting the study.
Glucometer One Touch Basic Plus
Specifications:
- measurement ranges - 0–33.3 mmol/l, higher results are displayed on the screen as the inscription “Hi”;
- power supply - 2 alkaline batteries, size AAA, voltage 1.5 V;
- permissible external conditions - 15–35°C, humidity 0–90% (without condensation), hematocrit 25–60%;
- measurement principle: photometric;
- analysis time - 45 s;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 75 values;
- dimensions - 109 x 66 x 30 mm;
- weight - 116.2 g (including battery);
- control of operation - using a test strip and control solution included in the device kit;
- coding - manually;
- equipment - device with battery, test strips (10 pcs.), pen for piercing Penlet Plus, Fine Point lancets, control solution, case, instructions and a brief test procedure;
- Warranty period - 5 years.
Advantages:
- the test strip does not require wiping a drop of blood;
- connecting the cable allows you to transfer information stored in the device’s memory to a computer for further processing using a special computer program.
Flaws:
- it is necessary to wash the test strip holder from blood;
- it is necessary to wipe the optical zone of the test from blood;
- Applying an insufficient volume of blood is a mistake in conducting the study.
Glucose meter One Touch Ultra
Specifications:
- measurement ranges - 1.1–33.3 mmol/l;
- power supply - 1 lithium battery with a voltage of 3 V (No. 2032);
- permissible external conditions - 6–44 ° C, humidity 10-90%, hematocrit 30–55%;
- measurement principle - electrochemical;
- analysis method: biosensor glucose oxidase;
- analysis time - 5 s;
- calibration - blood plasma;
- sample - fresh capillary blood from a finger, shoulder or forearm;
- memory - 150 values;
- dimensions - 79 x 57 x 21 mm;
- weight - 2.5 g (including battery);
- control of operation - using the control solution included in the device kit;
- coding - manually;
- equipment - device with battery, test strips (10 pcs.), pen for piercing One Touch Ultra Soft, replaceable cap One Touch Ultra Clear for obtaining a drop of blood from the shoulder/forearm , One Touch Ultra Soft lancets, control solution, soft sports case, instructions in Russian and warranty card;
- Warranty period - 3 years.
Advantages:
- the analysis result can be obtained in just 5 seconds;
- capillary blood sampling - only 1–2 μl. A change in the color of the test strip will confirm that the blood volume is sufficient to obtain an accurate result;
- touching the test strip does not affect the measurement result;
- the test area is located outside the device, so blood does not enter the device;
- You can choose the puncture site - hand or finger. Using a special One Touch Ultra Clear cap with a One Touch Ultra Soft piercing pen allows you to get a drop of blood not only from your finger, but also from your arm (shoulder or forearm);
- stores the results of 150 tests in memory, indicating the date and time of the test. Calculates the average result for 14 and 30 days;
- calibrated using blood plasma, so the analysis result is comparable in accuracy to the result obtained in the laboratory;
- a computer user can connect a glucometer to it and use the In Touch LifeScan program to process data on a PC. A special wire is supplied with the device. The program can be downloaded free of charge from the LifeScan website on the Internet.
Flaws:
- an opened bottle of test strips must be used within 3 months. After this period, the strips are unusable;
- high cost of the device and test strips.
Glucometer SmartScan
Specifications:
- measurement ranges - 1.1–33.3 mmol/l;
- power supply - 2 batteries No. 357 based on silver oxide with a voltage of 1.5 V;
- acceptable external conditions - 15–35°C, humidity 10–90%, hematocrit 30–55%;
- measurement principle - electrochemical;
- analysis method: biosensor glucose oxidase;
- analysis time - 15 s;
- calibration - blood plasma;
- sample - fresh capillary blood from a finger;
- memory - 150 values;
- dimensions - 79 x 57 x 19 mm;
- weight - 45.4 g (including battery);
- control of operation - using the control solution included in the device kit;
- coding - manually;
- equipment - device with battery, test strips (10 pcs.), Penlet Plus piercing pen, Fine Point lancets, control solution, soft sports case, instructions in Russian;
- warranty period - 3 years;
Advantages:
- allows analysis using a small drop of blood measuring 2.5 μl;
- capillary method of blood sampling;
- test strips are reliably protected and can be touched anywhere on the strip;
- calibrated using blood plasma for easier comparison with laboratory results;
- stores the results of 150 tests in memory, indicating the date and time and automatically calculating the average result for 14 days;
- The test area is located outside the device, so blood does not enter the device.
Flaw:
- high cost of test strips.
Accu-Chek Active glucometer
Specifications:
- measurement ranges - 0.6–33.3 mmol/l;
- power supply - 1 lithium battery type CR2032;
- permissible external conditions - 10–40°С, humidity 0–85%;
- measurement principle: photometric;
- analysis time - 5 s;
- calibration - whole blood;
- sample - fresh capillary blood;
- memory - 200 values;
- dimensions - 115 x 40 x 22 mm;
- weight - 45 g (without battery);
- performance control - control solution;
- coding - code plate;
- equipment - device with battery, 10 test strips, Accu-Chek Softclix finger pricking pen, 10 Accu-Chek Softclix lancets, case, instructions in Russian;
- Warranty period - unlimited.
Advantages:
- has the function of measuring blood glucose levels obtained from alternative places: forearm, shoulder, palm of the thumb, thigh or calves;
- capillary method of blood sampling;
- blood drops less than 2 μl;
- there is an automatic on/off function;
- additional memory functions: values indicating the time and date of measurement. Calculation of average values for 7 and 14 days;
- wireless data transfer to a PC via infrared;
- unlimited warranty period.
Flaws:
- galactosemia, ketoacidosis, dehydration, increased bilirubin levels (up to 20 mg/dl), as well as the administration of solutions of oligo- or monosaccharides, ascorbic acid, solutions containing icodextrin, can lead to an incorrect result.
Glucose meter Accu-Chek Go
Specifications:
- measurement ranges - 0.6–33.3 mmol/l;
- power supply - 1 lithium battery type CR2030 or DL2430;
- permissible external conditions - 10–40°С, humidity 0–85%;
- measurement principle: photometric;
- analysis time - 5 s;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 300 values;
- dimensions - 113 x 46 x 22 mm;
- weight - 55 g (without battery);
- performance control - control solution;
- coding - code plate;
- equipment - device with battery, 10 test strips, Accu-Chek Softclix finger pricking pen, 10 Accu-Chek Softclix lancets, 1 Accu-Chek Softclix device attachment, case;
- Warranty period - unlimited.
Advantages:
- capillary method of blood sampling;
- the ability to obtain a drop of blood from alternative sites (for example, shoulder, forearm);
- there is no direct contact of the device with blood;
- the presence of a mechanism for removing the test strip from the device ensures that there is no direct contact with blood or the used test strip;
- turns on and off automatically, results are also saved automatically;
- “alarm clock” function: you can set the sound signal to sound three times at different times of the day;
- Hypoglycemia Alert: You can set both a visual and an audible alarm to alert you when your blood glucose levels are unusually low.
- memory for 300 results (along with the date and time of the analysis);
- infrared interface for transmitting data to a personal computer or laptop on which a program for analyzing the results is installed (Accu-Chek Pocket Compass software);
- You can calculate the average of your blood glucose results over the past 7, 14, or 30 days;
- unlimited warranty period.
Flaw:
- high cost of the device and test strips.
Glucometer Ascensia Elite
Specifications:
- measurement ranges - 1.1–33.3 mmol/l;
- power supply - 2 lithium batteries with a voltage of 3 V (CR2030 or DL);
- permissible external conditions - 10–40°С, automatic temperature compensation using built-in thermal strips, humidity 20–80%;
- measurement principle - electrode-sensor technology;
- analysis time - 30 s;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 20 values;
- dimensions - 81 x 51 x 14 mm;
- weight - 50 g (without battery);
- operation control - test strip;
- coding - using a code test strip;
- equipment - device with batteries, 5 test strips, Microlet finger pricking device, 5 lancets, test strip, case, instructions, warranty card;
- Warranty period - 5 years.
Advantages:
- electrode-sensor technology for measuring glycemia;
- capillary method of blood sampling;
- volume of a drop of blood—2 μl;
- automatic on/off function;
- the device does not have a single button, so it is very easy to learn and use;
- Each test strip is hermetically sealed, the use of one strip does not affect the shelf life of the remaining strips.
Flaws:
- small amount of memory;
- there is no interface to the computer.
Glucometer Ascensia Entrust
Specifications:
- measurement ranges - 1.7–30.6 mmol/l;
- power supply - 1 lithium disk battery with a voltage of 3 V (CR2032);
- acceptable external conditions - 18–38°C, hematocrit 30–55%;
- measurement principle - electrode-sensor technology;
- analysis time - 30 s;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 10 values;
- dimensions - 100 x 58 x 21 mm;
- weight - 64 g;
- operation control - control strip;
- coding - electronic chip;
- equipment - device with battery, 5 test strips, code card, control strip, microlet finger pricking device, 5 lancets, case, user manual, quick guide;
- Warranty period - 5 years.
Advantages:
- electrode-sensor technology for measuring glycemia;
- capillary method of blood sampling;
- automatic on/off function;
- large strip field - easy to insert into the device and comfortable to hold in your hand;
- two-step measurement procedure;
- relatively low cost of the device and test strips.
Flaws:
- small amount of memory;
- there is no interface to the computer.
Glucometer Ascensia Confirm
Specifications:
- measurement ranges - 0.6–33.0 mmol/l;
- power supply - 1 lithium disk battery with a voltage of 3 V (CR2025);
- permissible external conditions - 10–40°C, humidity 10–80%;
- calibration - whole blood;
- sample - fresh capillary blood from a finger;
- memory - 100 values;
- dimensions - 110 x 75 x 17 mm;
- weight - 50 g;
- coding - manually;
- equipment - device with battery, 10 test strips, Microlet finger pricking device, 5 lancets, instructions;
- Warranty period - 5 years.
Advantages:
- the device is equipped with a disk containing 10 test strips at once;
- capillary method of blood sampling;
- blood drop volume - 3 µl;
- average glycemic value for 14 days;
- ability to connect to a computer.
Flaw:
- high cost of the device.
Glucometer Super Glucocard 2 (Super Glucocard II)
Specifications:
- measurement ranges - 1.1–33.3 mmol/l;
- power supply - 2 lithium batteries with a voltage of 3 V (CR2032);
- measurement principle - electrochemical;
- analysis time - 30 s;
- calibration - plasma/serum;
- sample - fresh capillary blood from a finger;
- memory - 20 values;
- dimensions - 51 x 87 x 14.5 mm;
- weight - 45 g;
- operation control - control strip;
- coding - coding strip;
- equipment - device with battery, 10 test strips, coding strip, control strip, Multilancet finger pricking device, 10 lancets, case, instructions.
Advantages:
- capillary blood sampling;
- the ability to apply a drop of blood to the test strip outside the device;
- blood drop volume - 3 µl;
- the device has no buttons;
- automatic on/off function;
- Each test strip is packaged in a separate sealed bag.
Flaws:
- small amount of memory;
- there is no interface to the computer.
N. Yu. Arbatskaya, Candidate of Medical Sciences, City Clinical Hospital No. 1 named after. N. I. Pirogova, Moscow
Types of lancets for glucometer
These devices are used to draw blood from a finger or earlobe and consist of a sterile needle inserted into a handle. The manufacturer of the device describes in detail how to use the lancet in the attached instructions.
All lancets are divided into two types:
- Automatic - a device with replaceable needles that automatically determines the depth of the puncture and draws blood. Equipped with protection - you cannot use the same needle twice. Works only in contact with the surface of the skin. After using the needles, the drum with them needs to be replaced.
- Universal - consists of a small needle and practically fits any glucometer, otherwise the packaging indicates the types to which it is not suitable. For protection, reliability and convenience, devices are often available with a protective cap and a piercing depth regulator.
Why does the device not cause pain?
Many people are intimidated by the very sight of a scarifier. The procedure seems especially scary to children, and many parents are faced with the tears of their child. The lancet needle is very small. Thanks to this, pain is practically absent. Its diameter is only 0.25 - 0.8 mm, and its length is no more than 1.8 mm. Such tiny sizes do not cause pain, and the puncture wound heals within a few hours. This feature of the device is of great importance for infants and patients who are afraid of injections.
Lancets for the Van Touch Select Plus glucometer
For a compact and easy-to-use glucometer from this company, they use a special device for piercing the skin, which regulates the depth of the puncture. Let's look at how to use lancets for a glucometer of this model, step by step:
- Wash your hands thoroughly and wipe dry.
- Insert a new lancet into the handle and set the puncture depth.
- Insert a test strip and the device will automatically turn on.
- Place the piercing pen on the side of your fingertip and press the button.
- The appearance of a flashing drop on the screen signals that the device is ready for operation.
- Apply the strip to a drop of blood on your finger and it will be automatically absorbed. After a few seconds, the result will be displayed on the screen.
After removing the test, the device will turn off on its own.
How to choose the right glucometer
You can see many models on the market. Equally high-quality devices differ in the degree of convenience for a particular user. You can understand which glucometer is best to buy for your home by answering a few questions:
- Which type of device is most convenient for you?
- Does the required blood volume matter? For the elderly, children and especially sensitive people, the depth of the puncture is important.
- Is measurement time important? Faster ones cost more, but not everyone needs them.
- What test strips are available in pharmacies near you?
- Is additional plasma calibration required? In simpler devices it is carried out through capillary blood.
- How much memory is needed? This determines how many last measurements can be recorded.
It is important to decide whether additional features are needed. Modern sugar meters can have a lot of them. But their presence is not necessary.
Features and benefits of automatic lancets
Some time ago, a metal “pen” was commonly used to draw blood. The procedure was accompanied by pain and burning, and caused fear in children. Modern automatic lancets, which are much more convenient to use, do not cause pain, ensure safety and make the procedure quick and comfortable. The device is closed with a cap and stored in a special case.
Before use, the cap is unscrewed, the needle extends when you press the button or when it comes into contact with the surface of the dermis. After completing the procedure, the needle is blocked in the body, which prevents the instrument from being reused.
The advantages of automatic lancets include:
- Lack of the human factor - strong or insufficient physical effort, hand trembling.
- Safety for patients - reuse is excluded.
- Ease of use - no special training required.
- Non-hazardous for medical staff - the needle is protected and blocked after drawing blood.
- The devices are very convenient and easy to use. Even children quickly learn how to use the lancet and are able to use them independently.
- Comfort – thin needles with a special sharpening do not cause pain, you can safely use the device for infants, after the puncture there is no irritation on the finger.
- The needles are ready for use and do not require additional processing or sterilization.
There are a large number of companies that produce these products. It is in great demand in medicine. The price of the device is reasonable; anyone can purchase it.
Device coding
This is a procedure on which the accuracy of the results depends. It allows you to bring the device itself and the test strips that come with it into maximum compliance. Older models required manual coding. It was replaced by electronic chips.
The most advanced devices do not require coding. It occurs automatically when the test strip enters the housing. The glucometer reads the code and configures itself.
No Coding technology was developed because it became apparent that most patients were not completing the necessary adjustments. The coding procedure cannot be ignored, as this reduces the accuracy of measurements. As a result, it is not possible to accurately determine the dose of insulin that needs to be administered to the patient.
Restrictions
When purchasing lancets, many people ask whether there are any restrictions on their use and whether one lancet can be used several times. The attached instructions state that:
- Do not use the device if the protective cap is missing or damaged.
- The needle is intended for one-time use only. It is forbidden to use the lancet more than once. For each puncture, you must use a new sterile needle.
- The device is intended for individual use only.
- To ensure the safety of infection, disposal is carried out with the cap tightly latched, observing safety precautions.
- Keep out of the reach of children.
Please remember that the device cannot be used after the expiration date.
Rating of the best devices
A high-quality glucometer can only be purchased at a pharmacy or medical equipment store that has the appropriate license. There are numerous manufacturers on the market that receive positive reviews. Their ranking is as follows:
| Manufacturer | Popular models |
| Accu-Chek (Germany) |
|
| OneTouch (Switzerland) |
|
| Bayer (Germany) |
|
| Diamedical (Taiwan) |
|
| Bioptik (Taiwan) |
|
| 77 Elektronika Kft (Hungary) |
|
| iHealth (USA) |
|
| CareSens (South Korea) |
|
| Satellite (Russia) |
|
| AgaMatrix (Germany) |
|
Tokareva Lyudmila Georgievna, therapist, medical offices 36.6
THERE ARE CONTRAINDICATIONS, BEFORE USE YOU MUST CONSULT WITH A SPECIALIST
How often should lancets be changed?
All needles are automatic and universal; it is recommended in all instructions for the glucometer to use them only once and then change them. Lancets are sterile, but after blood collection they lose this property. To avoid serious consequences, it is necessary to replace the lancet after use.
For this:
- Automatic needles are equipped with additional protection that prevents the patient from reusing them. Therefore, they are considered reliable and safe. It only takes a few seconds to draw blood. And you already know how to use a lancet.
- In the case of universal needles, this option is not available. Many diabetics who need to draw blood more than once a day use the devices repeatedly to save money. But they take risks and violate the instructions.
In addition, each time the needle becomes dull, the puncture becomes more painful. And in the area of damage to the skin, inflammation may begin.
Popular models
The modern pharmaceutical market offers a wide selection of devices that facilitate blood collection from children and adults. Let's consider several popular models.
Acti-lance
This is a scarifier lancet designed for one-time blood collection. This model is designed specifically for collecting biological material with a minimal level of skin trauma in patients who are forced to perform the procedure every day.
Acti-lance is one of the popular companies
The dermis is punctured with this device at the optimal distance between the pencil and the skin, which makes the session absolutely painless. When used at home or in clinics, the patient does not have to worry about his health, since the scarifier is used once.
Prolance Low Flow
Allows you to quickly and painlessly take blood for analysis. The mechanism is equipped with a double spring, which ensures quick piercing of the dermis with minimal pain. The design is made taking into account all the features of the procedure, which makes the lancet convenient to use.
The protective mechanism with which the scarifier is equipped prevents its reuse, which makes it safe in case of accidental repeated contact with the patient’s skin.
Apexlab
A universal device produced by a Chinese company. It is intended for collecting blood from newborns and patients aged up to 1.5 years. The lancet does not cause pain, the wound heals quickly. Its advantages include ease of use, safety, painlessness, and provision of psychological comfort to the child.
The mechanism has a needle lock after use and is equipped with needles sharpened on all sides, which does not cause physical or psychological discomfort when pierced.